Horner syndrome (HS), first described in humans in 1869 and in animals in 1852, is a possible complication associated with different techniques for controlling regional postoperative pain (intradural, epidural, or brachial plexus), with an incidence below 1.8%. We present a case of HS associated with the use of a thoracic paravertebral catheter to control postoperative pain after pulmonary resection by thoracotomy.
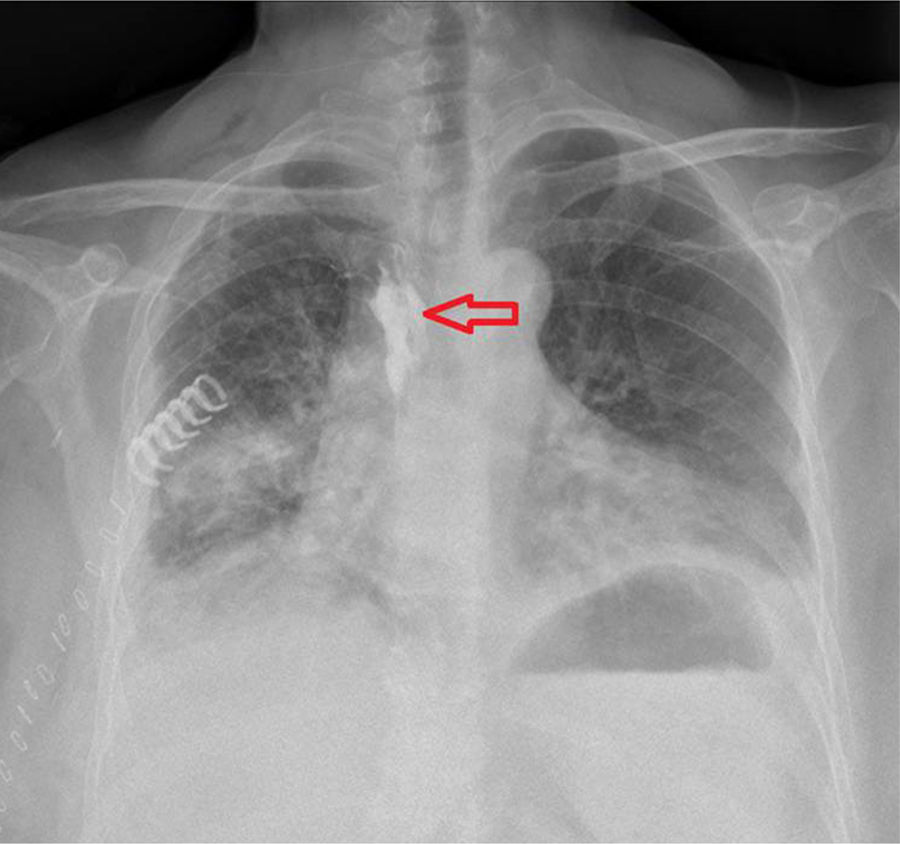
Our patient was a 58-year-old female smoker with drug-controlled arterial hypertension and insulin-dependent diabetes mellitus, receiving treatment with immunosuppressants to treat rheumatoid arthritis. She presented symptoms of diarrhoea and asthenia. A chest radiography revealed pulmonary consolidation in the middle lobe, which was diagnosed as pulmonary adenocarcinoma (clinical stage IA) after a CT-guided transthoracic needle biopsy. In the anaesthetic induction phase, a paravertebral catheter was placed to control postoperative pain, which had to be removed due to extravasation of blood through the device. During the procedure, we observed a haematoma fully dissecting the paravertebral space and a second paravertebral catheter was inserted (at the level of the fifth intercostal space, advancing cranially to the third). We started continuous perfusion of bupivacaine 0.25% at 5mL per hour for 24hours following the procedure. During the clinical progression in the inpatient ward, we observed ptosis with non-reactive pupil which forced us to stop perfusion of local anaesthetic; these symptoms resolved fully in the following hour. We performed a chest radiography with a 5mL bolus of iodinated contrast agent to verify that the paravertebral catheter was correctly placed (Fig. 1).1 Six hours later, a single 5mL bolus of bupivacaine 0.25% was instilled and symptoms reappeared, prompting the definitive discontinuation of the treatment. During the hospital stay, we observed no changes in cardiac rate, nor other accompanying neurological alterations.
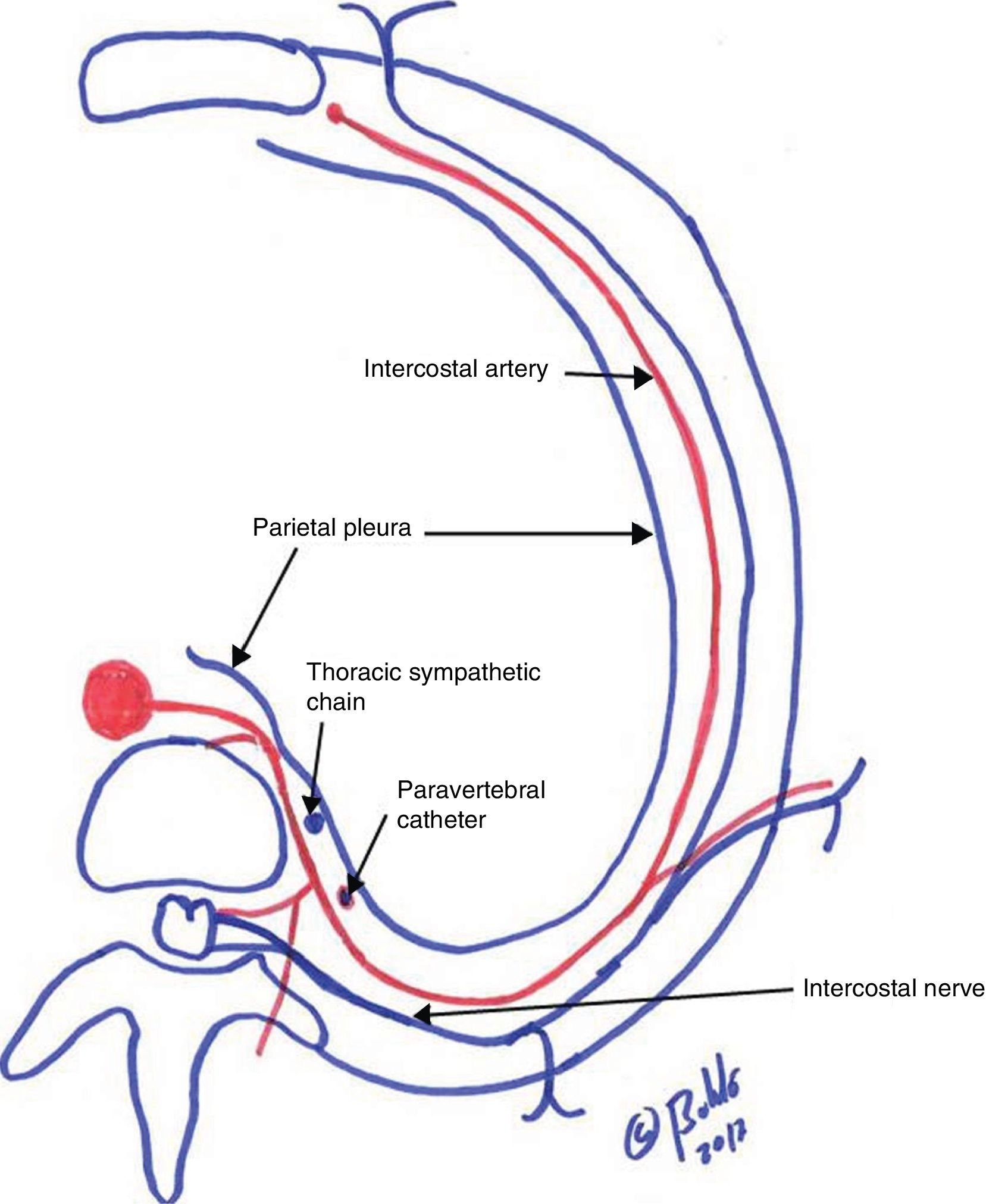
Administration of local anaesthetic in the thoracic paravertebral space (including fat, the spinal intercostal nerves, communicating branches, and in the anterior portion, the sympathetic chain) (Fig. 2) may lead to diffusion of the drug to the cervical sympathetic chain, resulting in myosis due to blocking of the pupil dilator muscle; these symptoms are isolated, transient, and usually disappear with no sequelae within hours of local anaesthetic administration.2 Exceptionally, HS may be accompanied by blockade of preganglionic sympathetic B-fibres3 at the level of C4 and C5, with alterations in cardiac rate and cardiac contractile strength, or be associated with decreased motility of the corresponding hemidiaphragm due to the adjacent blocking of the phrenic nerve.4
The thoracic paravertebral catheter is an effective mechanism of pain control5 in patients who have undergone thoracotomy, whether for pulmonary neoplasm resection or for any other pulmonary disease requiring the chest cavity to be opened.
Our patient showed cephalic paravertebral migration of a local anaesthetic reaching 5-8 dermatomes, facilitated by the paravertebral haematoma, with involvement of the stellate ganglion leading to HS, but with no other clinical or haemodynamic consequences.
The presence of HS during the postoperative period after insertion of a paravertebral rather than an epidural catheter suggests blocking of sympathetic fibres at a higher thoracic level, which may be accompanied by severe neurological and cardiorespiratory manifestations. Under these circumstances, we should suspend administration of the local anaesthetic through the catheter and closely monitor the patient during the following 24-48hours.
Please cite this article as: Rodríguez Gómez CM, Rubio Garay M, Baldó Padró X, Sebastián Quetglás F. Síndrome de Horner por migración paravertebral cefálica del anestésico local. Neurología. 2020;35:126–128.