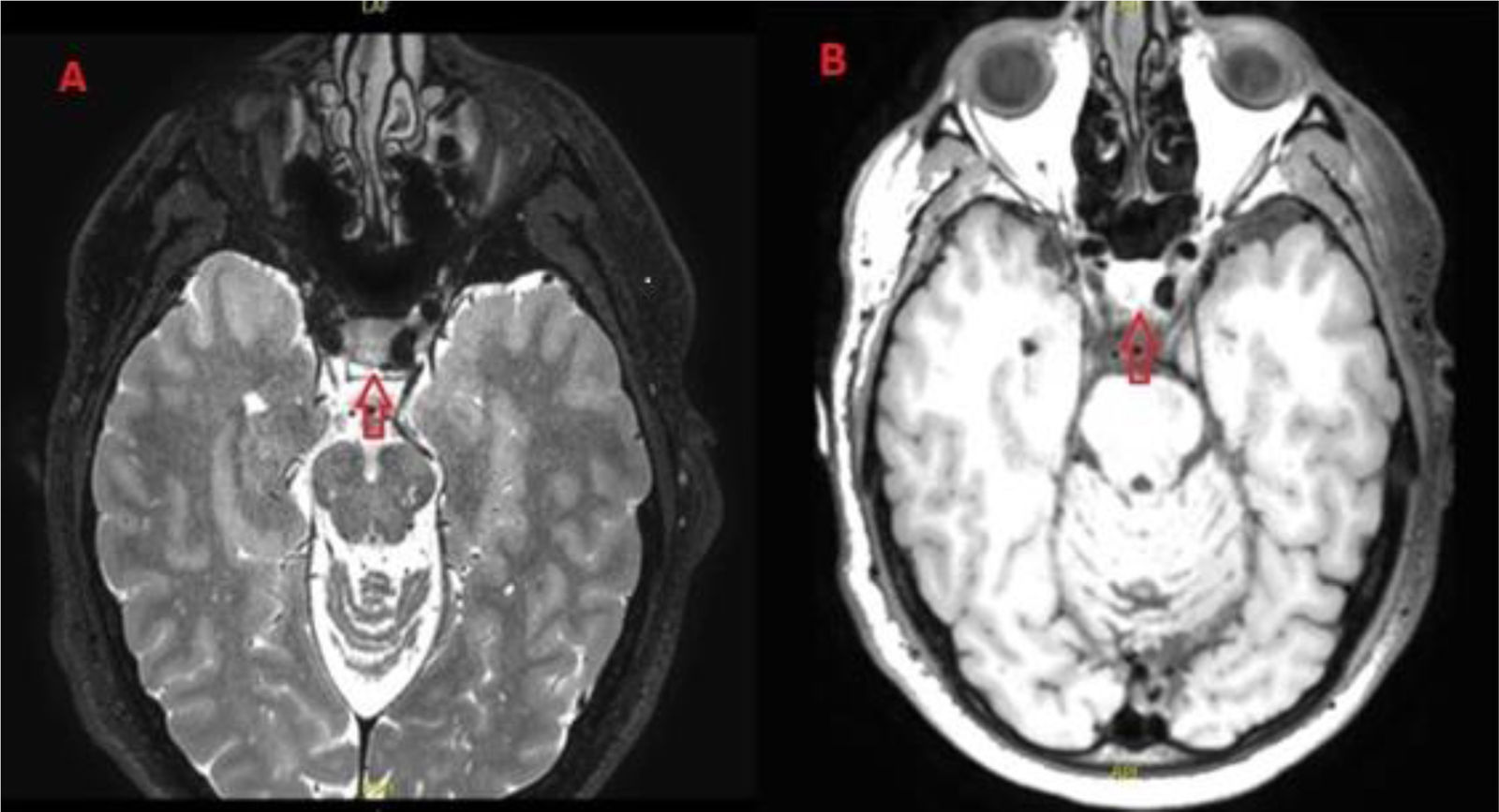
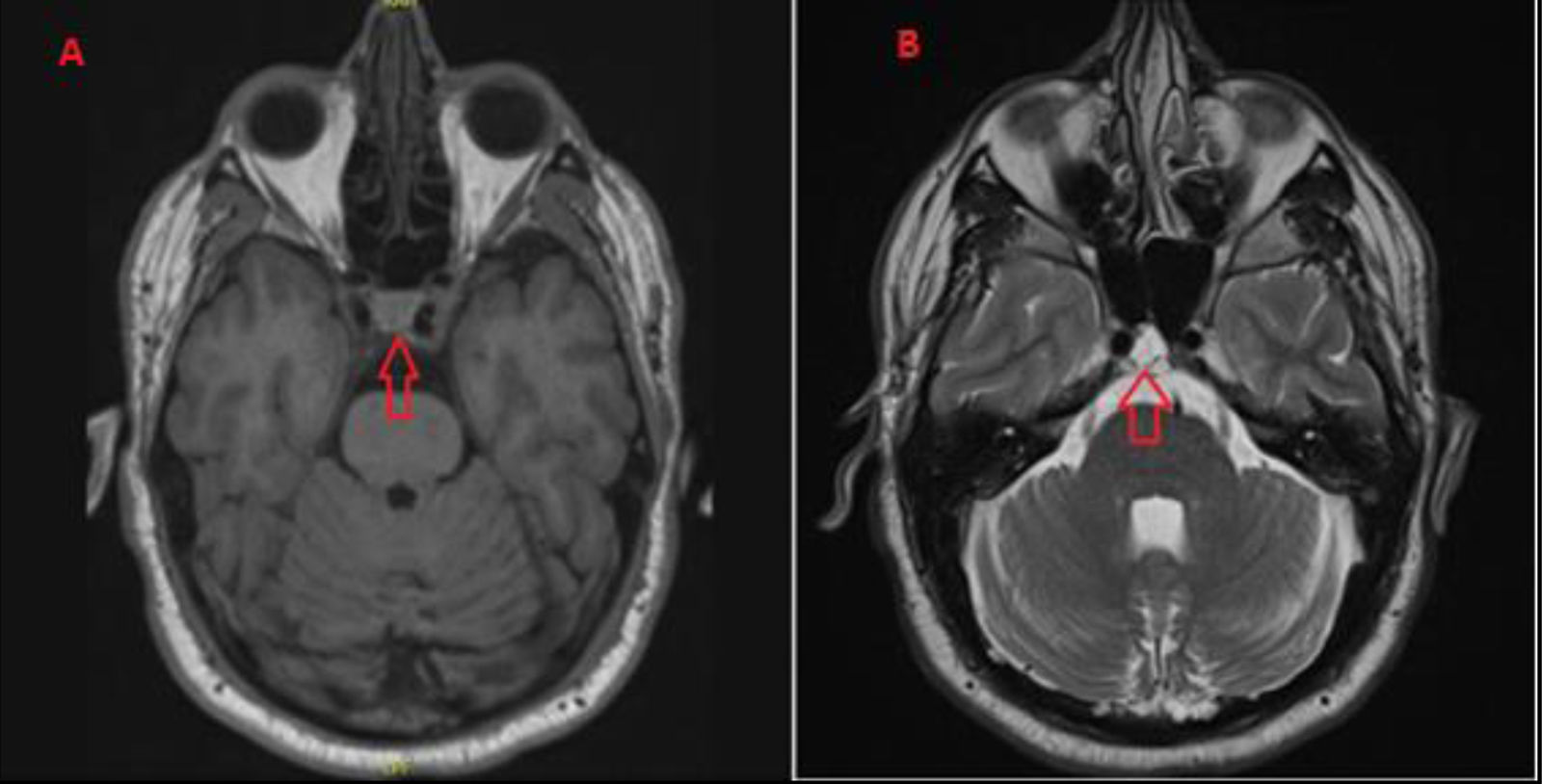
We present the case of a 45-year-old man with history of hypertension and no history of migraine or any other type of episodic headache, who was admitted to our department due to pain in the back of the head, responding to anti-inflammatory drugs, together with binocular diplopia consistent with right fourth cranial nerve neuropathy. He did not present fever or symptoms compatible with intracranial hypertension. Our assessment included a lumbar puncture, CT angiography, and blood analysis with autoimmunity study, yielding no relevant findings. A brain MRI study revealed a 10 × 17 mm cystic lesion on the dorsal surface of the clivus, located at the cisternal segment of the right fourth cranial nerve, which was diagnosed as a possible mucous retention cyst or sphenoid sinus mucocele. Symptoms resolved within days, without treatment. The patient was lost to follow-up. Thirteen years later, he presented the same symptoms, which once more resolved spontaneously, for which he did not seek medical help. He experienced a third episode 14 years after the initial episode. Unlike in the previous events, symptoms did not resolve spontaneously; therefore, treatment with prednisone was started, achieving a favourable therapeutic response with symptoms fully resolving. After this latter episode, an MRI study revealed a lesion on the dorsal surface of the clivus, which was compatible with ecchordosis physaliphora (Fig. 1). To date, he has experienced no further episodes. A third follow-up MRI study performed 4 years after the last episode revealed no changes (Fig. 2).
Ecchordosis physaliphora is a congenital benign hamartomatous lesion originating from notochord remnants, which is detected in up to 2% of autopsy studies.1 It is most frequently located in the retroclival prepontine region or middle cranial fossa; however, it may be found anywhere between the base of the skull and the sacrum.2 Differential diagnosis with chordoma is important, although some authors consider the 2 entities to be varieties of the same pathology.1 Its histological diagnosis is usually difficult,2 with neuroimaging findings being essential. In MRI studies, ecchordosis physaliphora typically appears hypointense on T1-weighted and hyperintense on T2-weighted sequences, with no contrast uptake or associated bone destruction, whereas chordoma usually manifests with contrast uptake and associated bone destruction.2 In cases in which MRI is subsequently performed, no increase in the size of lesions compatible with ecchordosis physaliphora has been observed.2 The majority of cases are identified incidentally in asymptomatic individuals.3 The few symptomatic cases reported to date present with headache, rhinorrhoea due to CSF leaks, or binocular diplopia,3 which is usually secondary to compression of the sixth cranial nerve in the Dorello canal at the petrous apex, before it reaches the cavernous sinus.4 The explanation for a radiologically stable lesion causing intermittent clinical symptoms may be transient inflammation. In cases of very disabling symptomatic lesions, endoscopic endonasal transsphenoidal surgery is performed.5 The corticosteroid treatment used in our patient has previously been reported in the literature in a single case; its therapeutic effect is believed to be mediated by a decrease in a possible inflammatory component, thereby reducing the compression on the fourth cranial nerve.4
In conclusion, ecchordosis physaliphora consists of notochord remnants that are asymptomatic in the majority of cases,3 but may cause headache, rhinorrhoea, or diplopia due to fourth cranial nerve palsy.4 Disabling symptoms are typically treated with endoscopic transsphenoidal resection.5 The use of corticosteroids may represent a therapeutic alternative.4
Ethical standardsOur study complies with ethical standards, preserving confidentiality of patient data. We have only included clinical data and excluded personal data or patient photographs.
Submission declarationAll authors declare that the manuscript has not previously been published elsewhere (in Spanish or any other language).
FundingThis work has received no funding of any kind, from any company or business.
The authors have no conflicts of interest to declare.
We would like to thank the staff of the Department of Neurology of Hospital Universitario de Cruces for their collaboration.