This study aims to determine which factors are associated with delays in door-to needle (DTN) time in our hospital. This will help us design future strategies to shorten time to treatment with intravenous thrombolysis (IVT).
MethodsRetrospective analysis of a prospective cohort of patients with ischaemic stroke treated with IVT in our hospital between 2009 and 2012. We analysed the relationship between DTN time and the following variables: age, sex, personal medical history, onset-to-door time, pre-hospital stroke code activation, blood pressure and blood glucose level, National Institutes of Health Stroke Scale (NIHSS), computed tomography angiography (CTA) and/or doppler/duplex ultrasound (DUS) performed before IVT, time to hospital arrival, and day of the week and year of stroke.
ResultsOur hospital treated 239 patients. Median time to treatment in minutes (IQR): onset-to-door, 84 (60–120); door-to-CT, 17 (13–24.75); CT-to needle, 34 (26–47); door-to-needle, 52 (43–70); onset-to-needle, 145 (120–180). Door-to-needle time was significantly shorter when code stroke was activated, at 51 vs. 72min (P=0.008), and longer when CTA was performed, at 59 vs. 48.5min (P=0.004); it was also longer with an onset-to-door time <90min, at 58 vs. 48min (P=0.003). The multivariate linear regression analysis detected 2 factors affecting DTN: code stroke activation (26.3% reduction; P<0.001) and onset-to-door time (every 30min of onset-to-door delay corresponded to a 4.7min increase in DTN time [P=0.02]). On the other hand, CTA resulted in a 13.4% increase in DTN (P=0.03). No other factors had a significant influence on door-to-needle time.
ConclusionsThis study enabled us to identify CTA and the “3-hour effect” as the 2 factors that delay IVT in our hospital. In contrast, activating code stroke clearly reduces DTN. This information will be useful in our future attempts to reduce door-to-needle times.
Identificar los factores que influyen en el tiempo puerta-aguja (tiempo P-A) en la administración de trombólisis intravenosa (TIV) en un hospital terciario para diseñar futuras estrategias que acorten los tiempos.
MétodosEstudio retrospectivo de pacientes tratados con TIV entre 2009 y 2012. Analizamos la relación entre el tiempo P-A y los siguientes factores: edad, sexo, antecedentes personales, tiempo inicio-puerta, activación de código ictus extrahospitalario (CIE), glucemia y presión arterial basal, NIHSS basal, realización de angio-TC o estudio neurosonológico previo, hora de llegada al hospital, día de la semana y año del ictus.
ResultadosHubo un total de 239 pacientes tratados. Tiempos de actuación en min (mediana [rango intercuartílico]): tiempo inicio-puerta 84 (60-120); tiempo puerta-TC 17 (13-24,75) tiempo TC-aguja 34 (26-47); tiempo puerta-aguja 52 (43-70); tiempo inicio-aguja 145 (120-180). El tiempo P-A fue significativamente menor con la activación del CIE: 51 vs. 72 (p=0,008), y mayor con la realización de angio-TC: 59 vs. 48,5 (p=0,004) y con tiempo inicio-puerta <90min: 58 vs. 48 (p=0,003). En el análisis de regresión lineal múltiple 2 factores redujeron significativamente el tiempo P-A: la activación de CIE (reducción=26,3%; p<0,001) y el tiempo inicio-puerta (por cada 30min de tiempo inicio-puerta, el tiempo P-A se acortó 4,7min; p=0,02). Por el contrario realizar una angio-TC aumentó un 13,4% el tiempo P-A (p=0,03). Los demás factores no influyeron significativamente en el tiempo P-A.
ConclusionesLa realización de angio-TC y el «efecto de las 3h» son 2 factores que retrasan el inicio de la TIV en nuestro hospital. Por el contrario el CIE reduce claramente los tiempos P-A. Los resultados de este estudio nos han permitido identificar qué factores retrasan nuestra actuación y servirán en un futuro para intentar disminuir los tiempos P-A en nuestro hospital.
Clinical trials have shown that early administration of intravenous thrombolysis (IVT) with recombinant tissue plasminogen activator (rt-PA) for acute ischaemic stroke results in better outcomes than a placebo.1,2
The established therapeutic window for this drug is 4.5hours2; however, the effectiveness of this treatment is time-dependent and decreases as time from symptom onset to treatment administration increases (onset-to-needle time, OTN time). Researchers have shown that the number needed to treat to obtain an optimal functional outcome (scores on the modified Rankin Scale of 0 to 1) increases by 1 for every 20minutes elapsed from symptom onset to treatment administration.3 Therefore, thrombolytic treatment should be administered as early as possible avoiding unnecessary delays. Every minute may be decisive for the patient's functional outcome, as we gather from the aphorism ‘time is brain’.4
The time elapsed between the patient's arrival at the hospital and receiving IVT (door-to-needle time [DTN time]) depends directly on each hospital's specialists and set protocols. According to the latest recommendations from the American Heart Association (AHA), DTN time should not exceed 60minutes.5 In the past few years, several studies analysing the reasons for in-hospital delays in IVT administration have been published. We also find results from protocols that have managed to safely and significantly reduce times to well below the recommended 60-minute threshold.5 Healthcare systems currently consider DTN time a quality control parameter for in-hospital care.8 Reducing these times depends not only on a trained, coordinated multidisciplinary team for stroke care, but often on technical and administrative improvements in the hospital as well.
Our aim is to analyse the factors impacting in-hospital delays in IVT administration at our centre. These data could be instrumental in the design of a protocol to reduce DTN times in the future.
Patients and methodsWe conducted a retrospective analysis of a prospective registry of patients treated with IVT between January 2009 and December 2012 in the stroke unit of a tertiary-care hospital in Madrid which provides care to a population of approximately one million inhabitants. In-hospital strokes were excluded.
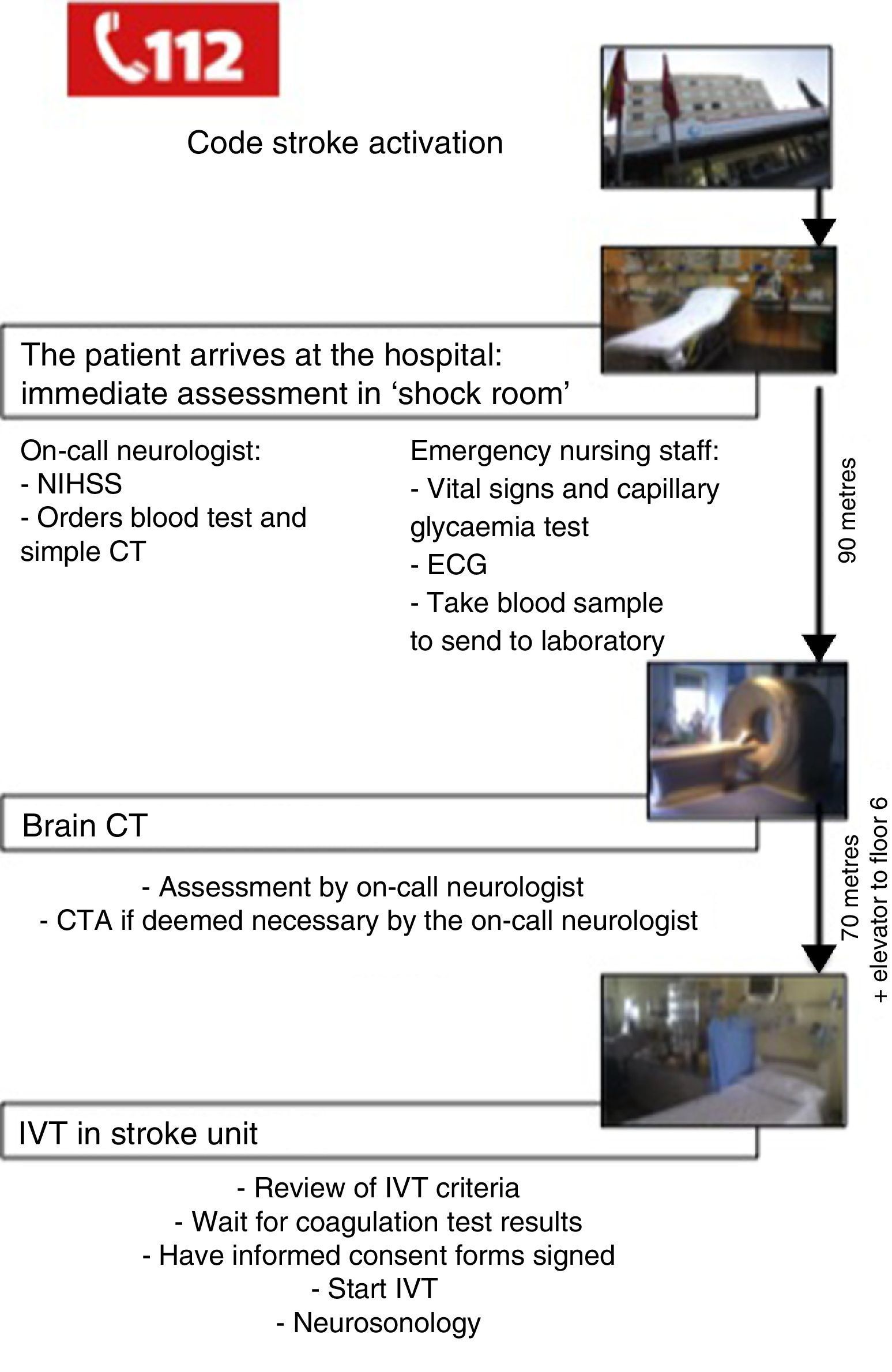
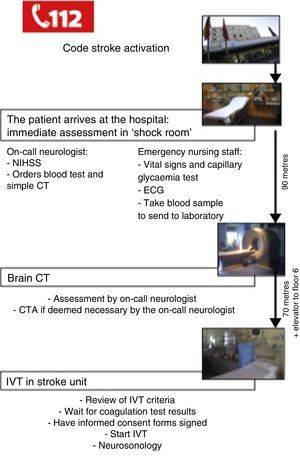
In-hospital action protocol for acute stroke in candidates for IVTThe stroke care plan for the region of Madrid was launched in 2006. It includes a pre-hospital action protocol aimed at identifying patients with suspected stroke to transport them to the hospital as quickly as possible.9
In our hospital, the on-call neurologist receives the call from the emergency services and informs the stroke unit, the vascular neurology team, and the emergency nursing/triage staff to coordinate care before the patient arrives.
Once in the hospital, the patient is immediately assessed in a room equipped with advanced life support equipment and located close to the main entrance; this is known as the ‘shock room’. The emergency nursing staff measures vital signs and performs a capillary glycaemia test, electrocardiography, and extracts a blood sample for analysis. The on-call neurologist assesses the patient's stability, confirms the diagnosis of stroke, determines severity, and calculates the patient's score on the National Institutes of Health Stroke Scale (NIHSS). The team then uses the hospital's computer system to request such pertinent complementary tests as complete blood count and a computed tomography (CT) brain scan.
The monitored patient is then transferred to the emergency radiology service (on the same floor, located 90m from the first assessment room) for the CT brain scan.
The clinical history of the patient is taken using a structured questionnaire.10 The on-call neurologist analyses the CT image. If the findings are unmistakeable, the on-call neurologist does not wait for the radiologist's report. The on-call neurologist will determine if a CT angiography (CTA) is necessary.
Once the study is completed, the patient is transferred to the stroke unit on the sixth floor. In the stroke unit, the neurologist waits for the results of the coagulation test to confirm that the patient fulfils all criteria for IVT as per current guidelines for the treatment of acute ischaemic stroke.11 In all cases, the team obtains anticoagulation test results and the informed consent of the patient before starting treatment. If the patient is unable to give consent (due to aphasia, low level of consciousness, etc.), family members are permitted to do so. If the patients do not have any family members at the hospital, the doctor in charge may act on the patient's behalf.
Once IVT has been started (rt-PA dosed at 0.9mg/kg),12 the patient will undergo a neurosonology study and monitoring with transcranial duplex ultrasound. This test will be used depending on the on-call neurologist's judgement and training in the technique.
Fig. 1 shows the actions taken between the patient's arrival at the hospital and IVT administration according to our current in-hospital protocol.
Variables analysedThe time elapsed from symptom onset to administration of the rt-PA bolus, OTN time was broken down into the following intervals: symptom onset to the patient's arrival to the emergency department, onset-to-door (OTD) time; time from arrival at the emergency department to CT scan, door-to-CT (DCT) time; time from scan to administration of rt-PA bolus, CT-to-needle (CTN) time; time from patient's arrival at the emergency department to administration of rt-PA bolus, door-to-needle (DTN) time.
We analysed the impact of the following factors on DTN time: age; sex; personal history including arterial hypertension, diabetes mellitus, dyslipidaemia, atrial fibrillation, smoking, and previous stroke; OTD time; activation of prehospital code stroke (PCS); baseline glycaemia and arterial pressure; baseline NIHSS; use of CTA or neurosonology study; stroke topography; hospital arrival time; day of the week; and year of stroke.
Statistical analysisWe used SPSS statistical software, version 15.0. Quantitative variables were presented as medians and interquartile ranges (IQR), and as means and standard deviations (SD). To compare medians between 2 groups, we used the Mann-Whitney U test. To compare medians between more than 2 groups, we used the Kruskal-Wallis test. The Pearson correlation coefficient was used to identify the lineal correlation between 2 quantitative variables. We conducted a simple linear regression analysis to identify the variables impacting DTN time. The factors that showed significant results in the univariate analysis were included in the multiple linear regression model. P values≤.05 were considered statistically significant.
ResultsWe included 239 patients treated with IVT in our hospital between January 2009 and December 2012. A total of 38 patients (15.9%) were treated in 2009, 73 (30.5%) in 2010, 65 (27.2%) in 2011, and 63 (26.4%) in 2012. Mean age was 69.24 years (SD, 12.88 years) and most were men (135; 56.5%). Posterior circulation strokes accounted for 6.7% of the total. The median score on the NIHSS scale was 14 points (IQR, 9–18). Action times in minutes were as follows (median; IQR): OTD time (84; 60–120); DCT time (17; 13–24.75); CTN time (34; 24–74); OTN time (145; 120–180); DTN time (52; 43–70). In 64.5% of the patients, DTN time was <60minutes. A total of 180 patients (75.3%) received thrombolytic treatment less than 180minutes after symptom onset, 57 patients (23.8%) were treated between 180 and 270minutes, and 2 (0.8%) were treated after 270minutes. PCS was activated for 88.3% of the patients. A CTA was performed in 34.5% of the cases, and neurosonology study in 27.2%. Of the patients, 49.8% were treated during normal working hours (8.00–15.00), 28.3% between 15.00 and 22.00, and the remaining 21.8%, between 22.00 and 8.00; 20.9% of the patients were treated on weekends or holidays.
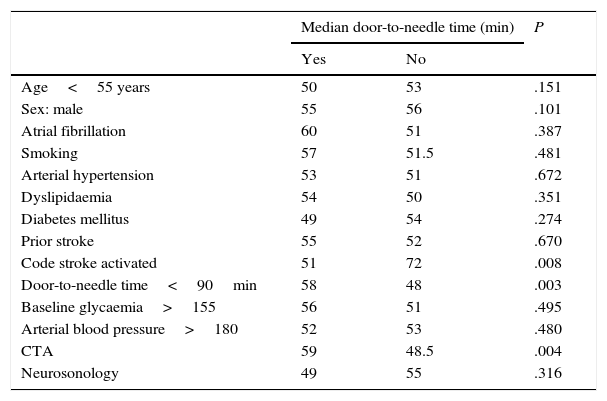
Median DTN time in minutes with PCS activation was 51minutes, vs 72 without code stroke activation (P=.008). In the group of patients who underwent CTA, mean DTN time was 59minutes; in those who did not undergo that test, mean DTN time was lower (48.5min; P=.004). Median CTN time in the patient group with CTA was 37minutes, vs 31minutes in the group without CTA (P=.001). However, performing CTA did not alter DCT times (17.5 vs 17min; P=.97). Patients assessed with CTA before undergoing IVT were younger (median age 68.5 vs 75 years; P=.002). Patients with an OTD time of less than 90minutes had significantly longer in-hospital response times (58min) than patients with OTD times in excess of 90minutes (48min; P=.003). Stroke severity as measured on the NIHSS (P=.752) did not have an impact on DTN time. Time of hospital arrival times (P=.652) and being treated on weekends or holidays did not affect DTN times. There was no linear correlation between age and DTN time (Pearson: 0.004; P=.948). Median DTN time was 50minutes in men vs. 55 in women (P=.101). The remaining factors included in Table 1 had no significant effect on DTN time.
Factors associated with median door-to-needle time.
| Median door-to-needle time (min) | P | ||
|---|---|---|---|
| Yes | No | ||
| Age<55 years | 50 | 53 | .151 |
| Sex: male | 55 | 56 | .101 |
| Atrial fibrillation | 60 | 51 | .387 |
| Smoking | 57 | 51.5 | .481 |
| Arterial hypertension | 53 | 51 | .672 |
| Dyslipidaemia | 54 | 50 | .351 |
| Diabetes mellitus | 49 | 54 | .274 |
| Prior stroke | 55 | 52 | .670 |
| Code stroke activated | 51 | 72 | .008 |
| Door-to-needle time<90min | 58 | 48 | .003 |
| Baseline glycaemia>155 | 56 | 51 | .495 |
| Arterial blood pressure>180 | 52 | 53 | .480 |
| CTA | 59 | 48.5 | .004 |
| Neurosonology | 49 | 55 | .316 |
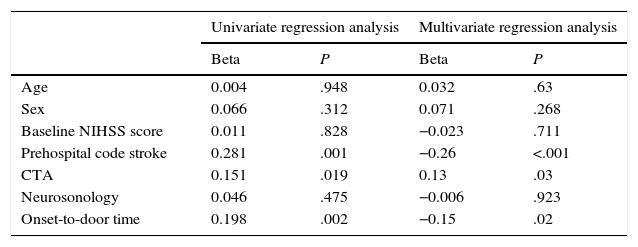
In the univariate linear regression analysis, 3 factors significantly affected DTN time: performing CTA (P=.02), activating PCS (P<.001), and OTD time (P=.002).
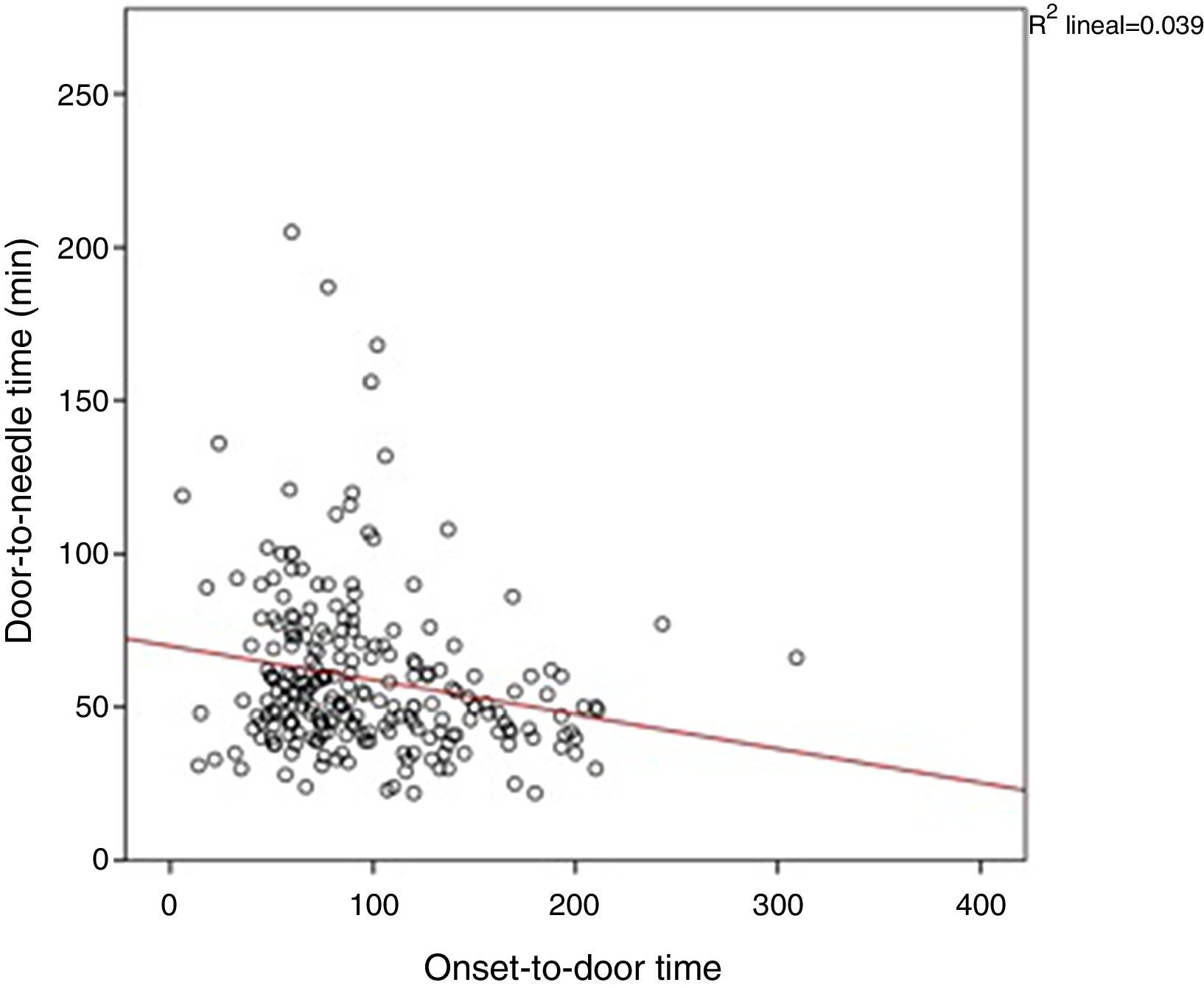
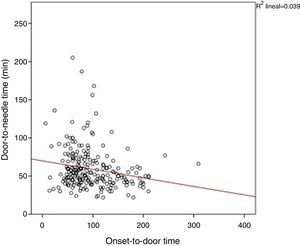
Two factors in the multivariate linear regression model significantly reduced DTN time: activation of PCS (decrease of 26.3% in DTN time; P<.001), and OTD time (for every 30min of OTD time, DTN time decreases by 4.7min; P=.02) (Fig. 2). OTD time had an impact on the CTN time (P=.008) but not on DCT time (P=.537). In contrast, performing CTA before IVT increased DTN time by 13.4% (P=.03) (Table 2).
Results from univariate and multivariate analysis. In the multivariate regression analysis, stroke code activation reduced DTN time by 26% (P<.001). Performing a CT angiography increased DTN time by 13.4% (P=.03). For every 30minutes of OTD time, DTN time lessens by 4.5minutes (P=.02).
| Univariate regression analysis | Multivariate regression analysis | |||
|---|---|---|---|---|
| Beta | P | Beta | P | |
| Age | 0.004 | .948 | 0.032 | .63 |
| Sex | 0.066 | .312 | 0.071 | .268 |
| Baseline NIHSS score | 0.011 | .828 | −0.023 | .711 |
| Prehospital code stroke | 0.281 | .001 | −0.26 | <.001 |
| CTA | 0.151 | .019 | 0.13 | .03 |
| Neurosonology | 0.046 | .475 | −0.006 | .923 |
| Onset-to-door time | 0.198 | .002 | −0.15 | .02 |
Prompt administration of rt-PA after ischaemic stroke has been shown to improve patients’ outcomes.3 To optimise IVT benefits, we must direct all efforts towards reducing or even eliminating treatment delays. Campaigns to raise awarness and more rapid response by emergency services have improved pre-hospital response times13; however, vital time is often wasted due to organisational problems within the hospital.14
In our study, activating the PCS significantly reduced DTN time. Similar results were observed in previous studies.9,15–17 Activation of the PCS helps the neurologist prepare for the patient's arrival. This is therefore a key strategy for reducing in-hospital delays: do all you can before the patient arrives so as to complete the fewest tasks in the shortest time possible once the patient is on site.7
Another factor affecting DTN time was OTD time. The longer the symptom progression time, the shorter the DTN time. This inverse relationship between OTD time and DTN time is known as the ‘three-hour effect’ and it has already been described in the literature.18,19 This is associated with the emergency level perceived by clinicians, meaning that patients with shorter symptom progression times, and thus more time to receive IVT, are treated with less urgency. In our series, the three-hour effect significantly interfered with CTN time, but not with DCT time. This finding does not seem to have been reported by previous studies. Proposed actions to eliminate the three-hour effect include constant review of DTN times by the stroke care team, exchange of feedback among doctors responsible for inhospital care of acute stroke patients, and better adherence to treatment guidelines.19
Performing a CTA before IVT increased DTN time significantly in our study. Previous studies have shown similar results.6,7,20 Using advanced neuroimaging techniques, such as CTA or perfusion CT, may be useful in identifying candidates for recanalisation therapies other than IVT, such as mechanical thrombectomy or intra-arterial thrombolysis. These tests can also extend the therapeutic window for IVT beyond 4.5hours and increase the number of patients treated with rt-PA.21 However, AHA guidelines state that advanced neuroimaging scans are not essential for performing IVT in patients with stroke with a progression time of less than 4.5hours, and that simple CT provides enough diagnostic information for this group of patients.12
The hospital protocols with the shortest response times only call for advanced neuroimaging scans before IVT in cases with an uncertain diagnosis. At the Helsinki hospital, which currently has a median DTN time of 20min, an analysis of 1860 patients showed that performing advanced neuroimaging scans doubles in-hospital response times. This protocol does not seem to increase diagnostic errors since stroke mimics accounted for only 1.4% of the total cases.6 In our series, since the decision to perform a CTA depended on the on-call neurologist, it is difficult to establish the precise reason for performing the test in all cases. CTA was probably assigned to patients with diagnostic uncertainty or used in more complex cases, but it may also have been performed in cases in which it was not strictly necessary, for the sole purpose of gathering more data before IVT.
The largest portion of the DTN time corresponded to the CTN interval. The three-hour effect and performing a CTA significantly impacted CTN time, but not DTN time. Other factors may have impacted CTN time, for example, waiting for results from the coagulation tests taken by all patients. This wait came to about 30minutes at the Helsinki hospital,6 which is comparable to the estimated delay at our hospital. Furthermore, delivering the bolus in the stroke unit, located on the sixth floor, may also have contributed to longer CTN times. Obtaining informed consent before starting treatment may also lead to delay if the patient is unable to sign and doctors must wait for family members to arrive instead. Unfortunately, due to the study design, analysing the effect of these factors on CTN time is not possible. Obtaining an INR Point of Care test to immediately determine the INR value, administering an rt-PA bolus in the radiology room immediately after performing the brain CT, defining criteria for selecting cases needing a CTA, and avoiding delays in obtaining informed consent forms may be effective means of reducing this time interval.
We also analysed if longer treatment delays were recorded during holidays, weekends, and night shifts, since these factors have been associated with increased DTN times in some series.22,23 However, none of them had a significant impact on DTN time in our study.24
Scores on the NIHSS and such demographic factors as age and sex may also impact in-hospital response times. In a recent multicentre analysis carried out in 9 Eastern European countries (SIST-EAST), a DTN time of less than 60minutes was associated with being young or having an NIHSS score indicating moderate to severe stroke (7–24), among other factors.19 The reason for this tendency is that clinicians tend to consider IVT less beneficial for the subgroup of older patients. A low NIHSS score is also perceived as less urgent.19,25 According to the ECASS III study, age and NIHSS score have no impact on the effectiveness of IVT treatment.26 Surprisingly, women and black patients have also been identified as more likely to meet with delays in starting IVT.25 In our study, we observed a tendency towards shorter in-hospital response times among younger patients and men, but this difference did not reach statistical significance. The baseline NIHSS score did not significantly impact DTN times in our series.
The presence of cardiovascular risk factors (arterial hypertension, diabetes mellitus, dyslipidaemia), atrial fibrillation, or previous stroke, provide the neurologist with clues which may facilitate clinical diagnosis of the patient. In some studies, a quicker diagnosis has been associated with shorter in-hospital response times.19,25 In our case, risk factor analysis did not significantly affect response times. Patients arriving with high BP values or glycaemia levels requiring immediate pharmacological treatment also did not show significantly longer DTN times. We did not locate any studies examining these factors.
Our study presents some limitations. Firstly, this is a retrospective study including only patients treated with IVT. The resulting absence of patients who did not receive treatment due to pre-hospitals or in-hospital delays may constitute a selection bias. Secondly, the small sample size may limit the validity of certain results. For example, PCS was activated in a very low number of cases (28 patients, 11.7% of the sample). Lastly, the decision to perform a CTA resided with the on-call neurologist. It is therefore difficult to ascertain whether the delay associated with this test had to do with it being indicated in cases that are more complex or have a less clear diagnosis, or if, on the other hand, the delay was caused by the time needed to complete and interpret the CTA itself.
We conclude that the three-hour effect and use of a CTA both constitute factors delaying IVT at our hospital. In contrast, PCS activation clearly reduces DTN time. The results of this study have helped us identify factors that delay response, and they may also be helpful in the future as we attempt to decrease DTN times at our hospital.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Iglesias Mohedano AM, García Pastor A, García Arratibel A, Sobrino García P, Díaz Otero F, Romero Delgado F, et al. Identificación de los factores que influyen en el retraso intrahospitalario del inicio de trombólisis intravenosa en el ictus agudo en un hospital terciario. Neurología. 2016;31:452–458.