This study explores the applicability of a cognitive stimulation method based on abacus arithmetic in elderly people with and without cognitive impairment.
MethodsThis observational and prospective pilot study was performed in 2 hospitals. The study assessed the applicability of a programme of arithmetic training developed for use in the elderly population. The primary endpoint was an evaluation of the stimulation programme, in terms of usability, satisfaction, and participation in healthy elderly controls and elderly patients with mild cognitive impairment or Alzheimer disease. Secondary endpoints were family satisfaction, caregiver burden, and the behaviour and cognition of patients.
ResultsUsability, satisfaction, and degree of participation were high. The Mini-Mental State Examination showed significant changes (23.1±4.8 before the intervention vs 24.9±4.2 afterwards, P=.002); there were no changes on the Trail Making Test parts A and B, Yesavage Geriatric Depression scale, and Zarit caregiver burden scale.
ConclusionsThe study suggests that cognitive stimulation with abacus arithmetic may be used in elderly people with and without cognitive impairment. Further studies will be needed to evaluate the efficacy of this kind of programmes.
El objetivo del estudio fue evaluar la aplicabilidad de un método de estimulación cognitiva basado en la aritmética mediante el uso del ábaco en población anciana sana y con deterioro cognitivo.
MétodosEstudio observacional, prospectivo, realizado en 2 centros, en que se evaluó la aplicabilidad de una versión desarrollada para población anciana de un programa de estimulación cognitiva aritmética. El objetivo principal del estudio fue valorar la usabilidad, la satisfacción y el cumplimiento del programa de estimulación en población sana, pacientes con deterioro cognitivo leve amnésico y enfermedad de Alzheimer. Asimismo, como objetivos secundarios, se evaluaron la satisfacción del familiar, la sobrecarga del cuidador y la cognición y la conducta de los pacientes.
ResultadosLa usabilidad, la satisfacción y el grado de participación fueron elevados. Se observaron cambios significativos en Mini-mental State Examination (23,1±4,8 antes de la intervención vs. 24,9±4,2 después, p=0,002), mientras que no se observaron diferencias significativas en TMT-A y B, escala de depresión geriátrica de Yesavage y la escala de sobrecarga del cuidador de Zarit.
ConclusionesEl estudio indica que la estimulación cognitiva aritmética mediante ábaco es aplicable a los sujetos ancianos, con y sin deterioro cognitivo. Se necesitan futuros estudios que evalúen la eficacia del tratamiento.
In recent years, the increase in life expectancy has inevitably led to population ageing and a higher prevalence of neurodegenerative diseases associated with cognitive impairment.1 Despite recent advancement of our knowledge of the pathophysiological and molecular basis of these diseases, there is still no curative treatment and the drugs available to date focus on symptoms.2 In this context, emphasis is put on non-pharmacological interventions for patients with dementia, mainly cognitive stimulation therapy.3 According to the cognitive reserve hypothesis, increased cognitive activity may delay the onset of cognitive symptoms even in elderly patients.4,5
Several studies and meta-analyses of cognitive stimulation therapies show overall positive results, reporting improvements in cognitive function, quality of life, and social interaction.6–8
A wide range of cognitive stimulation methods have been proposed. In recent years, an abacus-based training method has been applied to children. This method has been shown to improve learning and development and suggested to promote structural and functional changes in several brain regions.9–12 To our knowledge, no studies have evaluated this method in an elderly population. The purpose of our study was to assess the applicability of a cognitive stimulation method based on abacus arithmetic in healthy and cognitively impaired elderly patients.
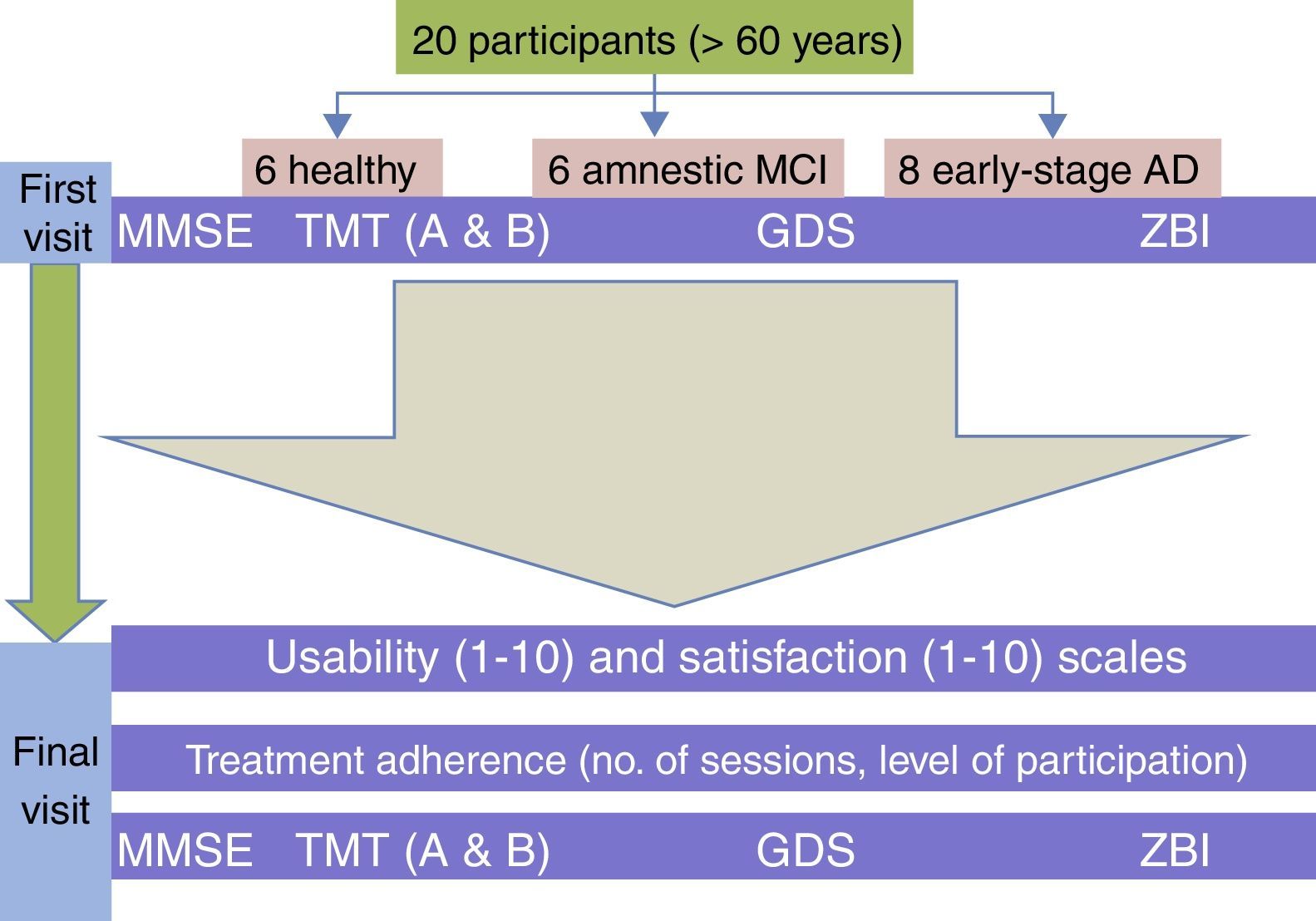
Material and methodsStudy designWe conducted a prospective observational study in 2 centres to analyse the applicability of a version of an arithmetic-based cognitive stimulation method specifically designed for elderly patients. The main purpose of this study was to assess usability, satisfaction, and compliance with a cognitive stimulation programme for healthy and cognitively impaired elderly patients. A second purpose was to evaluate family satisfaction, caregiver burden, and patients’ cognition and behaviour.
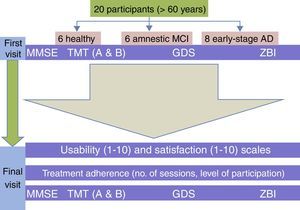
Study populationWe included patients aged over 65 years treated in the neurology department at Hospital Clínico San Carlos, in Madrid, or Hospital Universitario Infanta Cristina, in Parla, Madrid. The sample (n=20) was divided into 3 groups: 1) healthy patients (n=6) with no cognitive complaints or cognitive impairment affecting daily living and scoring>24 on the Mini-Mental State Examination (MMSE); 2) patients with a diagnosis of amnestic mild cognitive impairment (MCI) according to the diagnostic criteria by Petersen et al.13 (n=6); and 3) patients diagnosed with probable early-stage Alzheimer disease (AD) (Global Deterioration Scale=4) according to the NINCDS-ADRDA diagnostic criteria14 (n=8). We excluded all patients with severe behavioural disorders that might have resulted in low participation in the programme, depression (scores>5 on the short version of Yesavage's Geriatric Depression Scale [GDS]), functional illiteracy or a lack of basic mathematical knowledge, or severe systemic disease that might have led to poor compliance. The study was approved by the Clinical Research Ethics Committees of the 2 hospitals. All participants, and the main caregiver in the case of patients with probable AD, signed informed consent forms.
Clinical assessment and outcome variablesBefore starting the cognitive stimulation programme, the included patients were assessed by 2 independent neurologists at an initial consultation. We gathered several demographic and clinical variables. The participants were assessed with the MMSE,15 parts A and B of the Trail Making Test (TMT),16 and the short version of the GDS.17 Likewise, the caregivers of patients with AD were administered the Zarit Burden Interview (ZBI).18
After completing the cognitive stimulation programme, the patients were re-assessed by the same neurologists. Usability and satisfaction were measured with an analogue scale ranging from 1 (minimum score) to 10 (maximum score). Usability was evaluated with the question ‘Did you find it easy to complete the stimulation programme? Score the degree of difficulty in attending sessions on a scale from 1 to 10’. Satisfaction was assessed with the question ‘What is your level of satisfaction with the method BrainFactory +50?’. This question was asked to healthy patients, patients with MCI, and caregivers of patients with AD. We re-administered the MMSE, parts A and B of the TMT, the GDS, and the ZBI (Fig. 1). The therapists made a record of the number of sessions each patient attended and scored the level of participation and cooperation with the method from 1 (lowest) to 10 (highest). The therapists were unaware of each patient's diagnosis and blind to their scores on the cognitive and behavioural assessment tests mentioned previously.
Cognitive stimulation programmeWe used a version for patients aged over 60 of the BrainFactory +50 method, which is based on the ALOHA Mental Arithmetic method for children.19,20 The ALOHA Mental Arithmetic method is a mental development programme designed for children aged 5 to 13 aimed at improving children's intelligence by using an educational programme based on 3 fundamental pillars: the abacus, mental arithmetic, and educational games. Its recreational and interactive nature is one of the strengths of this programme. Children learn while they have fun thanks to an educational methodology that places a strong emphasis on games. The developers of this programme designed another version for healthy and cognitively impaired elderly patients (>60 years) using part of the original materials and the same educational and interactive methodology. This method is based on performing calculations using a Japanese abacus and includes tasks that promote attention, concentration, spatial orientation, problem analysis and resolution, visual memory, spatial thinking, and visuomotor and visuospatial skills. Subjects must solve a series of exercises of increasing difficulty using the abacus.
Our participants took 10 sessions lasting 150 minutes each for 5 weeks (2 sessions per week). They were divided into 2 groups of 10 people each; each group was led by 2 therapists. Both groups included participants from the 3 diagnostic groups. Each session included approximately 60 minutes of abacus-based calculations, 10 minutes of mental arithmetic, 45 minutes of other cognitive tasks, and 35 minutes of relaxation and/or concentration exercises. The programme included both individual and group tasks.
Statistical analysisStatistical analysis was performed with IBM SPSS Statistics version 20.0. Baseline and follow-up clinical characteristics were expressed as means±SD. We used non-parametric tests for hypothesis testing. More specifically, we used the Kruskal–Wallis test to compare quantitative variables between the 3 groups, and the Wilcoxon test to analyse pre-intervention and post-intervention cognitive test scores. Statistical significance was set at P<.05.
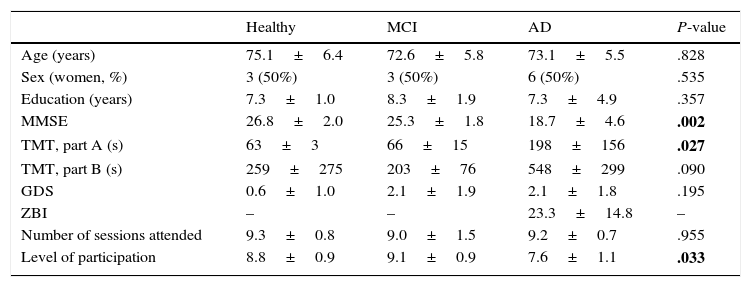
ResultsWe included 20 patients aged 73.6±5.6 and with 7.6±3.2 years of schooling; 12 were women (60%). The main demographic and clinical characteristics of each group are listed in Table 1.
Demographic and clinical characteristics of the study groups.
| Healthy | MCI | AD | P-value | |
|---|---|---|---|---|
| Age (years) | 75.1±6.4 | 72.6±5.8 | 73.1±5.5 | .828 |
| Sex (women, %) | 3 (50%) | 3 (50%) | 6 (50%) | .535 |
| Education (years) | 7.3±1.0 | 8.3±1.9 | 7.3±4.9 | .357 |
| MMSE | 26.8±2.0 | 25.3±1.8 | 18.7±4.6 | .002 |
| TMT, part A (s) | 63±3 | 66±15 | 198±156 | .027 |
| TMT, part B (s) | 259±275 | 203±76 | 548±299 | .090 |
| GDS | 0.6±1.0 | 2.1±1.9 | 2.1±1.8 | .195 |
| ZBI | – | – | 23.3±14.8 | – |
| Number of sessions attended | 9.3±0.8 | 9.0±1.5 | 9.2±0.7 | .955 |
| Level of participation | 8.8±0.9 | 9.1±0.9 | 7.6±1.1 | .033 |
Bold values indicate statistical significance was set at P<.05.
Usability was scored 8.4±1.27 and satisfaction obtained 9.4±0.68. Patients attended to a mean of 9.2±1.0 sessions and the level of participation was 8.4±1.19.
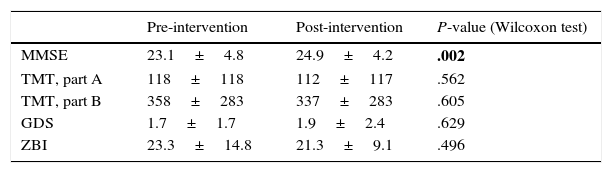
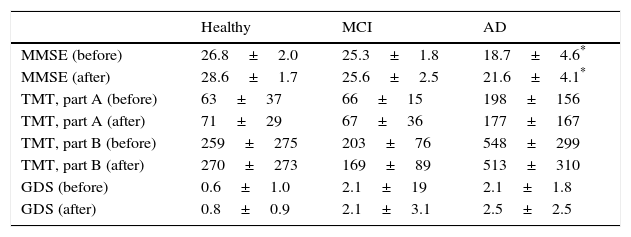
Regarding pre- and post-intervention scores, we found statistically significant differences in MMSE scores (23.1±4.8 vs 24.9±4.2, P=.002), but no significant differences were seen in parts A and B of the TMT, the GDS, or the ZBI (Table 2). We also found statistically significant differences between pre- and post-intervention MMSE scores when analysing patients with MCI or AD separately (21.5±4.9 vs 23.35±3.99, P=.01) (Table 3). Post-intervention assessments were conducted 24±36 days after completing the cognitive stimulation programme.
Variables assessing cognition, behaviour, and caregiver burden before and after the intervention.
| Pre-intervention | Post-intervention | P-value (Wilcoxon test) | |
|---|---|---|---|
| MMSE | 23.1±4.8 | 24.9±4.2 | .002 |
| TMT, part A | 118±118 | 112±117 | .562 |
| TMT, part B | 358±283 | 337±283 | .605 |
| GDS | 1.7±1.7 | 1.9±2.4 | .629 |
| ZBI | 23.3±14.8 | 21.3±9.1 | .496 |
Bold values indicate statistical significance was set at P<.05.
Cognitive and behavioural variables before and after the intervention, by diagnostic group.
| Healthy | MCI | AD | |
|---|---|---|---|
| MMSE (before) | 26.8±2.0 | 25.3±1.8 | 18.7±4.6* |
| MMSE (after) | 28.6±1.7 | 25.6±2.5 | 21.6±4.1* |
| TMT, part A (before) | 63±37 | 66±15 | 198±156 |
| TMT, part A (after) | 71±29 | 67±36 | 177±167 |
| TMT, part B (before) | 259±275 | 203±76 | 548±299 |
| TMT, part B (after) | 270±273 | 169±89 | 513±310 |
| GDS (before) | 0.6±1.0 | 2.1±19 | 2.1±1.8 |
| GDS (after) | 0.8±0.9 | 2.1±3.1 | 2.5±2.5 |
The purpose of this study was to analyse the applicability of a cognitive stimulation method using abacus arithmetic in patients over 65. Our results show a high level of satisfaction with and usability of the method in both healthy patients and patients with MCI or AD. The levels of participation and attendance to sessions were also high. Our findings suggest that this method is applicable to elderly patients.
In addition, the participants were found to score higher on the MMSE after the intervention. We hypothesise that arithmetic-based cognitive stimulation may improve overall cognitive function. However, we found no significant changes in the scores of the tests assessing visual scanning and psychomotor speed (TMT, part A) and selective attention (TMT, part B), depression (GDS), or caregiver burden (ZBI). Comparative studies including a control group are necessary to evaluate the effectiveness of cognitive stimulation. Likewise, further studies should include longer intervention and follow-up periods in order to assess the potential long-term effects of this method.
Arithmetic-based cognitive stimulation methods have been infrequently used in Western countries (Europe and America). Some studies developed in Japan report improved cognitive function in patients with dementia; these improvements lasted up to 6 months after the intervention.21,22 These findings suggest that the positive effects of the intervention may last over time in patients with dementia.
Neuroimaging studies in healthy subjects have shown that the parietal cortex activates bilaterally during mental calculation.23,24 In this intervention, patients must first learn to operate an abacus (understanding the value of each bead and the rules of use) and perform calculations using this tool. Patients later perform the same calculations mentally by applying the strategies they learned from using the abacus. In addition to mental calculation, this intervention involves such other cognitive functions as visuospatial skills, working memory, executive function, and episodic and semantic memory. This probably means that large neural networks in the frontal, parietal, and temporal cortex are also involved. Thus, using an abacus may stimulate multiple cognitive domains as well as a wide range of brain circuits and areas. However, studies similar to the ones conducted in children should be conducted in elderly patients to confirm this hypothesis.25
Our study has a number of limitations. The small sample size, inherent to pilot studies, does not allow us to draw definitive conclusions on the effectiveness of the intervention. However, our data on usability, satisfaction, participation, and attendance are relevant, which suggests that this type of intervention may be a promising tool for cognitive stimulation in the elderly. In addition, as patients were assessed right after the intervention, we do not know the effects of this type of cognitive stimulation in the long term. Finally, using an abacus requires a minimum knowledge of mathematics and level of literacy, which may be a limiting factor for certain population groups.
In conclusion, our study shows that a cognitive stimulation method based on abacus arithmetic may be useful in elderly patients, both with and without cognitive impairment. Randomised comparative studies with longer follow-up periods should be conducted to evaluate the effectiveness of this method on patients’ cognition and behaviour.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank BrainFactory +50 for their cooperation with the Spanish Society of Neurology's Research Operations Office in conducting this study.
Please cite this article as: Matías-Guiu JA, Pérez-Martínez DA, Matías-Guiu J. Estudio piloto de un nuevo método de estimulación aritmética empleando el ábaco en ancianos sanos y con trastorno cognitivo. Neurología. 2016;31:326–331.