Anxiety has negative effects on the cognitive performance and psychosocial adjustment of elderly people. Given the high prevalence of anxiety symptoms in patients suffering from cognitive impairment, it has been suggested that these symptoms may be an early marker of dementia. The State-Trait Anxiety Inventory (STAI) is one of the widely-used used scales for evaluating anxiety in elderly people. However, inasmuch as the STAI may be difficult to apply to older people, having a short form of it would be desirable.
MethodsThe participants comprised 489 community-dwelling individuals aged 68 years and over. All of them were volunteers in a longitudinal study for early detection of Alzheimer’ Disease (Proyecto Vallecas). The full sample was divided in two homogeneous subgroups: Group A, used to reduce the number of items and response options, and Group B, the group used to determine the psychometric properties of the new short form (STAIr).
ResultsA dichotomous Rasch model was used to obtain the STAIr. No statistically significant differences for STAIr scores were found with respect to sociodemographic variables. Psychometric properties and normative data were obtained for the new short-version.
ConclusionsThe STAIr is composed of 13 items and data fits the model well. Since it is short and easy to apply to elderly people, STAIr will be very useful in clinical and research settings.
La ansiedad tiene efectos negativos sobre el rendimiento cognitivo y el ajuste psicosocial de las personas mayores. Dada la elevada prevalencia de los síntomas de ansiedad en personas con deterioro cognitivo, se ha indicado que podrían ser un marcador precoz de demencia. Una de las pruebas más utilizadas para valorar el nivel de ansiedad en personas mayores es el Inventario de Ansiedad Estado-Rasgo (STAI). No obstante, en la medida en que puede resultar una escala larga para los mayores, sería deseable contar con una versión abreviada de la misma.
MétodosSe reclutó una muestra de 489 participantes mayores de 68 años cognitivamente sanos, todos ellos eran voluntarios en un proyecto de investigación longitudinal sobre la enfermedad de Alzheimer (Proyecto Vallecas). La muestra se subdividió en 2 grupos homogéneos: el grupo A se utilizó para reducir el número de ítems y de opciones de respuesta, y el grupo B para obtener las propiedades psicométricas de la nueva escala reducida (STAIr).
ResultadosSe empleó el modelo de Rasch dicotómico para obtener el STAIr. Las variables sociodemográficas no mostraron asociación con las puntuaciones de la nueva versión. Se estudiaron las propiedades psicométricas y se hallaron los datos normativos del STAIr.
ConclusionesLa nueva versión STAIr se compone de 13 ítems y presenta una adecuada bondad psicométrica. En la medida en que es una escala rápida y sencilla para las personas mayores, su aplicación resulta útil en los contextos clínico e investigador.
Anxiety is a feeling of agitation and restlessness in response to certain situations. It is a generally unpleasant emotional state manifesting, to a greater or lesser extent, with a triple cognitive, physiological, and behavioural response to stimuli that are perceived as dangerous or threatening. These stimuli are environmental or even psychological (thoughts, mental images, etc.).
Anxiety disorders constitute one of the most prevalent mental disorders worldwide. According to the European Study of the Epidemiology of Mental Disorders (ESEMeD), 13.6% of the population has experienced some type of anxiety disorder at one point in their lives, and 6.4% were affected in the past year.1 Similarly, a systematic review of 27 epidemiological studies conducted in Europe reports a prevalence of 12% for anxiety disorders.2 In Spain, lifetime prevalence of anxiety disorders is estimated at 9.4%, and the probability of having experienced an anxiety attack in the last year is 6.2%.3
Anxiety disorders are also some of the most frequently diagnosed psychiatric disorders among the elderly.4 Prevalence rates range from 15% to 52% for anxiety symptoms and 3% to 15% for clinical anxiety disorders that match diagnostic guidelines.5 According to several studies with clinical populations, anxiety symptoms present with a frequency of 24% in patients with mild cognitive impairment6 and 27% to 40% in patients with dementia.7
We must pay particular attention to presence of anxiety symptoms in elderly patients since these symptoms may have a negative impact on their psychosocial adjustment. Elderly patients with anxiety symptoms tend to show lower levels of autonomy, greater loss of visual and auditory acuity, neurotic traits, poor self-perceived health and quality of life, greater use of healthcare services, and increased risk of mortality.8–12 Furthermore, anxiety and cognitive performance are closely linked in elderly subjects with normal cognitive function.13 There is an inversely proportional association between anxiety levels and performance in episodic memory tasks,14,15 processing speed,16 selective attention,17 and executive function.18,19 Likewise, there is a greater prevalence of anxiety symptoms in patients with cognitive impairment than in subjects with normal cognitive function.20–22 Some authors have highlighted the role of anxiety as an early predictor of cognitive impairment,23 and as a marker of mild cognitive impairment conversion to dementia.22,24,25 Decreased cognitive function has been linked to poorer prognosis and resistance to anxiety treatment in elderly patients.26
Some of the best-known questionnaires for assessing anxiety are the Beck Anxiety Inventory (BAI),27 the Taylor Manifest Anxiety Scale (TMAS),28 the Inventory of Situations and Responses of Anxiety (ISRA),29 and the State-Trait Anxiety Inventory (STAI).30 The latter has become the most widely-used anxiety questionnaire among Spanish psychologists.31 The STAI is based on a theoretical model that recognises 2 components of anxiety: state anxiety and trait anxiety. State anxiety is a temporary emotional state characterised by consciously perceived subjective feelings of tension and apprehension, and by autonomic nervous system hyperactivity. Trait anxiety is a relatively constant personal tendency to perceive situations as threatening, which in turn increases the individual's level of anxiety. Each of these 2 components is assessed with a 20-item self-reported subscale.
The STAI is one of the most preferred scales for assessing anxiety in the elderly for 2 main reasons. Firstly, it evaluates the cognitive component of anxiety almost exclusively, since no items addressing physiological symptoms are included. Elderly patients often find it difficult to interpret STAI items since they are vague and describe feelings that may well be mistaken for the side effects of some common drugs.32 And secondly, the STAI is extremely sensitive at detecting numerous mental disorders in the elderly.33 As a result, the STAI has been validated specifically for elderly people32,34 and its psychometric properties have been analysed in this population.35 In Spain, this questionnaire has been validated recently for young adults36; however, no normative data for older adults are available.
Our purpose is to provide an assessment tool that will effectively detect anxiety symptoms in the elderly. To this end, we used the Item Response Theory (IRT), a theory which has been proved superior to other psychometric methods for item reduction and has been applied to other tests with excellent results.37 We therefore analysed the 2 STAI subscales based on the IRT to select the most discriminatory items on the anxiety continuum. Additionally, we created a reduced version (STAIr) including only 2 of the 4 original response options in order to minimise the difficulties elderly patients often experience with polytomous items. The result was a short inventory that can be quickly applied and easily completed. Lastly, we studied the psychometric properties of this new version and provide normative data that may be used in clinical and research settings.
Subjects and methodsSampleWe included 489 consecutive adults older than 69 and with normal cognitive function (mean age [SD], 74.35 [4.10]; mean school years, 10.71 [6.24]; 62.09% female). All subjects were voluntary participants in Proyecto Vallecas, a longitudinal research project focusing on early detection of Alzheimer disease and conducted by the Fundación Centro de Investigación de Enfermedades Neurológicas and the Queen Sofía Foundation. All participants underwent a thorough evaluation consisting of a neurological examination and a neuropsychological assessment, including the Mini Mental State Examination (MMSE),38 a biochemical and genetic analysis, and a neuroimaging study. The STAI was used to evaluate anxiety symptoms. We excluded all subjects with primary degenerative dementias, psychiatric symptoms, history of cerebrovascular accident, head trauma, encephalitis, normal pressure hydrocephalus, systemic disorders, neurosurgery, or drug abuse. All participants were native Spanish speakers.
According to the study's requirements, the sample was divided into 2 groups comprising 400 and 89 patients, respectively. In Group A, the IRT model was applied to the 2 STAI subscales in order to produce the new brief version. Once the 2 sub-samples were proved to be homogeneous, we used group B to compare the 2 versions in order to determine the psychometric properties of STAIr.
Material and methodsA structured interview was used to gather sociodemographic and clinical data from all participants. The neuropsychological assessment protocol, which included administration of the STAI, was applied in a single session lasting about 1hour; all participants were evaluated under similar conditions. Likewise, all participants were informed that they were allowed to take a break to prevent fatigue from affecting their cognitive performance. A psychologist was present at all times while the participants were filling in questionnaires in order to answer any questions.
The STAI was applied according to the instructions listed in its manual.39 This questionnaire consists of 2 subscales (state anxiety and trait anxiety) comprising 20 items each; some items are reverse-coded. Each item has 4 response options scored 0 (never/almost never) to 3 (always/almost always). Total score on each subscale was the sum of all item scores (negatively-keyed items were reverse-scored). Therefore, each subscale is scored from 0 to 60; higher scores correspond to greater anxiety. Participants’ responses were noted on response sheets for later codification and statistical analysis.
Statistical analysisFirstly, we studied the dimensional structure of the 2 STAI subscales. To this end, we used MicroFACT 2.0 software to conduct an exploratory factor analysis based on the polychoric correlations between items.40 Principal axis method and promax rotation were used to extract factors.
Once the 2 scales were confirmed to have a one-dimensional structure, the original polytomous items were dichotomised to create a new questionnaire that would be easier for the elderly to complete. We conducted a preliminary study to determine the best way to recode items and finally chose to limit the 4 original response options (3, 2, 1, 0) to a dichotomy (1, 0), maintaining the ordinal scale. Response options were recoded as follows: 3 and 2 on STAI became 1 on STAIr, and response options 1 and 0 became 0. ConQuest software41 was used to analyse how items fitted the dichotomous Rasch model. The infit and outfit statistics were used to evaluate model-data fit, with the interval [−2,+2] as a reference. Items were deleted in several stages based on the results of fit statistics.
Finally, we used an open-source software environment, R version 2.15, to determine the psychometric characteristics of the new short form in a new sample of subjects with normal cognitive function.42 We analysed potential statistically significant differences between the 2 groups regarding sociodemographic and neuropsychological variables (MMSE and STAI). Non-parametric tests were used due to disparities in group size: chi-square test for dichotomous variables, and Mann–Whitney and Kruskal–Wallis tests to make comparisons between 2 groups or more than 2 groups, respectively. The correlation between STAI and STAIr was analysed and Guttman's lambda 4 coefficient (λ4) was used to determine reliability of the new version. Normative data were generated by grouping raw scores by percentile ranks according to their position in the distribution. These percentile ranks were subsequently transformed into scaled scores to ensure as normal a data distribution as possible to enable comparisons between subjects. State anxiety and trait anxiety scores 1.5 standard deviations above the mean were considered indicative of high anxiety levels; this procedure is frequently used in the health sciences to define cut-off points.43
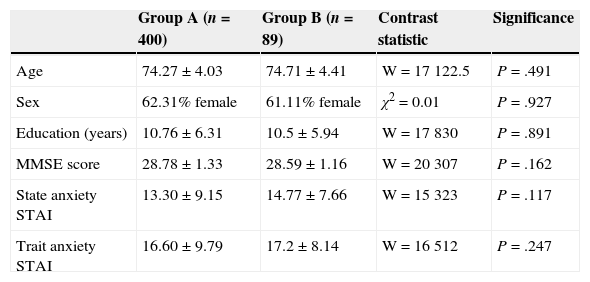
ResultsStudy sample characteristics are shown in Table 1. Group A was used to reduce the number of items and response options on the STAI; group B was used to validate the new short form and obtain normative data. No statistically significant differences were found between the groups regarding age, sex, educational level, and scores on the MMSE and the STAI subscales, and these results confirmed that the 2 groups were homogeneous.
Sociodemographic characteristics of sample groups A and B.
| Group A (n=400) | Group B (n=89) | Contrast statistic | Significance | |
|---|---|---|---|---|
| Age | 74.27±4.03 | 74.71±4.41 | W=17122.5 | P=.491 |
| Sex | 62.31% female | 61.11% female | χ2=0.01 | P=.927 |
| Education (years) | 10.76±6.31 | 10.5±5.94 | W=17830 | P=.891 |
| MMSE score | 28.78±1.33 | 28.59±1.16 | W=20307 | P=.162 |
| State anxiety STAI | 13.30±9.15 | 14.77±7.66 | W=15323 | P=.117 |
| Trait anxiety STAI | 16.60±9.79 | 17.2±8.14 | W=16512 | P=.247 |
MMSE: Mini Mental Status Examination; STAI: State-Trait Anxiety Inventory; W: Wilcoxon.
The strong correlation between the 3 factors identified in the exploratory factor analysis (r=0.68) suggested that all items revolve around the same one-dimensional concept of anxiety. As a result, no items had to be deleted before the IRT could be applied to the STAI subscales.
The dichotomous Rasch model was applied to the new item coding (1,0). The state anxiety STAI subscale was analysed in 2 consecutive stages. Only 6 items were shown to fit the model; consequently, the new state anxiety subscale included items 1, 5, 8, 12, 18, and 19 (χ2[5]=370.59; P<.001). Of these, items 1, 5, 8, and 19 were negatively keyed and responses therefore had to be recoded (scores of 1 were transformed into 0). Items in the trait anxiety STAI subscale were deleted in 4 consecutive stages. Only 7 items fitted the dichotomous Rasch model in the fourth stage; these made up the trait anxiety STAIr subscale: 27, 29, 30, 31, 32, 33, and 38 (χ2[6]=506.39; P<.001). As items 27, 30, and 33 were negatively keyed, responses needed to be recoded.
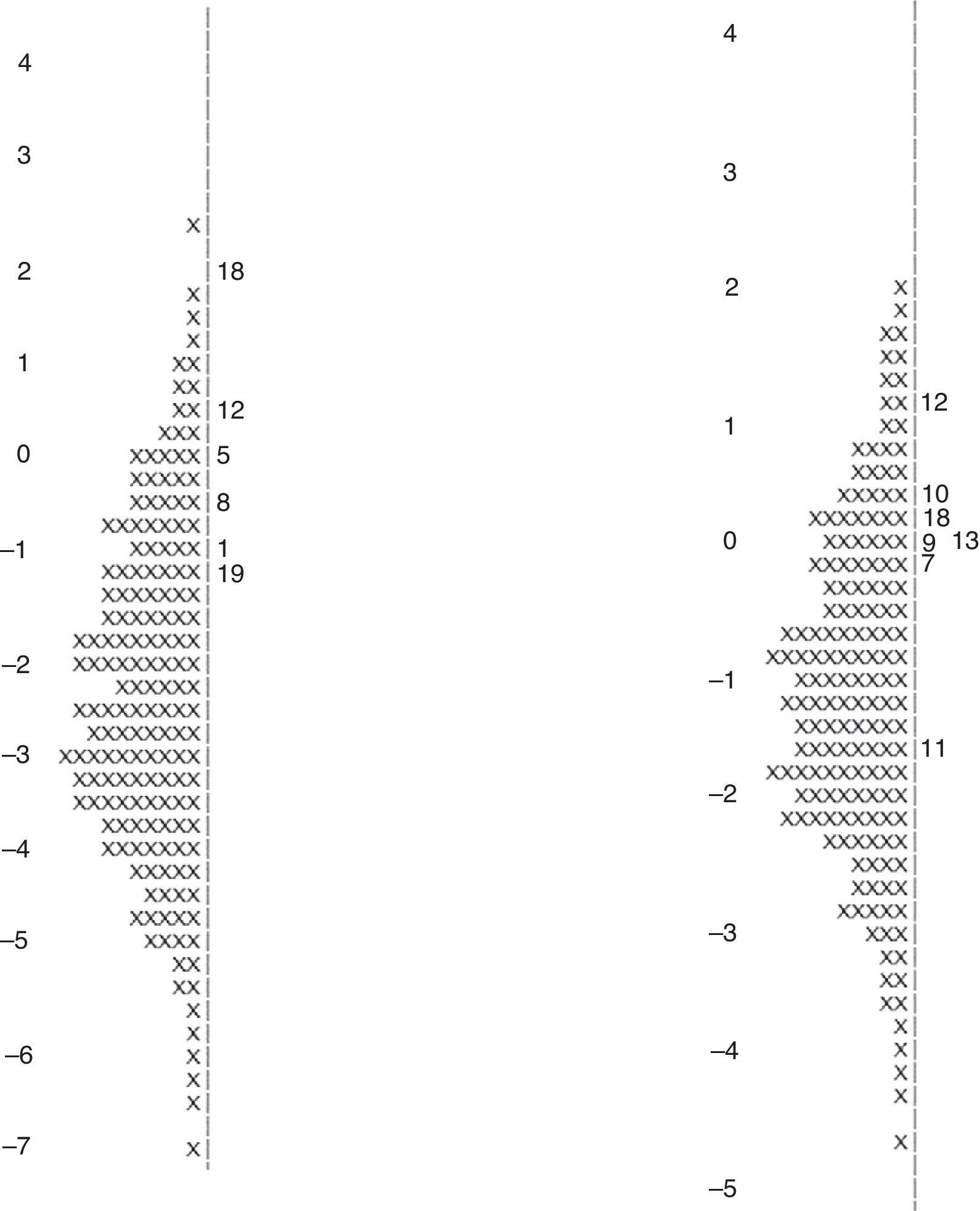
Fig. 1 shows the Wright map for the 2 STAIr subscales. In both cases, items are sufficiently different from one another and cover the whole anxiety continuum. Furthermore, the parameter separation reliability coefficient was 0.990 for the 2 subscales, which points to good item fit since the acceptable interval for this coefficient is (0,1).
Once the short STAI subscales had been created, we studied their properties with group B. Results showed an adequate correlation between STAI and STAIr for both the state anxiety and the trait anxiety subscales (r=0.81 and r=0.80, respectively). The reliability coefficient was higher for the STAI state anxiety subscales (λ4=0.86) and trait anxiety subscales (λ4=0.81) than for the STAIr subscales (λ4=0.58 and λ4=0.60, respectively).
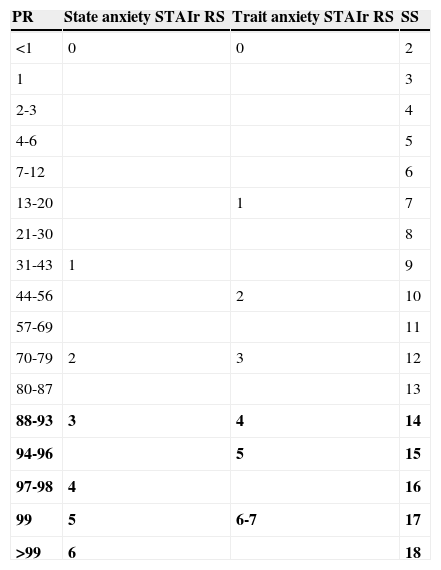
We subsequently studied the potential influence of sociodemographic variables on both STAIr subscales since these variables are so important when obtaining normative data for the inventory. No significant differences were found in the state anxiety STAIr subscale regarding age (Kruskal–Wallis χ2[2]=2.75; P=.253), sex (W=2.75; P=.050), or educational level (Kruskal–Wallis χ2[2]=1.51; P=.471). The trait anxiety STAIr subscale showed no significant differences for age (Kruskal–Wallis χ2[2]=0.05; P=.975), sex (W=963; P=.762), or educational level (Kruskal–Wallis χ2[2]=0.61; P=.738). Therefore, none of these variables was used to stratify STAIr normative data. Table 2 shows the equivalence between raw scores on both subscales, together with percentile ranks and the corresponding scaled scores. Raw scores equal to or higher than 3 or 4 were used as the cut-off point for state anxiety and trait anxiety STAIr subscales, respectively.
Distribution and cut-off points for the state and trait anxiety STAIr subscales.
| PR | State anxiety STAIr RS | Trait anxiety STAIr RS | SS |
|---|---|---|---|
| <1 | 0 | 0 | 2 |
| 1 | 3 | ||
| 2-3 | 4 | ||
| 4-6 | 5 | ||
| 7-12 | 6 | ||
| 13-20 | 1 | 7 | |
| 21-30 | 8 | ||
| 31-43 | 1 | 9 | |
| 44-56 | 2 | 10 | |
| 57-69 | 11 | ||
| 70-79 | 2 | 3 | 12 |
| 80-87 | 13 | ||
| 88-93 | 3 | 4 | 14 |
| 94-96 | 5 | 15 | |
| 97-98 | 4 | 16 | |
| 99 | 5 | 6-7 | 17 |
| >99 | 6 | 18 |
Data in bold express scores that may be interpreted as indicative of a high level of anxiety (cut-off point for state anxiety was 3-6, vs 4-7 for trait anxiety).
PR: percentile range; RS: raw score; SS: scaled score.
Anxiety symptoms are highly prevalent among the elderly. Presence of these symptoms has been associated with decreased processing speed16 and poorer cognitive performance13,15,17,19 in elderly patients with normal cognitive function. Likewise, patients diagnosed with cognitive impairment display higher anxiety levels than cognitively healthy subjects.22 This finding has led researchers to consider anxiety as a potential marker of cognitive decline23 and even as a predictor of cognitive impairment conversion to dementia.22,24,25 In light of the above, assessing level of anxiety in cognitive impairment units may be particularly relevant for the diagnosis and prognosis of cognitive decline.
The STAI is used internationally to evaluate anxiety symptoms. However, it may be too long and difficult to complete in some clinical settings. Some researchers have therefore been particularly interested in developing a short version. Several versions have been created to measure anxiety levels in pregnant women,44 patients with mechanical ventilatory support,45 or patients scheduled for surgery with general anaesthesia,46 and these versions are based on different statistical techniques,47 including IRT.46
Assessing elderly patients with STAI and other such subjective scales with polytomous items has several disadvantages: patients may be confused and unable to understand the question, and they may even find it difficult to choose a response option since they may not understand ordinal scales. In contrast, dichotomous items are much more suitable for the elderly population since they reduce confusion and uncertainty about answers.48 The purpose of the present study was to design a short questionnaire that can be completed in a short time and which evaluates the presence of anxiety symptoms in elderly patients. To this end, we administered the STAI to a sample of elderly subjects with normal cognitive function and applied the IRT to items on both STAI subscales.
Psychometric analyses determined the structure of the new short versions of the state anxiety and trait anxiety subscales, which were made up of 6 and 7 dichotomous items, respectively. According to the bivariate analysis, STAIr scores were not influenced by either age, sex, or educational level. These findings reveal that anxiety levels in elderly patients are less influenced by sociodemographic variables in the new short version of STAI. However, this hypothesis should be interpreted with caution; further studies are necessary to prove its validity.
Furthermore, we found striking disparities between anxiety scores in our sample and those obtained in other studies including young adults.36 Some studies have shown that elderly people are eager to present themselves as socially desirable and therefore score higher on social desirability scales than younger individuals.49,50 This may lead anxiety levels in elderly subjects to appear lower than they actually are.
Reducing the number of items is associated with decreases in scale reliability,51 which may explain why the STAIr subscales showed decreased reliability. On the other hand, reducing the number of response options is also problematic: decreased variance of total scores leads to a decreased reliability index.52 Both of these factors could explain the reduced reliability of the STAIr. However, reliability indices for the STAIr are moderate and there is a strong correlation between the STAIr and the STAI subscales. We can therefore state that the STAIr has acceptable psychometric properties.
In conclusion, the negative impact of anxiety disorders on psychosocial adjustment and cognitive function in the elderly has led many authors to suggest that anxiety is an early predictor of cognitive impairment and of conversion to dementia. Although anxiety is not usually evaluated in clinical and research settings, tools for measuring the level of anxiety in the elderly are necessary, especially in cognitive impairment research. This study describes modifications to the STAI, one of the most widely-used scales for anxiety, to create a short version, the STAIr. This scale demonstrates appropriate psychometric properties and can be applied quickly and easily to elderly subjects.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Fernández-Blázquez MA, Ávila-Villanueva M, López-Pina JA, Zea-Sevilla MA, Frades-Payo B. Propiedades psicométricas de una nueva versión abreviada del State-Trait Anxiety Inventory (STAI) para valorar el nivel de ansiedad en personas mayores. Neurología. 2015;30:352–358.