Lyme disease is a multisystemic infectious disease that affects the nervous system in 10% of all cases.1 It is caused by a spirochete, B. burgdorferi (Borrelia burgdorferi sensu lato), and transmitted by hard ticks (Ixodes ricinus in Europe).2,3 Neurological symptoms typically appear 1 to 12 weeks after the arthropod bite; the most common symptoms in our setting are painful meningoradiculitis and cranial nerve palsy.4–6 Many patients report having had a tick bite and a skin lesion, called erythema migrans (EM).7
A correct diagnosis of neuroborreliosis requires a suggestive clinical profile in the right epidemiological context, in addition to clear microbiological criteria (intrathecal synthesis of anti-B. burgdorferi antibodies or direct detection of the agent).8 Patients normally present lymphocytic pleocytosis in addition to high protein and normal glucose levels in cerebrospinal fluid (CSF). Patients respond well to antibiotics, with symptoms subsiding in 7 to 14 days.9
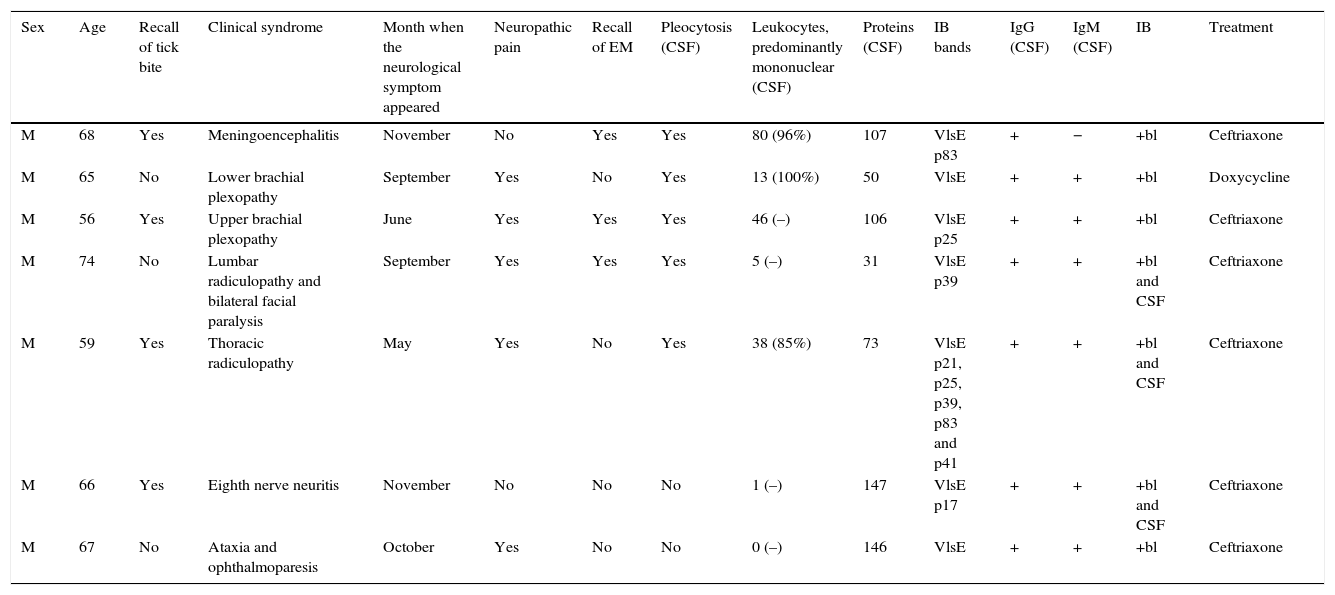
We describe the clinical, epidemiological, and microbiological characteristics of patients affected by neuroborreliosis (compatible symptoms plus positive IgG ELISA and immunoblot [IB] and/or positive PCR) between 2007 and 2012 (Table 1).
Patient characteristics.
| Sex | Age | Recall of tick bite | Clinical syndrome | Month when the neurological symptom appeared | Neuropathic pain | Recall of EM | Pleocytosis (CSF) | Leukocytes, predominantly mononuclear (CSF) | Proteins (CSF) | IB bands | IgG (CSF) | IgM (CSF) | IB | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 68 | Yes | Meningoencephalitis | November | No | Yes | Yes | 80 (96%) | 107 | VlsE p83 | + | − | +bl | Ceftriaxone |
| M | 65 | No | Lower brachial plexopathy | September | Yes | No | Yes | 13 (100%) | 50 | VlsE | + | + | +bl | Doxycycline |
| M | 56 | Yes | Upper brachial plexopathy | June | Yes | Yes | Yes | 46 (–) | 106 | VlsE p25 | + | + | +bl | Ceftriaxone |
| M | 74 | No | Lumbar radiculopathy and bilateral facial paralysis | September | Yes | Yes | Yes | 5 (–) | 31 | VlsE p39 | + | + | +bl and CSF | Ceftriaxone |
| M | 59 | Yes | Thoracic radiculopathy | May | Yes | No | Yes | 38 (85%) | 73 | VlsE p21, p25, p39, p83 and p41 | + | + | +bl and CSF | Ceftriaxone |
| M | 66 | Yes | Eighth nerve neuritis | November | No | No | No | 1 (–) | 147 | VlsE p17 | + | + | +bl and CSF | Ceftriaxone |
| M | 67 | No | Ataxia and ophthalmoparesis | October | Yes | No | No | 0 (–) | 146 | VlsE | + | + | +bl | Ceftriaxone |
EM: erythema migrans; IB: immunoblot; Ig: immunoglobulin; CSF: cerebrospinal fluid; F: female; bl: blood; M: male.
A 68-year-old man with no relevant medical history arrived at the emergency department in November 2009 with loss of consciousness and generalised tonic-clonic seizures. For 2 days he had had fever and felt unwell. Examination revealed somnolence, disorientation in time, and dysarthria. Blood analysis results were within normal limits and a CT scan showed no abnormalities. The CSF study yielded 80 predominantly mononuclear leukocytes as well as anti-B. burgdorferi antibodies. The patient was treated with doxycycline 100mg/12hours for 21 days in addition to valproic acid 500mg/12hours; he was asymptomatic a month later. The patient reported having been bitten by ticks in the weeks previous to admission, and remembered seeing a lesion compatible with EM.
Case 2A 65-year-old man with no relevant events in his medical history reported pain in the right shoulder radiating to the wrist over the previous 2 months. The pain occurred when he extended his right arm or flexed his wrist, together with tingling in the fourth and fifth fingers of the same hand. Triceps areflexia was noted during the physical examination. A neurophysiological study yielded a diagnosis of carpal tunnel syndrome. As the symptoms did not coincide with the result of the electroneurography (ENG) study, a lumbar puncture (LP) was performed to complete the study. Pleocytosis and anti-B. burgdorferi antibodies were observed in the CSF sample. Treatment consisted of 100mg of doxycycline every 12hours for 28 days, resulting in a good outcome. No follow-up testing was done. The patient did not report either a tick bite or EM.
Case 3In June 2011 a 56-year-old man was admitted due to intense pain and weakness in the right arm in the preceding month with no relief after treatment with analgesics. Biceps and triceps weakness was observed, in addition to decreased wrist extension on the right side (3/5), interosseous muscle weakness (1-2/5), along with significantly decreased reflexes in the right arm, without changes in sensitivity. An electroneurogram confirmed the presence of lower brachial plexopathy. Predominantly lymphocytic pleocytosis and anti-B. burgdorferi antibodies were found in the CSF. After 4 days of treatment with ceftriaxone 2g IV/d, the pain had disappeared and the patient had made significant gains in muscle strength. The patient was discharged after 21 days of treatment and was asymptomatic at his one-month follow-up visit. The patient reported having been bitten by a tick as well as a lesion compatible with EM.
Case 4A 74-year-old woman with no relevant medical history began to experience lumbar pain in September 2011. Symptomatic treatment brought no relief, and she reported radiating sciatic pain to her left lower limb; an examination revealed L5 radiculopathy without accompanying weakness. After 21 days she was admitted to hospital for pain treatment. While hospitalised, she presented bilateral facial paralysis. An LP revealed high numbers of predominantly lymphocytic leukocytes, in addition to anti-B. burgdorferi antibodies in the CSF. Treatment with ceftriaxone 2g IV/d was initiated, with a favourable outcome. The patient reported having seen a lesion compatible with EM a week before, although she could not recall a tick bite.
Case 5A 59-year-old man with no relevant medical history was admitted to hospital in June 2011 with fever and pain in the rib area. The patient reported having felt intense pain on the left side of the ribcage, associated with decreased sensitivity in the same area, for 15 days. Examination revealed left-sided hypoaesthesia at the T2 level and bilateral hypoaesthesia at the T3-T6 level compatible with thoracic radiculopathy. A CSF study yielded lymphocytic pleocytosis and intrathecal antibody synthesis. PCR testing for B. burgdorferi was positive, but the sequence matched Borrelia garinii. Treatment with ceftriaxone 2g IV/d for 21 days resolved all symptoms. The patient reported having had multiple tick bites in the preceding 2 months.
Case 6This 66-year-old woman had had EM rashes 6 years earlier and received appropriate treatment with doxycycline. In November 2010 she reported sudden deafness, gait instability, nausea, vomiting, and sweating, all of which improved over the next few days except the deafness. She was admitted and underwent a brain and petrous portion MRI which showed no changes. Autoimmune test results were normal. An ELISA test for B. burgdorferi proved positive, so an LP was performed. Although it yielded only one leucocyte, anti-B. burgdorferi antibodies were found and confirmed with immunoblot (IB) in blood and CSF. Treatment with ceftriaxone 2g IV/d for 21 days resulted in partial resolution of hearing loss.
Case 7A 67-year-old man without relevant medical history reported intense lumbar pain in the preceding month, plus unstable gait and double vision in the preceding 8 days. Examination revealed ophthalmoparesis with bilateral sixth nerve impairment, gait ataxia, and absence of deep tendon reflexes in the lower limbs. Results from blood and CSF analysis were within normal limits. An electromyogram (EMG) showed the absence of H-reflex in both lower limbs. Results from other nerve conduction studies and muscle examinations were within normal limits. Suspicion of Miller Fisher syndrome led to treatment with intravenous immunoglobulin. After 15 days the persistence of symptoms prompted doctors to perform a follow-up study on the patient, and a new LP revealed high protein levels and no leukocytes. A B. burgdorferi ELISA test (IgG ELISA and IB) gave positive results. The patient improved gradually during treatment with ceftriaxone 2g IV/d for 21 days until becoming asymptomatic.
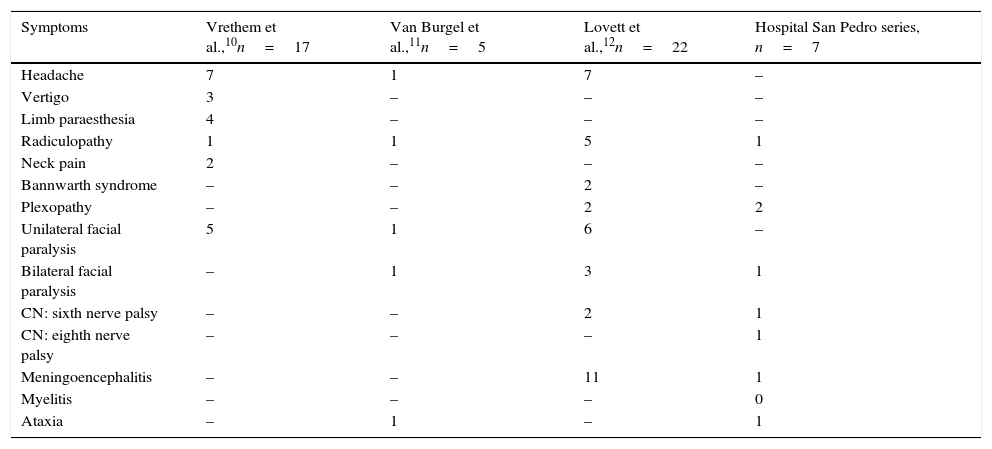
In this case series from a tertiary referral hospital in an area where Lyme disease is endemic, 7 patients out of a population of 310000 were diagnosed with neuroborreliosis over a 6-year period. The clinical and microbiological characteristics are similar to those described in other European series10–12 (Table 1). The last patient was unlike the others in that he suffered from ataxia and ophthalmoparesis, which has been described in the literature only rarely.13 It is interesting that neuropathic pain appeared relatively frequently, in 5 out of 7 patients (Table 1). We would like to highlight that nearly half the patients had no memory of either a tick bite or EM (Table 1). On this basis, we conclude that doctors must investigate the possibility of B. burgdorferi infection in patients with neurological symptoms who live in endemic areas14,15 (Table 2).
Clinical manifestations of neuroborreliosis in different studies.
| Symptoms | Vrethem et al.,10n=17 | Van Burgel et al.,11n=5 | Lovett et al.,12n=22 | Hospital San Pedro series, n=7 |
|---|---|---|---|---|
| Headache | 7 | 1 | 7 | – |
| Vertigo | 3 | – | – | – |
| Limb paraesthesia | 4 | – | – | – |
| Radiculopathy | 1 | 1 | 5 | 1 |
| Neck pain | 2 | – | – | – |
| Bannwarth syndrome | – | – | 2 | – |
| Plexopathy | – | – | 2 | 2 |
| Unilateral facial paralysis | 5 | 1 | 6 | – |
| Bilateral facial paralysis | – | 1 | 3 | 1 |
| CN: sixth nerve palsy | – | – | 2 | 1 |
| CN: eighth nerve palsy | – | – | – | 1 |
| Meningoencephalitis | – | – | 11 | 1 |
| Myelitis | – | – | – | 0 |
| Ataxia | – | 1 | – | 1 |
CN: cranial neuropathy.
Please cite this article as: Gómez-Eguílaz M, Gómez-Cerquera J, Calvo-Pérez L, Oteo JA. Neuroborreliosis: serie de 7 casos en un hospital. Neurología. 2016;31:137–139.
Part of the information in this article was reported at the SEN Annual Meeting in November 2012 and the number of patients was increased for the meeting of the Basque Society in March 2013.