Non-traumatic torsion is a rare cause of the palsy of radial and some other nerves of upper extremities. It can be visualized using high-resolution ultrasound (HRUS) as an hourglass-shaped constriction, which may be complete or incomplete.1 If associated with focal peripheral nerve paralysis of immunological etiology, it satisfies criteria of neuralgic amyotrophy (NA).2 We present a case of bilateral radial nerve torsion as the only sign of NA, which was diagnosed using HRUS after the patient underwent many other tests within several months period of time.
A 34-year-old woman was referred to our tertiary care center with a 13-month history of bilateral wrist and fingers drop. In April 2020, in the fourth week of her pregnancy, she experienced a sudden pain at night located in the right elbow followed by inability to extend her wrist and fingers. She underwent physiotherapy and the pain diminished after 4 weeks, however without any functional recovery. Three months later she experienced pain in similar location in the left extremity followed by the same motor deficits. The symptoms were preceded neither by trauma, surgery nor by infection. Laboratory work-up and imaging performed prior to consultation at our center were unremarkable.
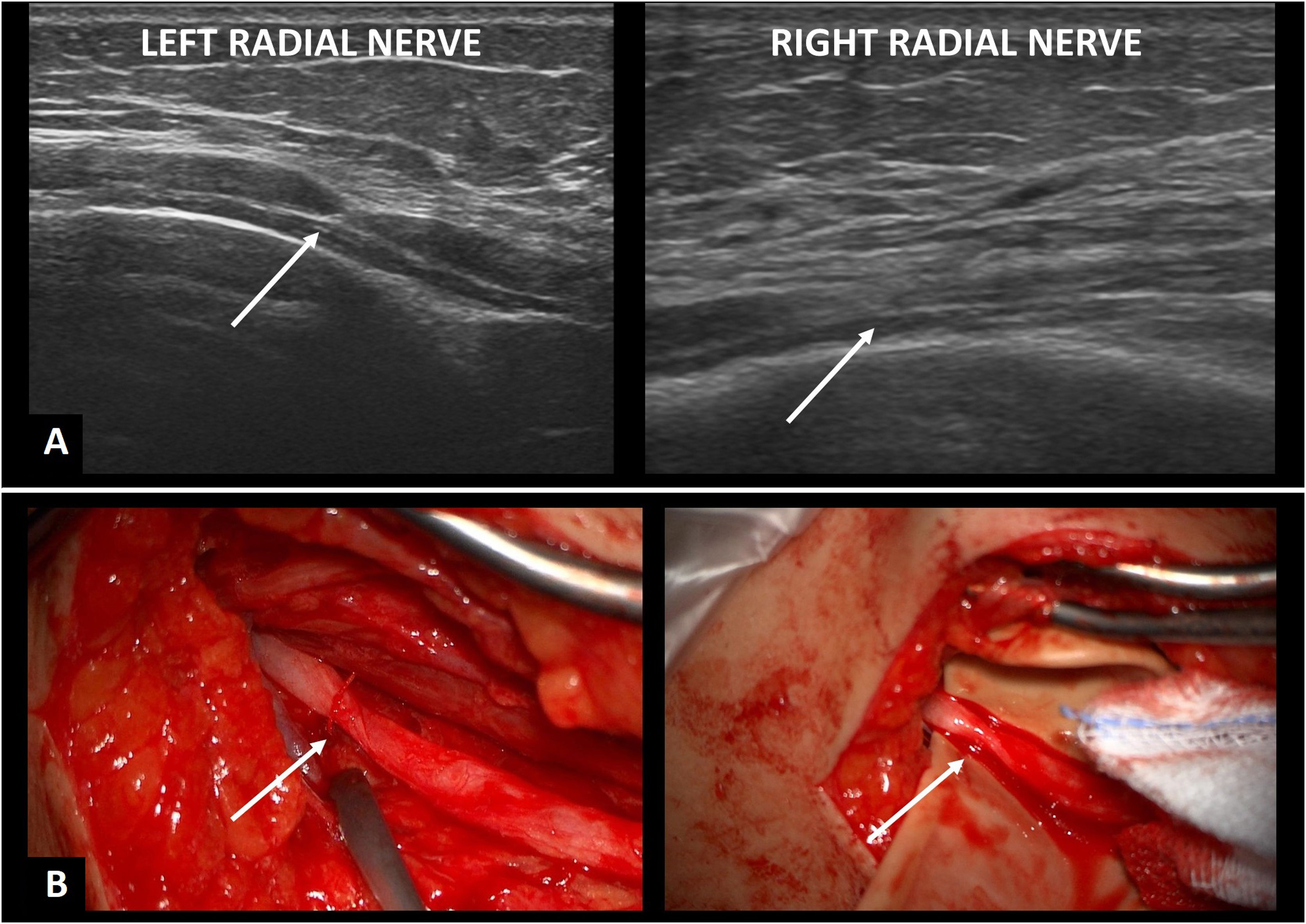
When presenting at our center, the patient showed bilateral complete paralysis of the wrist and finger extension, however without muscle wasting and sensory deficits. The deep tendon reflexes over radial bone were bilaterally diminished. Otherwise, the neurological examination including detailed checking of finger flexion, hand grip, strength of the movement in elbow and shoulder joints was normal. Also the meticulous visual inspection revealed no signs of muscle atrophy in upper extremities and shoulder girdle. Nerve conduction studies (NCS) were done using standard settings as well as stimulating and recording sites.3,4 NCS proved existence of bilateral distal motor-sensory radial neuropathy, more pronounced on the right side (Table 1). The amplitudes of compound motor action potential recorded from extensor indicis proprius and brachioradialis were markedly diminished after stimulation at the elbow and further decreased when the nerves were stimulated at the lateral brachium. A sensory nerve action potential (SNAP) was bilaterally not evocable. Also the assessment of central motor conduction to distal muscles of upper extremities made with transcranial magnetic stimulation was normal. Electromyography showed acute denervation in bilateral extensor indicis proprius and brachioradialis with no voluntary activity. No denervation signs, normal voluntary effort as well as normal motor unit action potentials were seen in both triceps. HRUS revealed bilateral focal enlargement and hourglass-like constrictions of the radial nerves in midarm level, distally to the radial nerve crest. The nerve enlargement was markedly more pronounced on the left side (Fig. 1A).
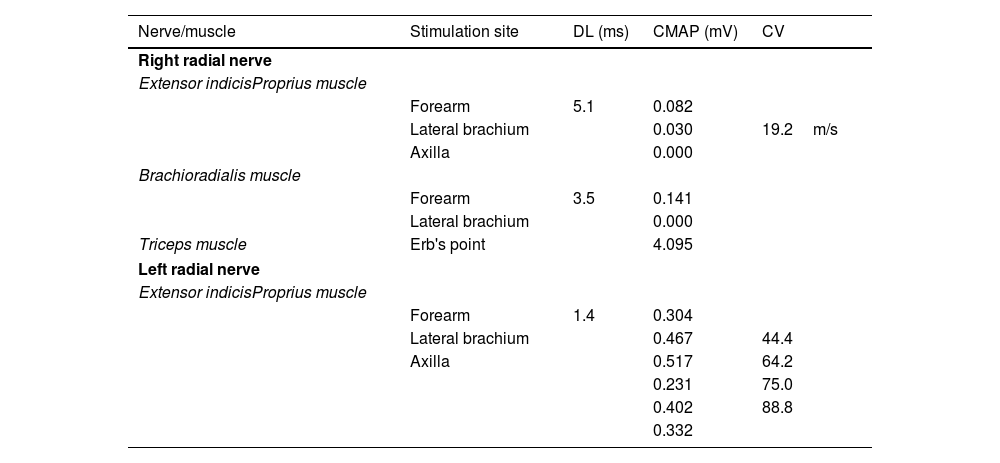
Results of nerve conduction studies.
| Nerve/muscle | Stimulation site | DL (ms) | CMAP (mV) | CV |
|---|---|---|---|---|
| Right radial nerve | ||||
| Extensor indicisProprius muscle | ||||
| Forearm | 5.1 | 0.082 | ||
| Lateral brachium | 0.030 | 19.2m/s | ||
| Axilla | 0.000 | |||
| Brachioradialis muscle | ||||
| Forearm | 3.5 | 0.141 | ||
| Lateral brachium | 0.000 | |||
| Triceps muscle | Erb's point | 4.095 | ||
| Left radial nerve | ||||
| Extensor indicisProprius muscle | ||||
| Forearm | 1.4 | 0.304 | ||
| Lateral brachium | 0.467 | 44.4 | ||
| Axilla | 0.517 | 64.2 | ||
| 0.231 | 75.0 | |||
| 0.402 | 88.8 | |||
| 0.332 | ||||
DL: distal latency; CMAP: compound muscle action potential; CV: conduction velocity.
In June 2021, 11 months after the symptom onset, a spontaneous recovery of motor function was seen on the left side. Within several weeks, patient was able to extend her wrist and fingers, subjectively with only slightly less strength than before the onset. A surgical exploration of the right nerve, which took place in September 2021 revealed a non-compressive torsion at the midarm level (Fig. 1B). During the exploration, the neurolysis and detorsion of the nerve were done. On the follow-up visit, 8 weeks after the surgery, the right nerve was properly positioned, without sonographic signs of torsion but no functional improvement could be seen. Neither it arose after oral steroids. On the left side, despite marked clinical improvement, we could observe persistent torsion with constriction and focal nerve enlargement. The motor conduction remained on both sides unchanged but low amplitude SNAPs in radial nerves appeared bilaterally (right – 7μV; left – 5μV). The surgery and the pharmacotherapy have been delayed due to intensive involvement of our hospital, including authors, in the care of patients with COVID-19 infection. The patient has been finally referred to the hand surgery clinic and is currently undergoing a process of planning the tendon transfer procedure for the right extremity.
NA (also known as Parsonage-Turner syndrome) is an acute, monophasic, focal or multifocal inflammatory neuropathy affecting usually particular nerves of brachial plexus. Its mainstay features are unilateral, multifocal upper limb weakness and atrophy, which follow the attack of severe neuropathic pain. Only minority of cases suffers bilateral, symmetric symptoms. Similarly, nerve torsion can be identified only in small portion of affected individuals. Typically, NA is a unilateral disorder of a monophasic course, although the symptoms and nerve involvement may reoccur. In the current case, the symptoms were symmetric in severity, limited to radial nerves, however their onset on each side was separated by several months’ interval. The torsion occurred bilaterally, which – to the best of our knowledge was never reported before. According to the results of the large studies with idiopathic or hereditary NA, lesion of radial nerve was observed in 5% of cases. The symptoms affecting both upper extremities are observed in up to one third of diagnosed cases, however bilateral, symmetric involvement of particular nerves occurs as rarely as in approximately 0.8% of patients, most often with simultaneous side involvement.5,6 Sequential course – although documented previously – is even more unusual.7 These features as well as limitation of the process to radial nerves may put in question the diagnosis of NA. On the other side, an extensive radiologic and laboratory testing did not reveal other possible background of the symptoms. Finally, the non-traumatic nerve torsion almost never occurs in conditions other than NA. Although NA has been considered as a rare disorder, recent studies indicate that it is vastly underdiagnosed with a real incidence rate reaching 1 per 1000 per year.8 Lack of awareness of the disorder in primary care setting hinders quick and accurate identification.8 In the case of our patient, diagnosis was probably delayed due to unusual presentation with symmetric involvement of a just single nerve. Thus, our report stresses the previously postulated need of broader use of HRUS in patients with focal peripheral neuropathies; here particularly in patients with radial nerve palsy, especially if occurring bilaterally or not resolving spontaneously.9
The concept of immune-triggered, focal inflammation has been widely accepted as the process underlying NA.10 Three quarters of neuralgic amyotrophy patients report a preceding factor,11 similar to other autoimmune disorders, including but not limited to, trauma, all kinds of surgery, infections, and pregnancy (which was the only association with NA in the current case). The delay between the trigger and the onset of pain should be less than a month.11 Nagano and Lundborg have postulated that the possible mechanism of nerve torsion is initiated by inflammatory process, which leads to intraneural edema and swelling of the nerve.12,13 Aranyi et al. indicated that inflammation leads to constriction of the nerve which is a precursor of the torsion.14 Our diagnostics lacked genetic testing. Therefore we cannot definitely exclude hereditary etiology, which may occur in up to 10% of NA cases. On the other side, the lack of family history and association of symptom onset with pregnancy makes the genetic background unlikely.
While NA in our case was bilateral, the left side recovered spontaneously. Moreover, functional recovery was not associated with changes in ultrasonographic picture, which showed continuously focal nerve enlargement with constriction. When we saw the patient for the first time, the loss of finger and wrist extension was complete on both sides. The left side was characterized by shorter disease duration, slightly better motor conduction and markedly more pronounced neve enlargement compared to the right side. We can speculate that the enlargement reflected inflammation, which promoted the nerve reorganization and recovery. Our case indicates that spontaneous recovery is possible even if the constriction is complete and most probably associated with torsion (ultrasonographic picture was similar to the right side, where the torsion had been visualized during surgical exploration). The right nerve remained paralyzed despite surgical intervention and steroids. Surgical intervention with detorsion has the highest chance of functional recovery when performed within 3 months since the disease onset.9 Nevertheless, a functional benefit has been reported after an operation over one year after disease onset.2 Since our patient was operated 16 months after wrist and finger drop occurred, the neurolysis and detorsion could still bring benefit. On the other hand, an earlier diagnosis, introduction of oral steroids and operation would likely increase the chance of return of the motor function. As mentioned earlier, the surgery and steroids have been delayed due to the COVID-19 pandemics and direct and intensive involvement of our hospital in the care of infected patients. Our first plan was to make surgical intervention and then to introduce steroids. The operation had to be postponed several times due to necessary admission of COVID-19 patients to the Department of Neurosurgery. Our neurophysiologic team was also engaged in direct care of COVID-19 patients and for a certain period could not deal with COVID-19 negative patients.
In summary, we report a case of unusual presentation of NA with bilateral torsion of radial nerves and with spontaneous, one-sided recovery. Our report underlines the importance of an early diagnosis in NA, which requires HRUS to make correct indication for operative therapy in part of affected patients.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare that they have no conflict of interest.