During surgical admissions, the use of antidopaminergic drugs is associated with increased morbimortality and hospital stay in patients with Parkinson's disease (PD) and other parkinsonisms. We implemented a protocol to ensure adequate perioperative pharmacological management in our center, including educational sessions and complementary tools, such as an electronic Pharmacological Alert and a Patient Information Sheet.
ObjectiveThe objective of this study was to analyze the changes in the prescription of contraindicated medications to PD or parkinsonism patients admitted for surgery, in the three years following implementation of the protocol, and to establish the compliance with the protocol among the medical staff involved in their hospital care over the same period.
MethodsThis is an observational, analytical, prospective study with a before–after design.
ResultsPrescription of contraindicated drugs decreased significantly over the study period (from 57.8% to 20.6%; p<0.001). Patients without an activated Pharmacological Alert had a 13.31 times higher risk of being prescribed contraindicated drugs than patients with such an alert (p<0.001). Neurologists and neurosurgeons used the protocol tools more than Emergency Department surgeons. There was very high compliance with the protocol in admissions for deep brain stimulation and related surgeries.
ConclusionsThe protocol reduced the prescription of contraindicated drugs to PD and parkinsonism patients during their surgical admissions in our center. The Pharmacological Alert and Neurology clinics played a crucial role.
El empleo de fármacos antidopaminérgicos durante los ingresos quirúrgicos se asocia a un aumento de la morbimortalidad y de la estancia hospitalaria en los pacientes con enfermedad de Parkinson (EP) y otros parkinsonismos. Para asegurar un adecuado manejo farmacológico perioperatorio, implementamos un protocolo en nuestro centro, mediante sesiones educativas y varias herramientas complementarias, como una alerta farmacológica electrónica y una hoja de información al paciente.
ObjetivoAnalizar la evolución de la prescripción de los medicamentos contraindicados a los pacientes con EP o parkinsonismo ingresados para cirugía, en los 3 años siguientes a la implantación del protocolo, y establecer el cumplimiento del mismo entre el personal médico implicado en su atención hospitalaria durante el mismo período.
MétodosSe trata de un estudio observacional, analítico y prospectivo, con diseño antes/después.
ResultadosLa prescripción de fármacos contraindicados disminuyó significativamente durante el período de estudio (del 57,8 al 20,6%; p<0,001). Los pacientes sin alerta farmacológica activa tuvieron un riesgo 13,31 veces mayor de que se les prescribieran fármacos contraindicados que los pacientes con dicha alerta (p<0,001). Los neurólogos y neurocirujanos utilizaron más las herramientas del protocolo que los cirujanos del servicio de urgencias. Se produjo un cumplimiento muy elevado del protocolo en los ingresos para estimulación cerebral profunda y cirugías relacionadas.
ConclusionesEl protocolo redujo la prescripción de fármacos contraindicados a los pacientes con EP y parkinsonismo durante sus ingresos quirúrgicos en nuestro centro. La alerta farmacológica y las consultas de neurología jugaron un papel crucial.
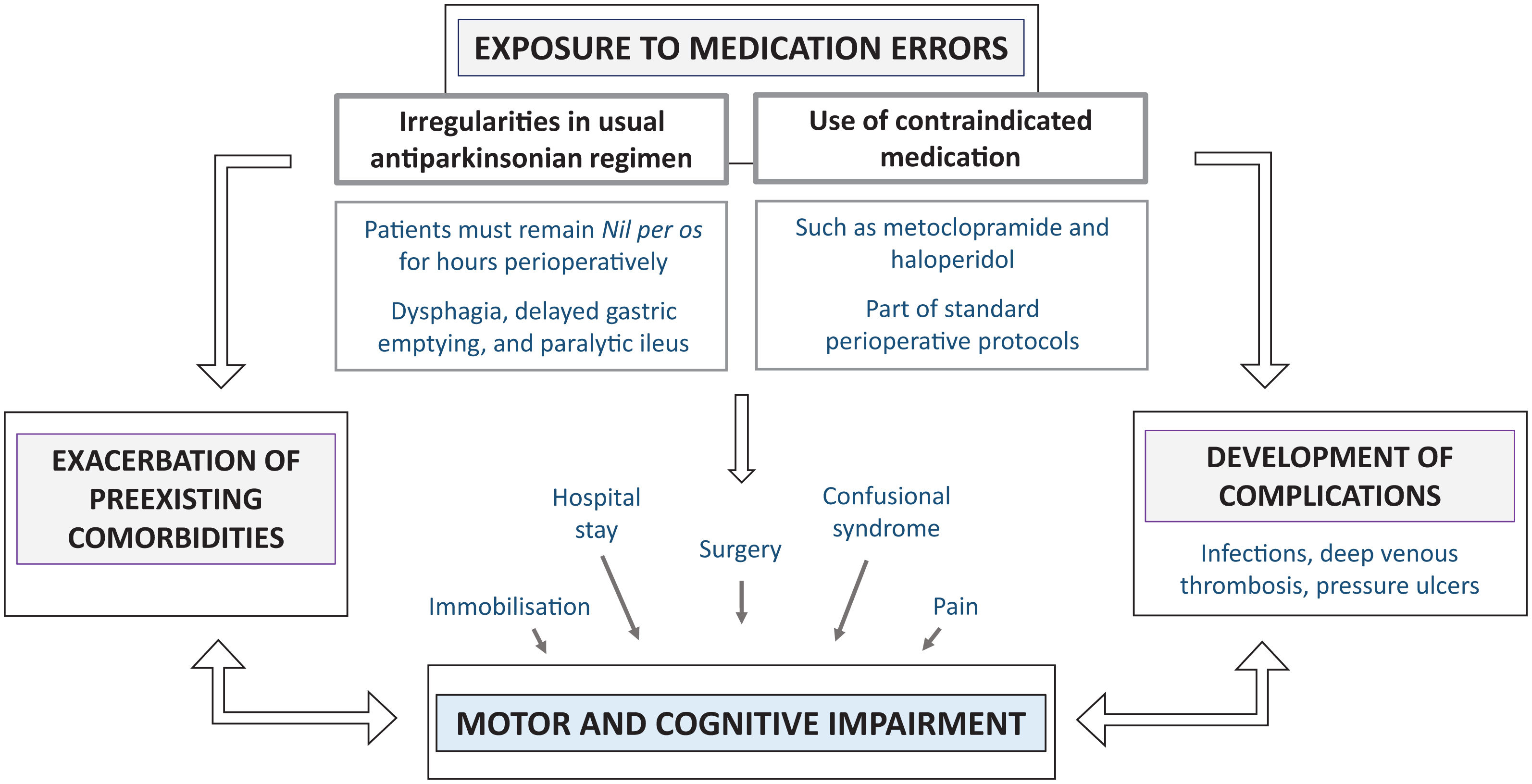
Hospitalizations in PD patients are more frequent1 and prolonged2,3 compared to age-matched control hospitalizations, and increase with patient age and PD progression.4 They are often caused by other comorbidities rather than the PD itself,5 and, regardless of the reason for admission, they are associated with a higher risk of complications.6 In addition, during their hospital stay, medication errors are not uncommon, due to irregularities in the usual antiparkinsonian treatment or the use of antidopaminergic drugs. All these factors contribute to the higher mortality associated with their hospitalizations.7
When these patients are admitted for surgery, the risk of complications and medication errors increases substantially,8 and complex clinical situations can arise (Fig. 1). Indeed, PD constitutes an independent risk factor for prolonged hospital stay and increased morbidity and mortality in patients undergoing surgery.9,10 There is, therefore, ample reason for the development of strategies to increase safety in their hospitalizations, which could have an impact on the patient's clinical status, recovery, and hospital stay duration.7,11 In this regard, general recommendations for pharmacological management have been published.12,13
In December 2015, we introduced a protocol at our center to ensure appropriate pharmacological management during the perioperative period, applicable to all patients with PD or parkinsonism. It details the actions that should be taken at each stage of this period, adapting them to the type of surgery. For its implementation, educational sessions were conducted, and several complementary tools (see electronic supplementary material A) were developed: a Patient Information Sheet, an electronic Pharmacological Alert, an information leaflet for professionals, and a post-operative pain protocol. All information regarding the protocol and complementary tools was available to all professionals on the hospital's internet network. In addition, reminder posters were distributed in Neurosurgery, Neurology, and Anesthesiology clinics, the hospitalization wards of surgical services, and the Emergency Department (ED).
The main objective of the study was to analyze the change in the prescription of contraindicated drugs to PD or parkinsonism patients admitted for surgery, comparing the year prior to the protocol's implementation with the subsequent three years. The secondary objective was to establish the degree of compliance with the protocol among the medical staff involved in these patients’ hospital care, and its change over the same period based on three main indicators: use of protocol tools in Neurology clinics, compliance with the protocol in surgical procedures for deep brain stimulation (DBS), and the medical staff's knowledge of the protocol.
MethodsDesignWe conducted an observational, analytical, prospective study with a before–after design.
Study population and data collectionWe collected the patients’ baseline demographic and clinical variables and admission-related variables and analyzed whether they had received the Information Sheet or had the Pharmacological Alert activated, by reviewing their medical records and the hospital's electronic prescribing program.
Indicators and achievement targetsTo assess the impact of the protocol's introduction, four main indicators were considered. Achievement targets were set for each of these, which in some cases varied depending on the year after implementation, requiring progressively higher compliance.
- 1.
Change in the prescription of contraindicated medications. All patients with a diagnosis of PD or parkinsonism admitted for surgery at the hospital between 2015 and 2018 were included. Both PD-specific (DBS and related surgeries) and general (scheduled or urgent) interventions were considered, excluding diagnostic and/or therapeutic procedures and minor surgeries performed on an outpatient basis. Indicator: the percentage of patients diagnosed with PD or parkinsonism hospitalized for surgery during the year who were prescribed contraindicated medication during admission. Achievement targets: first year after protocol implementation: less than 40%, second year: less than 35%, and third year: less than 25%.
- 2.
Information in Neurology clinics. Patients with a diagnosis of PD or parkinsonism who were attended at the hospital's movement disorders (MD) unit in the third quarter of 2016, 2017, and 2018 were included. Indicator: The percentage of patients with PD or parkinsonism who attended the MD clinics in the third quarter of each year who were provided the Information Sheet or for whom the Pharmacological Alert was activated. Achievement targets: first year: 50%, second year: above 60%, and third year: above 70%.
- 3.
DBS surgery patients managed according to the protocol. All admissions prompted by DBS surgical procedures (both DBS system implantations and generator replacements, as well as interventions due to their complications), were included. Indicator: the percentage of PD patients undergoing DBS or related surgeries, over the course of the year, who were managed according to the protocol. Achievement target: application level above 90%.
- 4.
Awareness of the protocol among physicians. A brief, voluntary and anonymous questionnaire was administered to the Neurology and Neurosurgery staff and to the surgeons from different surgical departments who worked regular hours in the ED one year after implementation of the protocol. Achievement target: the percentage of all physicians involved in the perioperative care of PD patients who participated in the voluntary questionnaire who were aware of and/or had used the protocol should be above 50%.
Descriptive statistics were applied to characterize the variables. Pearson's chi-square test or Fisher's exact test and the chi-square test for a linear trend were used to compare proportions. Binary logistic regression was used to test the independent association of the Pharmacological Alert and the Information Sheet with the absence of prescription of contraindicated drugs. Results with p<0.05 were considered statistically significant.
Ethical considerationsThe Clinical Research Ethics Committee of the Gregorio Marañón General University Hospital evaluated and approved the study. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
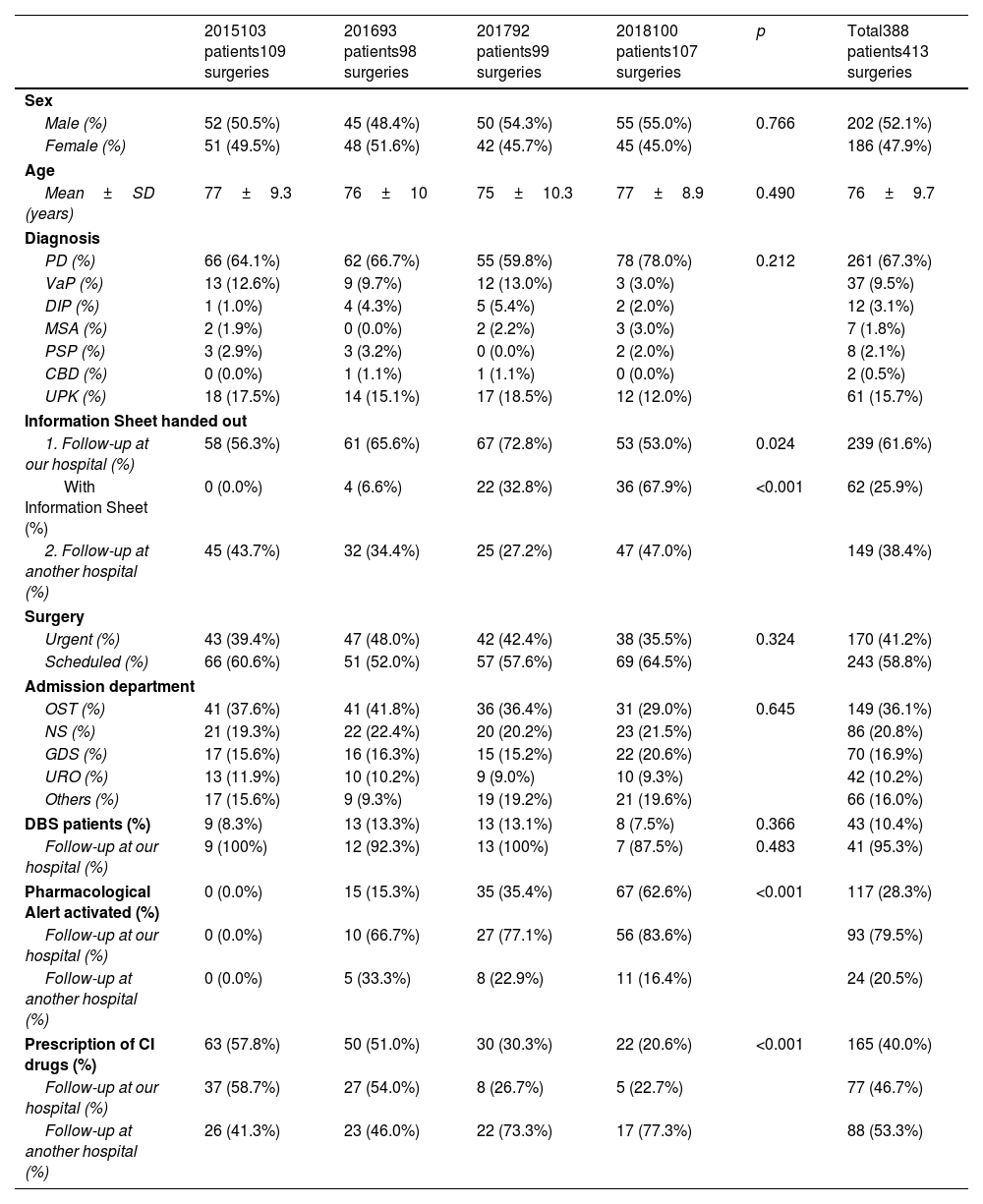
ResultsChange in the prescription of contraindicated medicationsOver the four years of the study, 388 patients with PD or parkinsonism were admitted for surgery, 61.6% of whom were being followed up in the MD unit of our hospital. Their baseline and clinical characteristics and the information regarding their admissions are presented in Table 1.
Baseline and clinical characteristics and information regarding the admissions of patients with PD or parkinsonism during the study period.
| 2015103 patients109 surgeries | 201693 patients98 surgeries | 201792 patients99 surgeries | 2018100 patients107 surgeries | p | Total388 patients413 surgeries | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male (%) | 52 (50.5%) | 45 (48.4%) | 50 (54.3%) | 55 (55.0%) | 0.766 | 202 (52.1%) |
| Female (%) | 51 (49.5%) | 48 (51.6%) | 42 (45.7%) | 45 (45.0%) | 186 (47.9%) | |
| Age | ||||||
| Mean±SD (years) | 77±9.3 | 76±10 | 75±10.3 | 77±8.9 | 0.490 | 76±9.7 |
| Diagnosis | ||||||
| PD (%) | 66 (64.1%) | 62 (66.7%) | 55 (59.8%) | 78 (78.0%) | 0.212 | 261 (67.3%) |
| VaP (%) | 13 (12.6%) | 9 (9.7%) | 12 (13.0%) | 3 (3.0%) | 37 (9.5%) | |
| DIP (%) | 1 (1.0%) | 4 (4.3%) | 5 (5.4%) | 2 (2.0%) | 12 (3.1%) | |
| MSA (%) | 2 (1.9%) | 0 (0.0%) | 2 (2.2%) | 3 (3.0%) | 7 (1.8%) | |
| PSP (%) | 3 (2.9%) | 3 (3.2%) | 0 (0.0%) | 2 (2.0%) | 8 (2.1%) | |
| CBD (%) | 0 (0.0%) | 1 (1.1%) | 1 (1.1%) | 0 (0.0%) | 2 (0.5%) | |
| UPK (%) | 18 (17.5%) | 14 (15.1%) | 17 (18.5%) | 12 (12.0%) | 61 (15.7%) | |
| Information Sheet handed out | ||||||
| 1. Follow-up at our hospital (%) | 58 (56.3%) | 61 (65.6%) | 67 (72.8%) | 53 (53.0%) | 0.024 | 239 (61.6%) |
| With Information Sheet (%) | 0 (0.0%) | 4 (6.6%) | 22 (32.8%) | 36 (67.9%) | <0.001 | 62 (25.9%) |
| 2. Follow-up at another hospital (%) | 45 (43.7%) | 32 (34.4%) | 25 (27.2%) | 47 (47.0%) | 149 (38.4%) | |
| Surgery | ||||||
| Urgent (%) | 43 (39.4%) | 47 (48.0%) | 42 (42.4%) | 38 (35.5%) | 0.324 | 170 (41.2%) |
| Scheduled (%) | 66 (60.6%) | 51 (52.0%) | 57 (57.6%) | 69 (64.5%) | 243 (58.8%) | |
| Admission department | ||||||
| OST (%) | 41 (37.6%) | 41 (41.8%) | 36 (36.4%) | 31 (29.0%) | 0.645 | 149 (36.1%) |
| NS (%) | 21 (19.3%) | 22 (22.4%) | 20 (20.2%) | 23 (21.5%) | 86 (20.8%) | |
| GDS (%) | 17 (15.6%) | 16 (16.3%) | 15 (15.2%) | 22 (20.6%) | 70 (16.9%) | |
| URO (%) | 13 (11.9%) | 10 (10.2%) | 9 (9.0%) | 10 (9.3%) | 42 (10.2%) | |
| Others (%) | 17 (15.6%) | 9 (9.3%) | 19 (19.2%) | 21 (19.6%) | 66 (16.0%) | |
| DBS patients (%) | 9 (8.3%) | 13 (13.3%) | 13 (13.1%) | 8 (7.5%) | 0.366 | 43 (10.4%) |
| Follow-up at our hospital (%) | 9 (100%) | 12 (92.3%) | 13 (100%) | 7 (87.5%) | 0.483 | 41 (95.3%) |
| Pharmacological Alert activated (%) | 0 (0.0%) | 15 (15.3%) | 35 (35.4%) | 67 (62.6%) | <0.001 | 117 (28.3%) |
| Follow-up at our hospital (%) | 0 (0.0%) | 10 (66.7%) | 27 (77.1%) | 56 (83.6%) | 93 (79.5%) | |
| Follow-up at another hospital (%) | 0 (0.0%) | 5 (33.3%) | 8 (22.9%) | 11 (16.4%) | 24 (20.5%) | |
| Prescription of CI drugs (%) | 63 (57.8%) | 50 (51.0%) | 30 (30.3%) | 22 (20.6%) | <0.001 | 165 (40.0%) |
| Follow-up at our hospital (%) | 37 (58.7%) | 27 (54.0%) | 8 (26.7%) | 5 (22.7%) | 77 (46.7%) | |
| Follow-up at another hospital (%) | 26 (41.3%) | 23 (46.0%) | 22 (73.3%) | 17 (77.3%) | 88 (53.3%) | |
SD: standard deviation; PD: Parkinson's disease; VaP: vascular parkinsonism; DIP: drug-induced parkinsonism; MSA: multiple system atrophy; PSP: progressive supranuclear palsy; CBD: corticobasal degeneration; UPK: unspecified parkinsonism; OST: Orthopaedic Surgery and Traumatology; NS: Neurosurgery; GDS: General and Digestive Surgery; URO: Urology; others (includes Gynecology, Cardiac Surgery, Vascular Surgery, Thoracic Surgery, Maxillofacial Surgery, Plastic Surgery, Otorhinolaryngology, and Dermatology); DBS: deep brain stimulation; CI: contraindicated.
A total of 413 surgeries were performed, with no significant differences between the different years in either the type of intervention (p=0.324) or the frequency of admission to the different surgical departments (p=0.645), the main ones being Orthopedic Surgery and Traumatology (36.1%), Neurosurgery (20.8%), and General and Digestive Surgery (16.9%). No differences were observed in the percentage of patients with DBS (10.4% of surgeries) (p=0.366), of whom 95.3% were being followed up at our center.
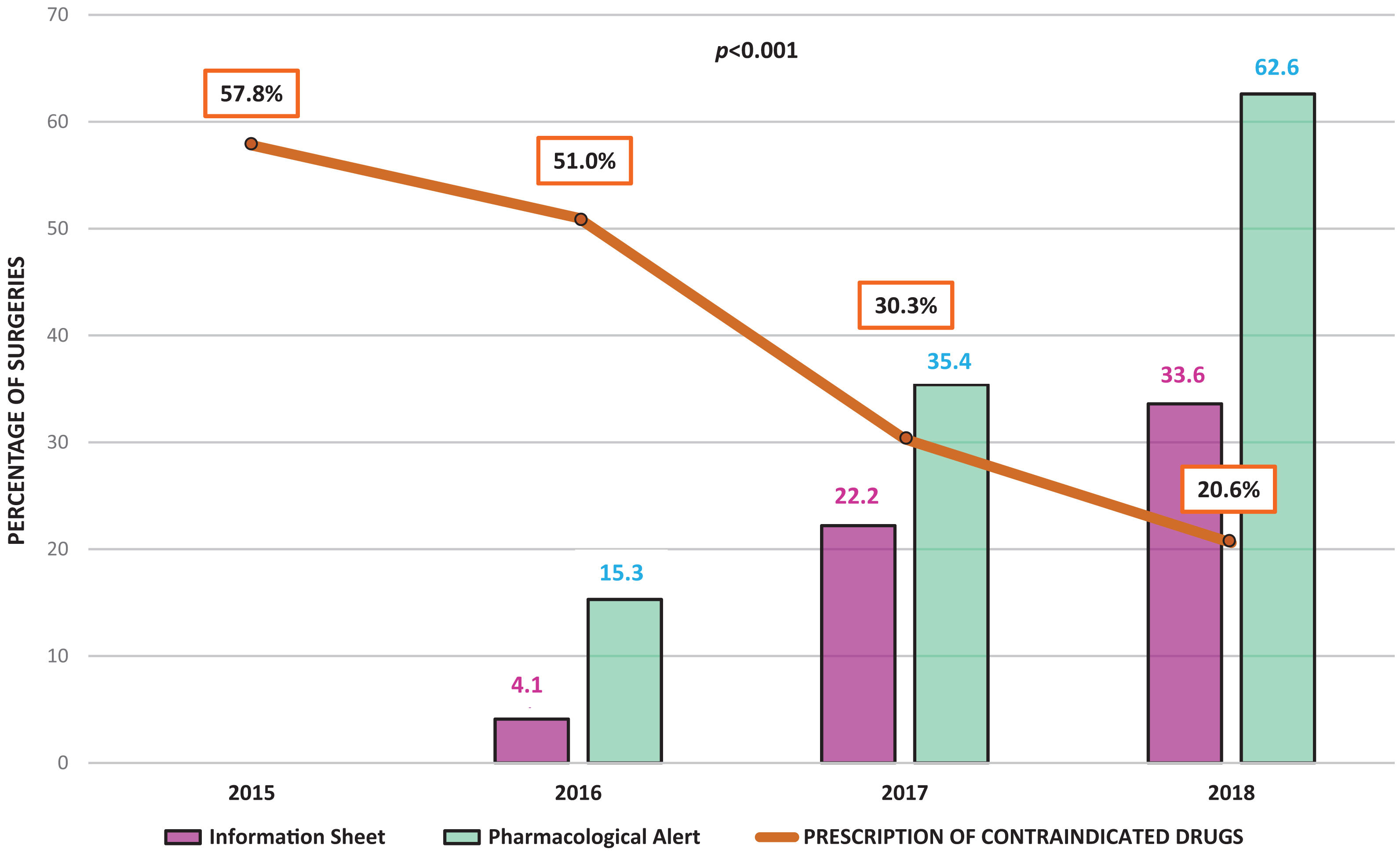
Over the study period, there was a progressive increase in the percentage of patients admitted for surgery who had already received the Information Sheet during follow-up, from 6.6% in 2016 to 32.8% in 2017 and 67.9% in 2018 (p<0.001). Thus, the percentage of surgical admissions in which the patient already had the Information Sheet rose from 4.1% to 22.2% and 33.6%, respectively. Use of the Pharmacological Alert also increased, with more and more patients admitted for surgery having the Alert activated in the prescription program, from 15.3% of surgeries in 2016 to 35.4% in 2017 and 62.6% in 2018 (p<0.001). The follow-up at our hospital MD unit was associated with a higher frequency of activated Pharmacological Alerts from 2017 onwards. In 2016, 66.7% of the activated Alerts corresponded to patients followed up at our hospital versus 33.3% to patients from other centers (p=0.841). In 2017, 77.1% versus 22.9% (p=0.005), respectively, and in 2018, 83.6% versus 16.4%, respectively (p<0.001).
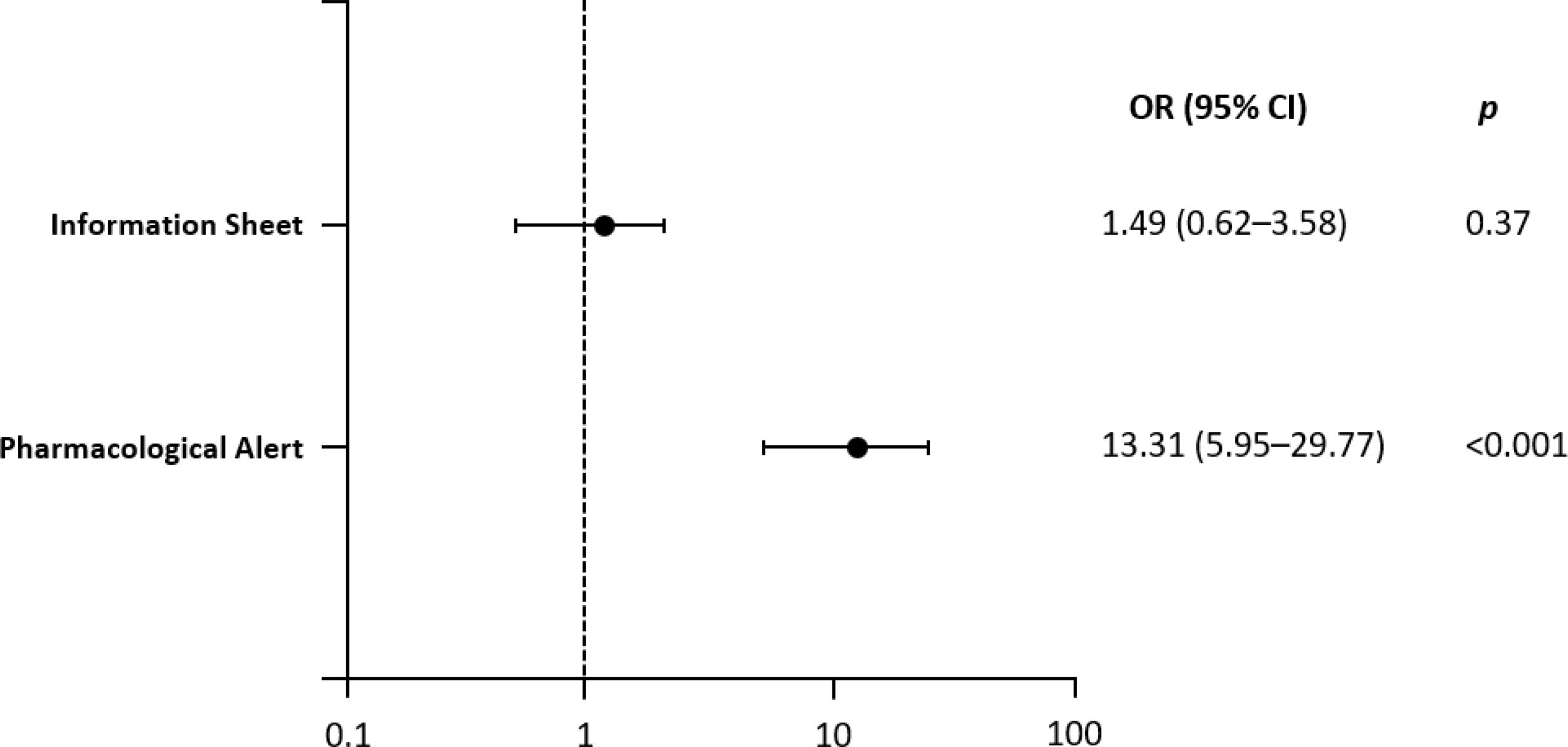
In 2015, contraindicated drugs were prescribed in 57.8% of admissions, which decreased to 51.0% in 2016, 30.3% in 2017, and 20.6% in 2018 (p<0.001) (Fig. 2). The main contraindicated drugs prescribed were metoclopramide, haloperidol, risperidone, and olanzapine. Of the admissions in which contraindicated drugs were prescribed in 2018, 22.7% corresponded to patients monitored in the hospital and 77.3% to patients from outside the center (p=0.001). Patients without an activated Pharmacological Alert had a 13.31 times higher risk of being prescribed contraindicated drugs than patients for whom it had been activated (OR=13.31 [95% CI 5.95–29.77], p<0.001) (Fig. 3).
Out of a total of 808 patients with a diagnosis of PD or parkinsonism, 269, 228, and 311 patients were attended to in the MD unit in the last quarter of 2016, 2017, and 2018, respectively. Their full demographic and clinical characteristics are presented in electronic supplementary material B.
The percentage of patients in possession of the Information Sheet increased from 13% in 2016 to 57% in 2017 and 76.2% in 2018 (p<0.001). The percentage of patients with an activated Pharmacological Alert increased from 29% in 2016 to 60.1% in 2017 and 90.7% in 2018 (p<0.001).
DBS surgery patients managed according to the protocolBetween 2016 and 2018, a total of 38 DBS-related interventions were performed. The full demographic and clinical characteristics of the 34 operated patients and the information about their admissions are presented in electronic supplementary material C. There were no significant differences between years in terms of the frequency of surgeries (p=0.493); the most frequently performed were generator replacements (63.2%), followed by DBS system implantations (26.3%). Surgeries performed for complications accounted for 10.5%. There was very high compliance with the protocol with regard to the management of antiparkinsonian treatment and the anesthetic and perioperative pain management (100%). The percentage of DBS interventions in which the patient had received the Information Sheet increased from 6.7% in 2016 to 35.7% in 2017 and 100% in 2018 (p<0.001). Similarly, the percentage of surgeries in which the patient had the Pharmacological Alert activated increased from 20.0% in 2016 to 85.7% in 2017 and 100% in 2018 (p<0.001).
Awareness of the protocol among physiciansThe questionnaire was completed by 23 neurologists, 11 neurosurgeons, and 38 physicians from different surgical departments (electronic supplementary material D). The target was met in all of the surveyed departments. Most participants stated that they were aware of the existence of the protocol (87.0% in Neurology, 81.8% in Neurosurgery, and 63.2% in the ED), although use of the protocol tools was higher among neurologists (65.2%) and neurosurgeons (63.6%) compared to ED surgeons (31.6%).
A summary figure of the achievement targets is presented in electronic supplementary material E.
DiscussionChange in the prescription of contraindicated medicationsThe sample of patients admitted for surgery at our center throughout the study is fairly representative of the profile of patients with PD or parkinsonism most frequently admitted according to the literature, as they were of advanced age2,4 and with a slight predominance of the male sex.5 In line with previous publications, the most frequent admission department was Orthopedic Surgery and Traumatology.3 Ophthalmological and urological surgeries, which are very common in PD,12 were under-represented due to the exclusion of outpatient procedures. In light of the presence of a multidisciplinary Functional Neurosurgery in Movement Disorders team at the center, it is not surprising that the second most frequent department was Neurosurgery, and that 10.4% of the interventions were performed on patients already undergoing DBS therapy.
Achieving such a significant reduction in the prescription of contraindicated drugs is of great relevance in routine practice. Among the medication errors that occur in hospital settings, prescription errors are known to be the errors most frequently related to adverse events.14 Specifically, in PD patients, medication errors have been identified as one of the main predisposing factors to motor impairment during admissions,15 even more so than infections.6 In particular, the administration of contraindicated drugs has been associated with longer hospital stay7,11 and increased mortality, as much as or more than the incorrect administration of antiparkinsonian treatment.7 Considering the frequency with which contraindicated drugs are used in PD in surgical admissions,8 the observed decrease in their use is of even greater significance. The results are also noteworthy due to the inherent difficulty of implementing protocols in tertiary centers with a large number of professionals belonging to different departments and a high volume of care processes.16 To date, most studies assessing the prescription of contraindicated drugs during admissions of PD patients have included hospitalizations in medical and surgical services.7 To our knowledge, the only study to date focusing solely on surgical admissions was published by Derry et al.,8 in which the prescription of contraindicated drugs affected up to 41% of patients. In line with our data before implementation of the protocol (with contraindicated drugs prescribed in 57.8% of admissions), both data sets point to the magnitude of the problem.
Multiple measures have been proposed to improve the pharmacological management of patients with PD or parkinsonism during their admissions. These include educational measures, focused both on patients17 and professionals.18 In this regard, our protocol included distribution of the Information Sheet and training patients during patient appointments, as well as educational sessions for professionals, accessible protocol documents, and posters distributed throughout the hospital. Various surveillance and prevention interventions have also been proposed, such as systems for reporting admissions of these patients to the corresponding specialists,19 specialized units for monitoring them during their hospitalization,20 the creation of alarms for nurses for the timely administration of their treatments,21 or involvement of the Hospital Pharmacy in the validation of prescriptions18 and optimization of medications.22 In our protocol, the Pharmacy unit was involved in the development of the protocol and the creation of the Pharmacological Alert in the electronic prescription program.
Computer-based interventions have gained particular prominence among the measures aimed at preventing medication errors in PD,23,24 and our Pharmacological Alert is a good example of this as it proved to be highly effective in reducing the prescription of contraindicated drugs. Other studies that have analyzed the impact of PD electronic alert interventions have obtained mixed results. In the recent publication by Aslam et al.,25 the authors combined a series of training activities with a computer alert that notified the Pharmacy unit upon admission of patients with a diagnosis of PD or upon treatment with dopaminergic drugs. They observed a reduction in the prescription of contraindicated drugs (from 42.5% to 17.5%, p<0.001). This sharp reduction contrasts with our results, which is probably related to the pharmacists’ role in the study, who reviewed the prescribed medication and generated an alert when antidopaminergic drugs were prescribed. Other differences include a smaller sample size, a shorter follow-up time, inclusion of admissions to medical services, and exclusion of patients admitted for PD-specific surgeries. The study published by Morris et al.26 was based on an alert in the prescribing program that was generated when dopamine receptor antagonist drugs were prescribed for patients admitted under treatment with dopamine agonists. Of the total number of prescriptions of antidopaminergic drugs, 83.1% were inappropriate, and of these, 74.1% were maintained despite the alert. One possible explanation for the greater effectiveness of our alert is its configuration as a drug allergy; when active, the patient is recorded as being allergic to the group “Drugs contraindicated in Parkinson's disease”. The combination with training measures for professionals, the accessibility of the protocol on the hospital's computer network, and the possibility of contacting the Neurology unit by telephone throughout the day (which was emphasized in the training sessions, in the protocol documents, and on the information posters) to find out about safe treatment alternatives, could also have played a role.
The follow-up in the MD unit of our center acted as a protective factor against the prescription of contraindicated drugs, due to the activation of the Pharmacological Alert and patient education supported by the Information Sheet. This highlights the importance of compliance with the protocol in Neurology clinics. However, the protocol may also be beneficial for patients coming from other hospitals, as long as the professionals attending them use its tools.
Information in Neurology clinicsThe sample is representative of the population usually treated in MD units, with elderly patients, a large majority of PD patients, a low percentage of other primary and secondary parkinsonisms, and approximately 15% of patients with DBS, with no differences between years (p=0.487). There was a significant increase in the use of the protocol tools over the study period, especially from the second year onwards. This was to be expected, given that incorporating new tools into routine practice is usually gradual and consolidates over time.
Patient education is critical because appropriately informed patients (or their caregivers) can assume a leading role in their own safety during admission. Previous studies17 have demonstrated that patient education can improve the timing of administration of antiparkinsonian treatment. Most of the patients admitted for surgery during the study were receiving follow-up in our hospital, so they could aware of the importance of correct pharmacological management to the healthcare staff and show them the Information Sheet. We cannot compare our results with previous studies because, to our knowledge, no similar work has been published to date.
DBS surgery patients managed according to the protocolA very high compliance rate was observed for all admissions due to DBS-related interventions since the protocol was implemented. This is not surprising given the high level of specialization of the professionals involved in the perioperative period of these surgeries, and their awareness of the complications associated with medication errors. Along with other factors, it may also influence the short duration of these admissions,20 with a majority of patients discharged home,27 unlike other surgical admissions, where referral to centers for care or rehabilitation is not uncommon.28
To our knowledge, this is the first study to evaluate the impact of a specific perioperative management protocol for DBS surgery on the pharmacological management of such patients. None of the patients received contraindicated medications. Ensuring adequate pharmacologic management facilitates DBS programming, as the use of antidopaminergic drugs can worsen PD symptoms and hinder the patient's clinical evaluation.29
Awareness of the protocol among physiciansThe differences in the use of the protocol tools observed in the questionnaire are probably due to the fact that neurologists and neurosurgeons received more specific training when the protocol was implemented, and they are the physicians most closely involved with these patients. The lower awareness and use of the protocol by ED surgeons is probably due to less contact with PD patients in their routine practice.8 Although the achievement targets were met, the results could be considerably better and point to the need to improve the training of professionals and their knowledge of the protocol. Widespread use of the protocol in the hospital, beyond Neurology clinics, would undoubtedly increase the impact on the safety of these patients and the quality of their care.
The protocol includes indications for the appropriate management of antiparkinsonian treatment in surgical admissions. Evaluating this aspect is complicated when many patients are followed up by Neurology in other centers, but it is something that must necessarily be analyzed in the future. To promote compliance with their antiparkinsonian regimen, it is essential to continue training professionals, who, following the protocol, will prescribe their usual treatment, adapting it to the type of surgery, stopping it and resuming it when appropriate. The reinforcement training sessions should begin with the surgical services to which these patients are most frequently admitted, and should be extended to services such as ED, Internal Medicine and Geriatrics, given that the use of the protocol tools can also be useful in their medical admissions. To ensure compliance with the protocol, a team of neurologists could be assigned to review the treatment of all patients with an activated Alert who are admitted to surgical services. In addition, the Hospital Pharmacy could also prioritize the review of the treatment of patients with such an Alert, ensuring the availability of their antiparkinsonian medications in the hospital and the absence of contraindicated drugs prescribed. Complementary electronic tools could also be created. In patients with the Pharmacological Alert activated, the program could ask the physician whether the patient's antiparkinsonian treatment has been prescribed and, if a contraindicated drug has been included, it could directly propose a list of safe alternatives. Finally, the use of the protocol tools will be reinforced in the Neurology Department, and compliance with the protocol will continue to be periodically analyzed.
The main limitations of this study are its single-center nature and the exclusive use of electronic prescription records (there could have been verbal prescriptions that were not recorded, although this is very rare nowadays). Its strengths are its prospective design and its development in a tertiary hospital with a large number of professionals and a large sample of patients. In addition, the analysis was performed on the contraindicated medications prescribed, regardless of their final administration. The results are novel because, to our knowledge, this is the first study to include the development of a specific management protocol that also covers DBS-related surgeries, to establish its impact on contraindicated medications, and to assess the physicians’ knowledge.
ConclusionThe implementation of a perioperative management protocol for PD patients in our center has significantly reduced the prescription of contraindicated drugs to patients with PD or parkinsonism during their surgical admissions. The Pharmacological Alert in the electronic prescribing program played a crucial role. DBS surgeries showed high compliance with the protocol. Neurology clinics are an essential element for the functioning of the protocol in the hospital.
Ethical approvalThe study was approved by the Clinical Research Ethics Committee of the Gregorio Marañón General University Hospital (PR-PRP-01).
FundingThe Movement Disorders Study Group of the Madrid Association of Neurology supported this work [Research Grant, 2017]. We used funding for English editing services of the final manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
To all the healthcare professionals who contributed to the development and implementation of the protocol and to all those who are actively using it at present to improve patient safety.