Fibromyalgia (FM) is a chronic condition defined by widespread body pain, tenderness to palpation of tender point areas, and constitutional symptoms. The diagnosis of FM is based on the classification criteria of the American College of Rheumatology, it is usually made between the ages of 20 and 50 years and is more prevalent in women.1 Migraine has been diagnosed in 63% of FM patients presenting with headache, hence, potential links between FM and headache have been described.1,2 Pregabalin is an antiepileptic drug used in the management of chronic pain conditions such as FM. A Cochrane analysis of randomized controlled trials showed that doses ranging from 300 to 600mg of pregabalin were associated with a reduction in pain intensity over 12–26 weeks when compared with a placebo in FM patients with moderate or severe pain. Tolerable adverse events such as dizziness, somnolence, weight gain, and peripheral edema were observed in a small proportion of patients.3
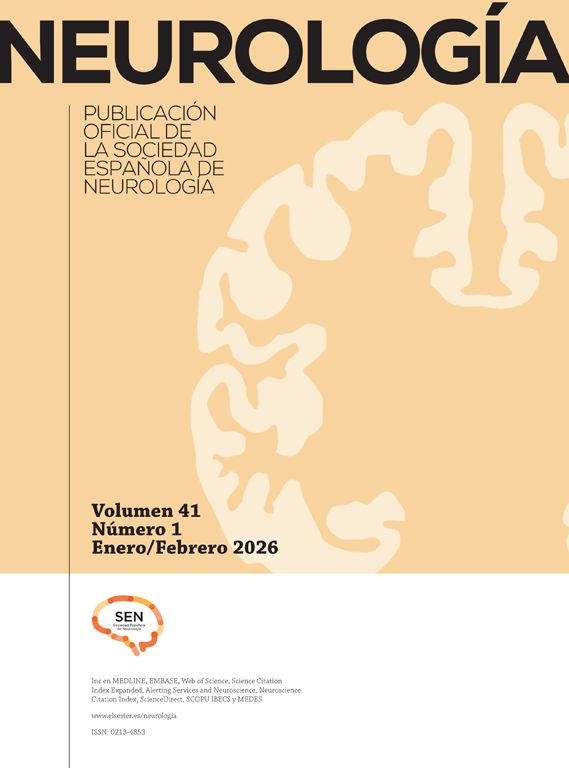
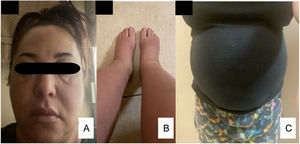
A 50-year-old woman with a 15-year history of migraine without aura and widespread body pain was diagnosed with FM in 2005, she began treatment with pregabalin 75mg twice a day and zolmitriptan 2.5mg as needed for headache. The patient attended our outpatient clinic for several years and remained in reasonable pain control with 150mg pregabalin daily. In 2013 she had an FM crisis that was treated with tramadol and desvenlafaxine for a three-month period after which she continued with the original 150 pregabalin daily dose. In 2016 a crisis of FM, arterial hypertension, and insomnia was precipitated by her divorce. At that time pregabalin was increased to 75mg three times daily and Valsartan/Hydrochlorothiazide 80mg/12.5mg/day was initiated. In October 2020, due to relapses of FM, she decided to obtain a second opinion with a rheumatologist who increased her pregabalin dose to 150mg three times a day. One month later, the patient returned to our clinic due to a 15kg weight gain, severe generalized pitting edema (3+), and symptomatic hypotension (Fig. 1). We assessed renal, hepatic, and cardiac function laboratories as well as performed a thoracoabdominal CT, a transthoracic echocardiogram, chest X-ray, and arterial and vein ultrasounds of the four limbs. All these studies were within normal ranges. Pregabalin was discontinued and after 6 weeks, the patient returned to her baseline weight and the generalized edema disappeared (Fig. 2).
Pregabalin's mechanism of action is binding to the α2δ subunit of presynaptic voltage-gated calcium channels in presynaptic neurons, thereby reducing the release of the excitatory neurotransmitter glutamate.4 Peripheral edema and worsening of heart failure symptoms have been reported with the use of pregabalin for neuropathic pain.4,5 These effects may be the result of the antagonism of L-type calcium channels in the vasculature causing vasodilation, similar to the mechanism of calcium channel blockers used to treat hypertension.4 L-type calcium channels are widely distributed in the smooth muscle cells of peripheral arteries, their blockage dilates the systemic vasculature, substantially reducing blood pressure and may cause edema. In this patient, generalized edema was observed when the daily dose of pregabalin was increased from 150mg to 450mg. The recommended daily dose of this drug for the treatment of FM ranges from 300 to 600mg.3 The peripheral edema as an adverse event increases with the patient's age and is dosage-dependent. It has been observed in 15% of older patients and in 7.6% of those younger than 64 years.6 The peripheral edema increases from 3.7% in pregabalin doses ≤150mg/day to 11.5% in doses ranging from 300 to 600mg/day.6 In our patient, the generalized edema and the arterial hypotension were results of the dosage increment of pregabalin and the subsequent vasodilation due to the drug's antagonism of the L-type calcium channel in the vasculature. Ethnic pharmacokinetics and pharmacodynamic differences between populations may be the origin of the susceptibility to develop this dose-dependent generalized edema in our patient. To our knowledge, pregabalin-induced severe generalized edema has not been reported in the literature and is prone to be unrecognized as an adverse effect of this drug.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestAll authors declare no compelling conflicts of interest.