Functional movement disorders (FMD) are challenging to diagnose and constitute a frequent cause of neurological disability.1–3 Diagnosis requires numerous specialists and considerable healthcare resources, which results in considerable diagnostic delays and distress for patients.4 In the case of psychogenic non-epileptic seizures, early diagnosis assists in treatment and improves prognosis.5,6
We present the case of a 67-year-old woman with history of poliomyelitis, which resulted in paresis of the right lower limb and severe osteoporosis, leading to multiple bone fractures. A year previously, she was diagnosed with chronic kidney disease secondary to Goodpasture syndrome. She was started on haemodialysis; a humero-axillary arteriovenous fistula was created in the right arm for that purpose. In the months following surgery, the patient was admitted to hospital due to haematoma and bleeding in the right arm. Five months after the intervention, she presented pain in the right elbow, radiating to the hand and associated with impaired movement; symptoms presented exclusively during dialysis. A Doppler ultrasound ruled out ischaemic steal syndrome. The pain resolved several days later, and the patient started to present tonic contractions of the right forearm and hand, starting several seconds after the dialysis machine was switched on and appearing only during haemodialysis. Electrolyte levels (Na+, K+, Cl−, Ca2+, and Mg2+) were within normal ranges. A neurophysiological study of peripheral nerves was performed during dialysis. A physical examination performed during the procedure revealed normal colouration, hypoaesthesia with no defined distribution, rigidity, and contraction of hand and forearm muscles, with no associated pain or emotional component. Opposition movement was observed when trying to open the hand; muscle tone fluctuated with distraction movements, and wrist flexion was slow and discontinuous. As these results are suggestive of FMD,3 we decided to suspend haemodyalisis and perform an induction test combined with a neurophysiological study with surface electromyography (EMG) (Elite®, Cadwell Industries, Inc.; Kennewick, USA).7
For the induction test, 2 contact electrodes were placed on the ipsilateral supraclavicular region, and the patient was informed that she would receive electric stimulation. We administered trains of continuous monophasic pulses at 30Hz for 100μs, increasing the intensity to 5mA. After several seconds, the patient presented an episode of similar characteristics to those described previously; the EMG study revealed irregular, non-specific changes in muscle tone with distraction movements. The episode resolved several seconds after electric stimulation was stopped.
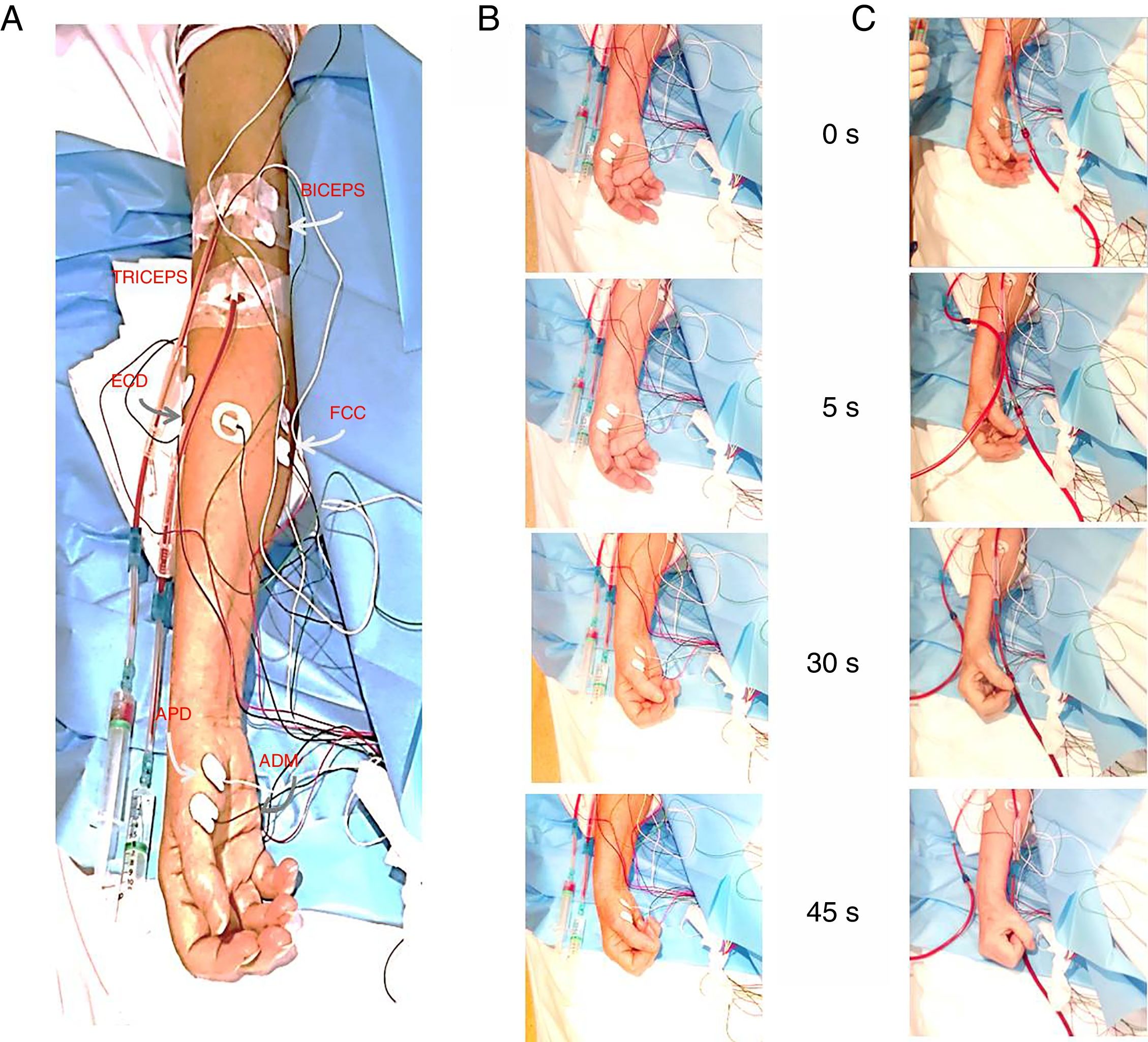
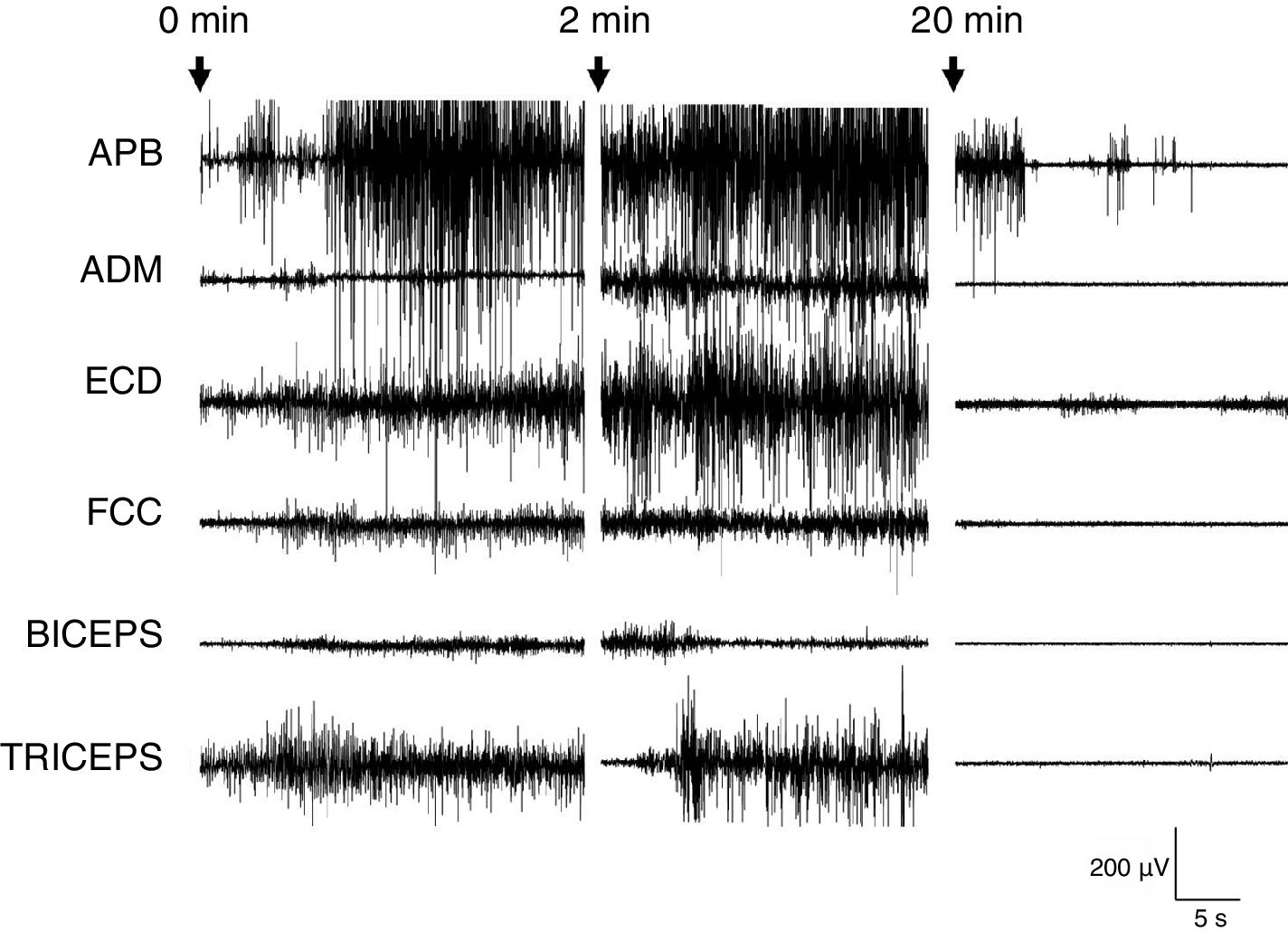
Haemodialysis was resumed (Fig. 1), and EMG continued for 120minutes; the patient presented another episode. The recording showed no sustained increase in muscle tone of over a minute, and revealed fatigability: during the last 60minutes, muscle activity was mostly normal, with short-lasting increases in muscle tone, particularly in the flexors of the forearm and in muscles of the hand (Fig. 2).
Neurophysiological study. A) Location of adhesive electrodes on the biceps, triceps, extensor digitorum, flexor digitorum, thenar eminence, and abductor digiti minimi muscles of the right arm. B) Sequence of clinical manifestations during the induction test. C) Sequence of clinical manifestations during haemodialysis. The numbers indicate the time elapsed (seconds) since onset of the induction test/haemodialysis. ADM: abductor digiti minimi; APB: abductor pollicis brevis; ED: extensor digitorum; FDP: flexor digitorum profundus.
The patient was referred to the psychiatry department with a diagnosis of FMD. The patient received 5 sessions of psychotherapy, where she was informed about her diagnosis and the psychological mechanisms contributing to the pathogenesis of FMD were identified.8 She was taught a series of stress-coping strategies and relaxation techniques. Psychotherapy achieved complete remission of the FMD, and the patient recovered her functional status and subjective quality of life.
Diagnosis of FMDs is based on the presence of clinically inconsistent findings during the physical examination.3 In any case, diagnosis is often challenging, with a risk of inter-rater variability.3,9 The diagnostic criteria for functional tremor and myoclonus have been established, and diagnosis of these entities should be based on neurophysiological findings.10 Dystonia is the most challenging FMD to diagnose. Neurophysiological studies are useful since they provide objective results.11,12 In the case of dystonia, however, they are difficult to perform since the patient is not relaxed, and only surface EMG can be performed.1 Induction tests for psychogenic non-epileptic seizures have 30% sensitivity and up to 90% specificity.13 In our patient, the ability to trigger an episode with an induction test and the results of the physical examination and neurophysiological study enabled early diagnosis of FMD, which is associated with better prognosis as it enables early psychological treatment.14,15
FundingThis study was funded by the Spanish Ministry of Health (Institute of Health Carlos III research funds, project no. PI17/02193) and the European Regional Development Fund.
Please cite this article as: Vega-Zelaya L, Ezquiaga E, Giogi González M, Pastor J. Prueba de inducción con maniobra no fisiológica para el diagnóstico en un caso de trastorno de movimiento de origen funcional. Neurología. 2020;35:579–581.