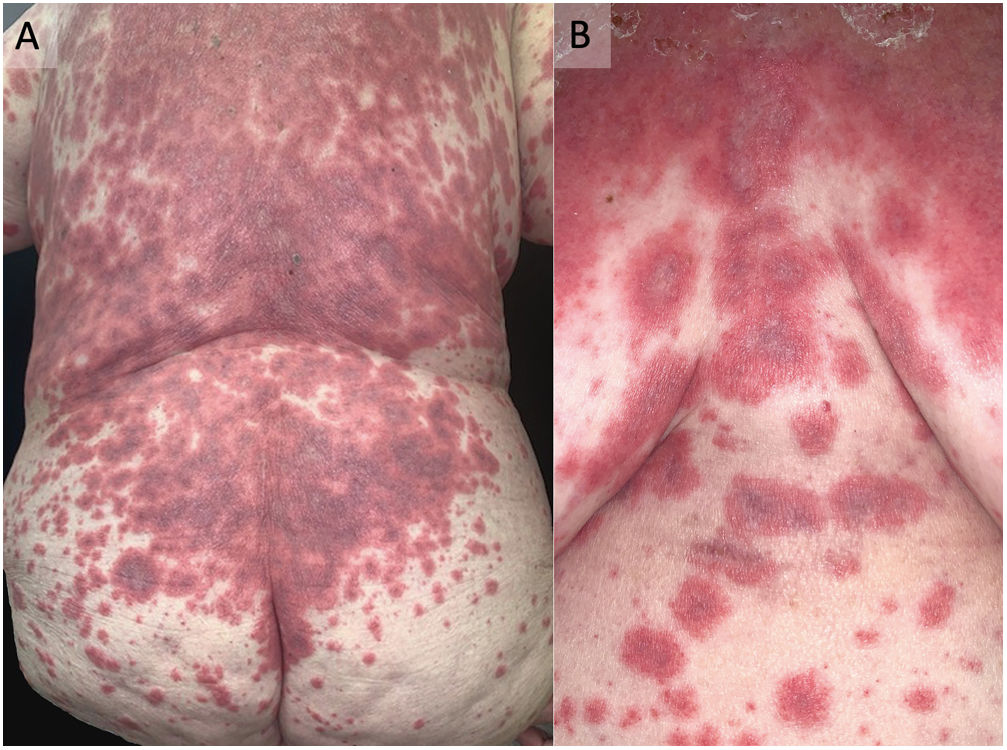
An 85-year-old woman presented with erythematous-violaceous plaques on her neck, back, and chest. She reported a recent 3-week history of hydroxychloroquine intake for the management of a rheumatic condition. The clinical examination revealed erythematous patches with confluent growth and cephalocaudal projection. These patches (Fig. 1) exhibited a strikingly atypical targetoid appearance, characterized by irregular borders and the presence of two concentric rings, often with a grayish or violaceous center. Importantly, there was no involvement of mucous membranes or other systemic symptoms. Suspecting Stevens-Johnson Syndrome (SJS), the patient was promptly hospitalized, and hydroxychloroquine was discontinued. A skin biopsy was performed, revealing keratinocyte necrosis, both individually and in extensive areas, subepidermal blister, and mild superficial perivascular lymphohistiocytic infiltration. High-dose corticosteroid treatment was initiated. Over a 10-day hospitalization, the patient showed improvement, with no new lesions or cutaneous detachment. The initially alarming lesions evolved to a lighter, evanescent red color.
Lesions at the time of consultation – atypical target lesions were observed on the posterior and anterior trunk. These lesions exhibited a distinctive appearance characterized by irregular borders, a reduced number of concentric rings, and a central area displaying a grayish hue. The recognition of these unique atypical targets was pivotal for the accurate diagnosis of Stevens-Johnson Syndrome.
The presented case emphasizes the importance of early recognition of atypical target-like lesions in Stevens-Johnson Syndrome (SJS) and underscores the need for timely referral to a dermatologist. SJS is a severe and potentially life-threatening condition, with mortality rates ranging from 10% to 30% among affected patients.1 In many cases, it is triggered by medications, as was the case with the patient who had been taking hydroxychloroquine.
The atypical presentation of target-like lesions, with irregular borders and two concentric rings, challenges the conventional diagnostic criteria for SJS, which often focus on the classic three concentric rings seen in erythema multiforme. A skin biopsy is usually recommended in cases of suspected Stevens-Johnson Syndrome to confirm the diagnosis through histopathological assessment of skin changes, including epidermal necrosis and other characteristic findings. It is crucial to have this evaluation conducted by a pathologist experienced in dermatopathology for accurate results.3
This atypical presentation can lead to diagnostic delays, as physicians may not immediately associate it with SJS.2 Delayed diagnosis can have grave consequences, as it allows the condition to progress to a more severe stage, increasing the risk of systemic involvement and higher mortality rates.1,3
Therefore, it is crucial for healthcare professionals, especially primary care physicians, to be aware of the diverse clinical presentations of SJS, including these atypical lesions. Any suspicion of SJS should prompt immediate referral to a dermatologist for further evaluation and management.4 Prompt recognition and discontinuation of the causative agent, such as the implicated medication, along with early initiation of appropriate treatment, can greatly improve the patient's prognosis and minimize the risk of complications associated with this condition.1,3,4 In conclusion, timely recognition and referral play a vital role in preventing the devastating consequences of SJS.
Informed consentOral and written consent was obtained to publish this image.
Ethical approvalProcedures followed here were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 1983. We have not use patients’ names, initials, or hospital numbers.
Authors’ contributionsMiguel Mansilla-Polo and Carlos Abril-Pérez managed clinical treatment and procedures, contributing to the development of this paper.
Daniel Martín-Torregrosa supervised the work.
All authors had access to the data and played a role in writing this manuscript.
FundingThis article has no funding source.
Conflicts of interestThe authors have declared no conflicts of interest.