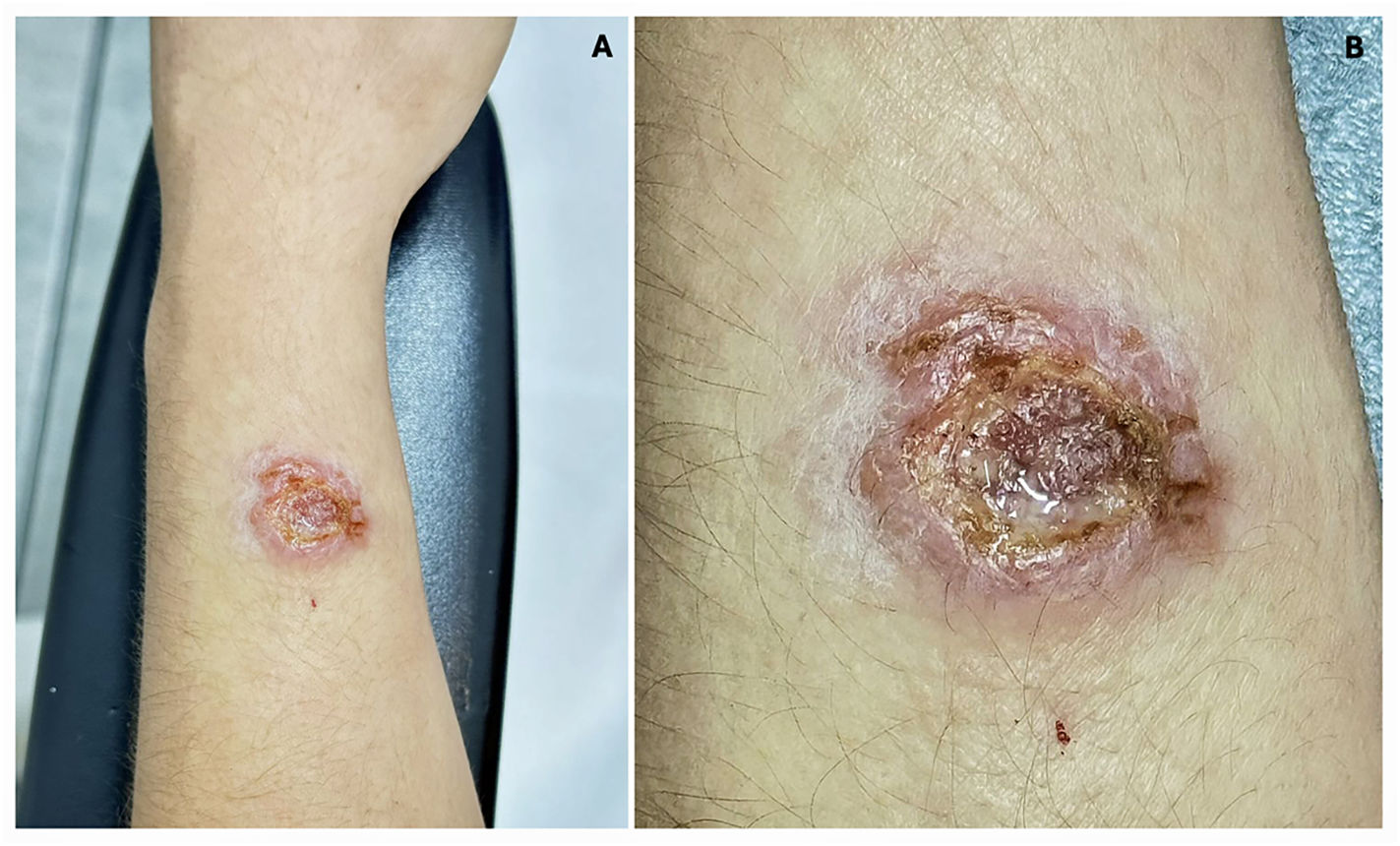
A 22-year-old female Venezuelan immigrant presented to our dermatology clinic with a painful, non-healing ulcer on her left forearm that had persisted for 12 months. She had previously received multiple topical and systemic treatments without clinical improvement. Physical examination revealed a well-circumscribed ulcerative lesion with erythematous and indurated borders, and a necrotic-purulent base (Fig. 1A and B). Laboratory investigations demonstrated the presence of anti-Leishmania antibodies, and polymerase chain reaction (PCR) analysis of the tissue sample confirmed Leishmania infantum DNA. Histopathological examination revealed epidermal ulceration with dermal edema and a compact, nodular granulomatous infiltrate composed of multinucleated giant cells, histiocytes, and lymphocytes. Based on these findings, a diagnosis of cutaneous leishmaniasis was established. The patient was treated with intralesional sodium stibogluconate in combination with CO₂ laser therapy, resulting in progressive healing and a favorable clinical outcome.
Ethical considerationPatient written informed consent was obtained.
FundingThere was no funding or financial support in the creation of this clinical image.
Ethical committeeComité de Investigación de la UDEM.
Registry number18092024-CARD-CI.
None.