Mumps is characterized by parotid inflammation and fever and is preventable by vaccination with MMR vaccine. The objective of the study is to assess the impact and effectiveness of the vaccine.
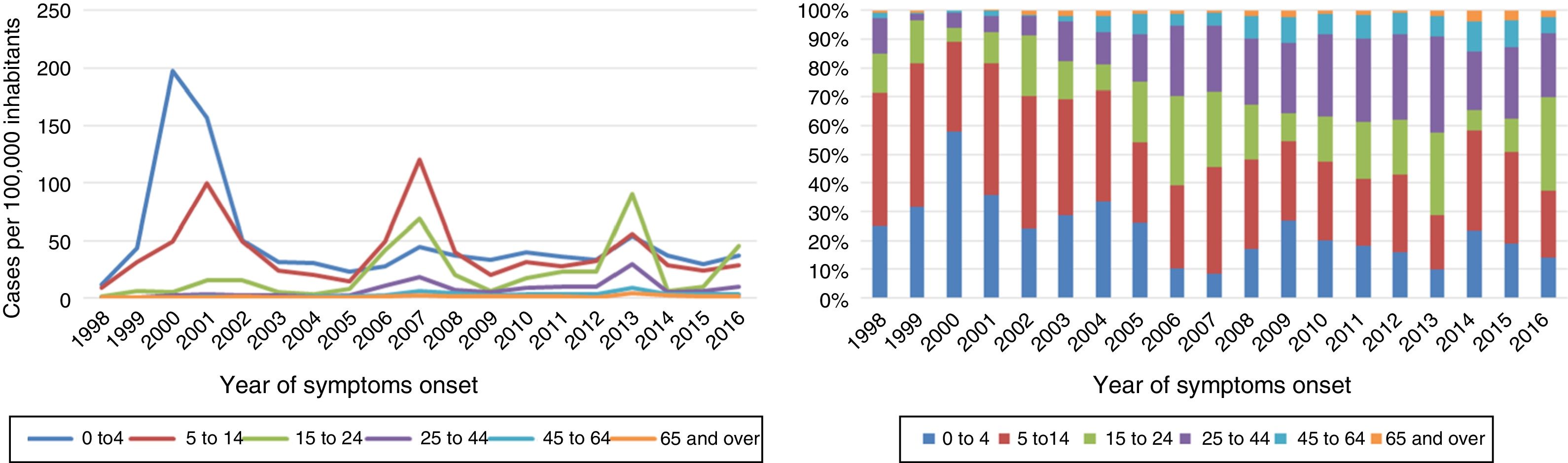
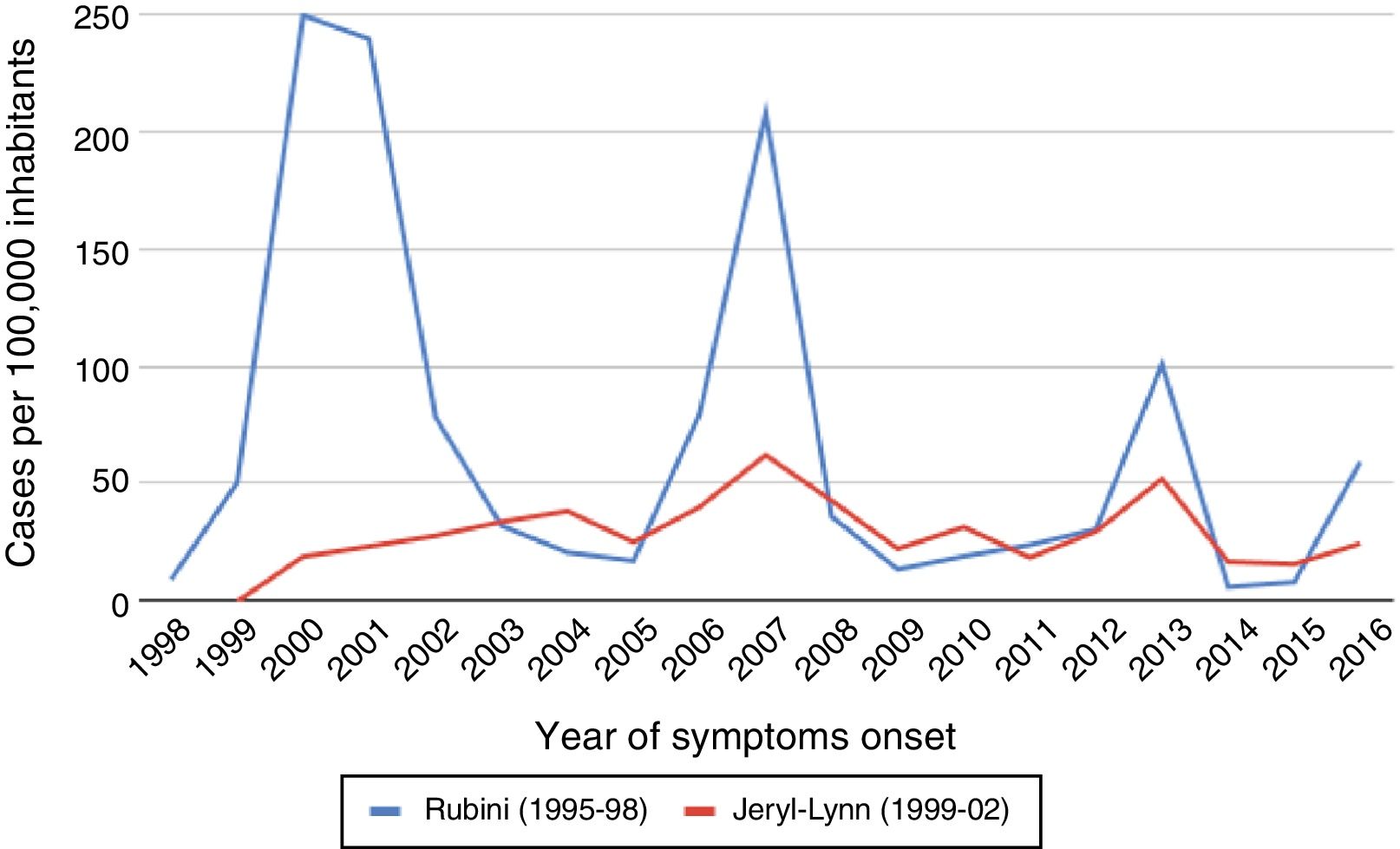
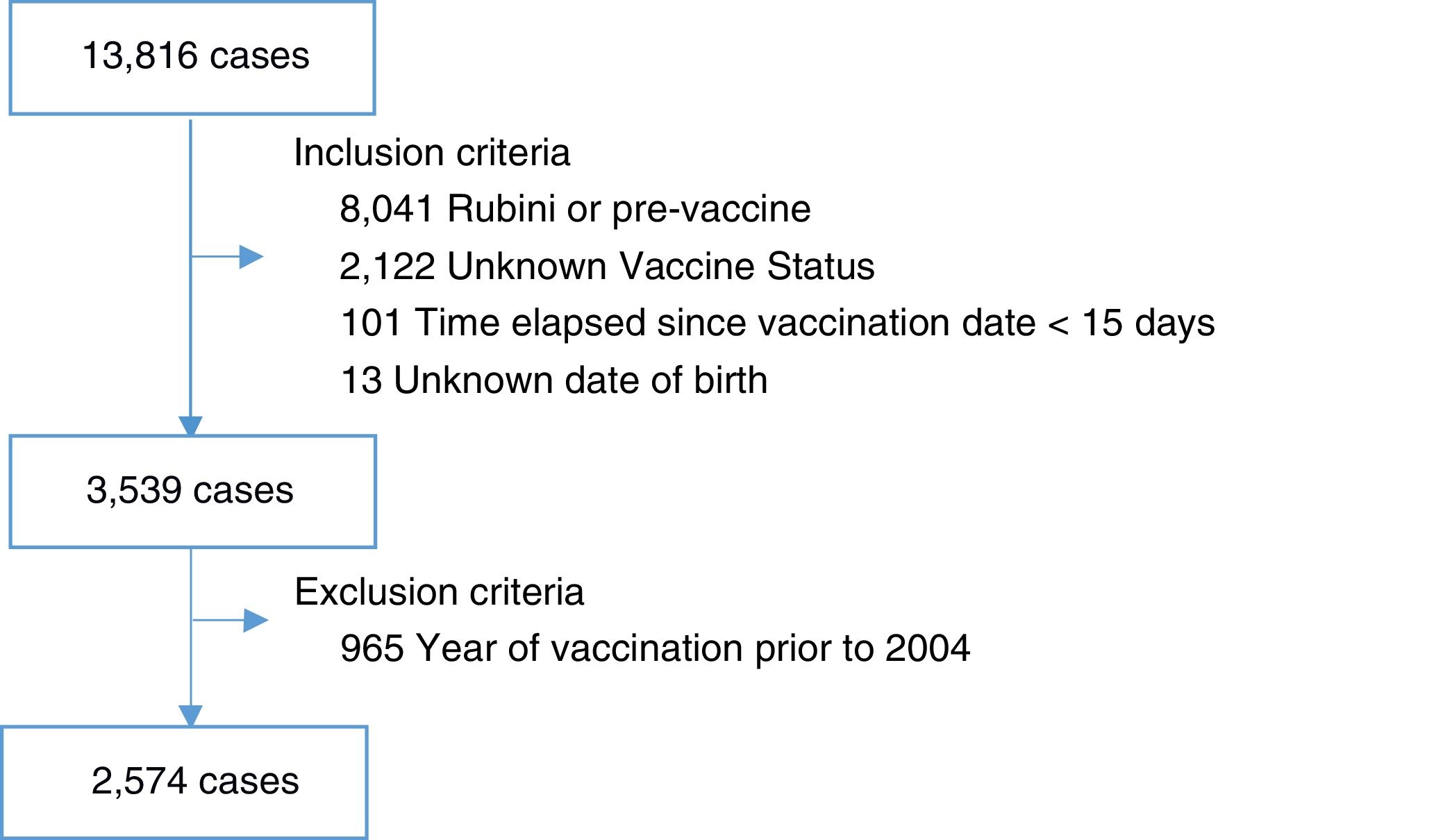
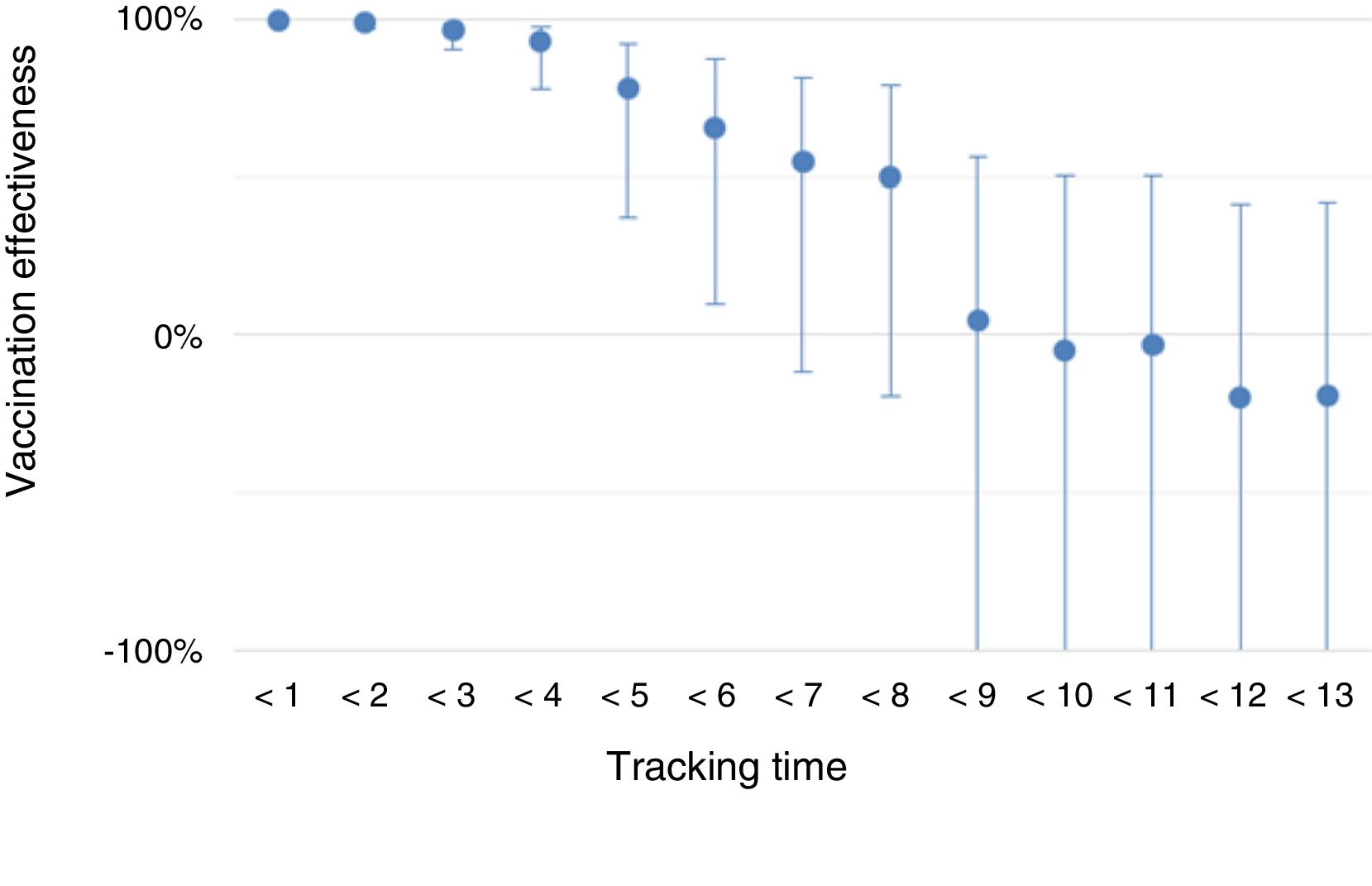
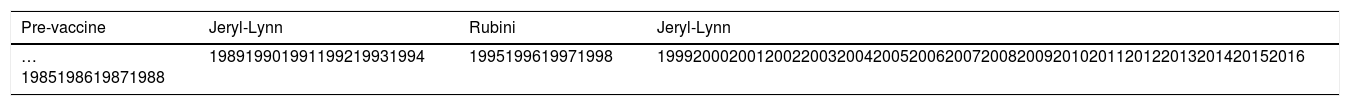
Material and methodsCases notified to the Notifiable Disease System between 1998 and 2016 were used for the study. The vaccine effectiveness (VE) was calculated in cohorts vaccinated with two doses of Jeryl-Lynn, and the impact was calculated by comparing incidences by age and by Rubini (1995–1998) and Jeryl-Lynn (1999–2002) cohorts during the periods 1998–2004, 2005–2009 and 2010–2015. The incidences for age group and period were compared with the previous period and the incidences for cohorts were compared within a period with incidence ratios (IR) using Poisson models. The VE was estimated using the screening method using logistic regression models.
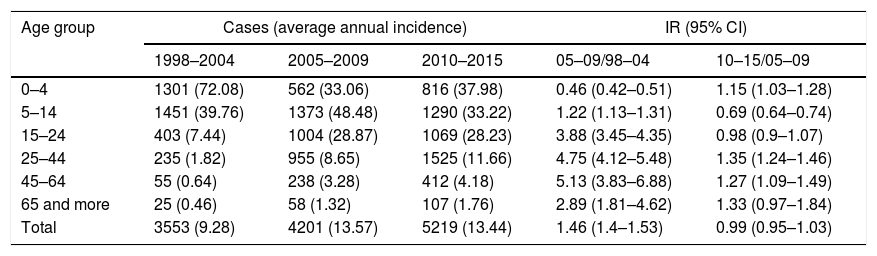
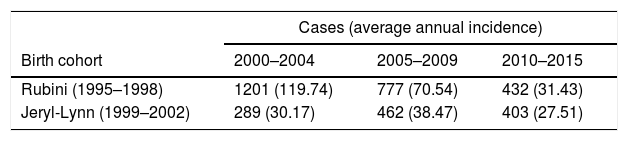
Results13,816 cases were reported. The incidence in 2005–2009 was higher than in 1998–2004 (IR: 1.46, 95% CI: 1.40–1.53), and it remained stable in 2010–2015 (IR: 0.99, 95% CI: 0.95–1.03). The average incidence rate of the Rubini cohort was 69.43 and the Jeryl-Lynn cohort was 32.24. The IR was 0.25 (95% CI: 0.22–0.29), 0.55 (95% CI: 0.49–0.61) and 0.88 (95% CI: 0.76–1.00) for each period respectively. 2574 cases were included in the VE study. EV decreased over time reaching not significant values after seven years of follow-up (VE: 55%, 95% CI: 82 to −12%).
ConclusionsParotiditis behavior is characterized by fluctuations, changes in presentation and a decrease in VE.
La parotiditis se caracteriza por la inflamación de la glándula parótida y fiebre, y es prevenible mediante vacunación con triple vírica (TV). El objetivo es evaluar el impacto y la efectividad vacunal (EV).
Material y métodosSe seleccionaron los casos notificados al Sistema de Enfermedades de Declaración Obligatoria entre 1998 y 2016. La EV se calculó en cohortes vacunadas con 2 dosis de Jeryl-Lynn, y el impacto comparando las incidencias por edad y por cohortes Rubini (1995-1998) y Jeryl-Lynn (1999-2002) en los periodos 1998-2004, 2005-2009 y 2010-2015. Las estimaciones por grupo de edad y período se compararon con las del período anterior y las estimaciones por cohortes se compararon entre sí dentro de cada período mediante razones de incidencia (RI) empleando modelos de Poisson. La EV se estimó empleando el método de cribado mediante modelos de regresión logística.
ResultadosSe notificaron 13.816 casos. La incidencia en 2005-2009 fue superior a la de 1998-2004 (RI: 1,46; IC 95%: 1,40-1,53), y en 2010-2015 se mantuvo estable (RI: 0,99; IC 95%: 0,95-1,03). La incidencia anual media de las cohortes Rubini fue de 69,43 casos por 100.000 habitantes y la de las cohortes Jeryl-Lynn de 32,24. La RI fue de 0,25 (IC 95%: 0,22-0,29), 0,55 (IC 95%: 0,49-0,61) y 0,88 (IC 95%: 0,76-1,00) para cada periodo, respectivamente. Se incluyeron 2.574 casos en el estudio de EV. La EV disminuyó con el tiempo al alcanzar valores no significativos tras 7 años de seguimiento (EV: 55%; IC 95%: 82 a -12%).
ConclusionesEl comportamiento de la parotiditis se caracteriza por presentar fluctuaciones, cambios en la presentación etaria y una disminución de la EV.