Edited by: Dr. Ana Rita Silva
(University of Coimbra, Coimbra, Portugal)
Dr. Elodie Bertrand
(Paris Cité University, Paris, France)
Dr. Maria Schubert
(Zurich University of Applied Sciences, Zurich, Switzerland)
Last update: October 2025
More infoWith increasing global life expectancy, cognitive interventions hold promise in mitigating cognitive decline and fostering healthy aging. Despite the demand for evidence-based interventions, there have been few attempts to summarize existing evidence. This study aims to assess the effectiveness and feasibility of unimodal and multimodal cognitive interventions for cognitively healthy older adults.
MethodSystematic meta-review, selecting articles from four databases: PubMed, Web of Science, Embase, and Cochrane Library. Quality assessment carried out with AMSTAR2. Findings were summarized and discussed narratively.
ResultsThirty-nine articles were included, with 21 meta-analyses and 18 qualitative systematic reviews. The total number of reviews was 38 for cognitive training, 4 for cognitive stimulation, and 1 for multicomponent interventions. Most reviews had low or critically low quality.
ConclusionsThe prevailing evidence supports cognitive training. Continued research into cognitive stimulation and multicomponent protocols is encouraged. Longer follow-ups are important for identifying combined and clinically significant results. Rigorous risk of bias and quality assessment is necessary to enhance the evidence base.
Life expectancy is increasing worldwide (Gauthier et al., 2022) with the world population aged 65 years or over being projected to reach 994 million by 2030 and 1.6 billion by 2050 (United Nations Department of Economic & Social Affairs, Population Division, 2022). By this year, the World Population Prospects 2022 suggests that there will be more than twice as many persons over this age as children under 5 years old worldwide, and a 65-year-old individual is expected to live for approximately 20 more years (United Nations Department of Economic & Social Affairs, Population Division, 2022). This new demographic configuration requires societies to adapt, promoting new health and social care policies to provide for the older population, preparing for the changes that lie ahead.
With the increase in life expectancy, the prevalence of major neurocognitive disorders should follow a corresponding progression (Ferri et al., 2005; Prince et al., 2013). The global prevalence of dementia in adults over 50 years old is estimated at 6.97 % (Cao et al., 2020) with 153 million people expected to be living with dementia worldwide by 2050 (GBD 2019 Dementia Forecasting Collaborators, 2022). The annual global cost of dementia in 2019 was 1.3 trillion USD, with approximately half of these costs being attributable to care provided by family members and close friends (World Health Organization, 2023). Large costs of healthcare needs often impact the families of people living with dementia (PlwD) and their ability to work, particularly affecting the economy and social care in low-income countries (Carvalho & Neri, 2019).
Albeit complex, reducing age-specific risk for dementia is feasible, given changes in development and lifestyle (Langa, 2015). For example, increases in education in early life and decreases in hypertension, smoking, and diabetes across the life span have protective value (Prince et al., 2013). Recent findings suggest that cognitive activities may help reduce the risk of dementia and enhance latelife cognition, potentially contributing to cognitive maintenance (Livingston et al., 2020), but the quality of existing evidence has been questioned (Livingston et al., 2024), limiting more consistent recommendations.
Also, there is considerable variability between individuals regarding the susceptibility to both age-related and pathological brain changes for which cognitive reserve may be one of the factors responsible (Stern, 2012). Epidemiological evidence suggests that life experiences, even in later life, can contribute to cognitive reserve (Stern, 2012). Interventions for healthy older adults (HOA) that seek to improve functional and cognitive abilities might be useful to slow age-related cognitive decline and prolong healthy aging (Stern, 2012).
Cognitive interventions are usually classified as cognitive stimulation (CS), cognitive training (CT) or cognitive rehabilitation (CR) (Clare & Woods, 2004; Mlinac et al., 2022). CS involves engagement in a range of activities and discussions, typically in a group, aimed at the general enhancement of cognitive and social functioning (Clare & Woods, 2004; Mlinac et al., 2022). CT refers to guided practices on a set of standard tasks designed to reflect particular cognitive functions (Clare & Woods, 2004; Mlinac et al., 2022). CR employs a biopsychosocial approach to identify and work towards achieving treatment goals that are relevant to everyday functioning (Clare & Woods, 2004; Mlinac et al., 2022).
The World Alzheimer Report 2023 recommends that people keep learning (Long et al., 2023), but it does not cite any structured protocol that can be strongly recommended for the prevention of cognitive decline in healthy older adults (for PwD, Cognitive Stimulation Therapy is recommended; Spector et al., 2003; Gauthier et al., 2022). Despite the demand for a reliable intervention and the diversity of empirical studies and systematic reviews for specific types of intervention, there have been few attempts to do a broad analysis of actual evidence. Gavelin et al. (2020) conducted a recent overview, but included only unimodal CS or CT interventions, excluding multimodal or other arrangements. Considering this, the current systematic meta-review investigates the effectiveness and feasibility of unimodal and multimodal cognitive interventions designed for cognitively healthy older adults, based on the available scientific literature.
MethodsLiterature searchReviewed articles were selected according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Page et al., 2021) guidelines and the systematic review protocol was registered in PROSPERO (CRD42023387917). Each search term was systematically searched on the PubMed, Web of Science, Embase and Cochrane Library databases, considering articles published until the 2nd of April 2024.
The following keywords were used: (("cognitive stimulation") OR ("cognitive training")) AND (("older adults") OR (elderly)) AND (((((((dementia) OR ("cognitive decline")) OR (AD)) OR (Alzheimer*)) OR (MCI)) OR ("cognitive impairment")) OR ("neurocognitive disorder*")) AND ((systematic reviews) OR (meta-analysis)).
Study selectionThis systematic meta-review includes peer-reviewed systematic reviews and meta-analyses with cognitive, affective and/or functional outcomes. Eligible studies met the following criteria: psychosocial interventions for cognitively healthy older adults, with an average age greater than or equal to 50 years old. We accepted any definition of “healthy older adults” established by the review authors.
We initially planned to include only studies with an average age greater than 60 years. However, as we observed that some studies considered participants over 50 years old as healthy older adults, to conduct a comprehensive overview, these articles were not excluded. Systematic reviews and meta-analyses including studies with healthy older adults and clinical groups, or with healthy older adults and other age groups, were included only if the data of our population of interest (cognitively healthy older adults) could be sorted from other populations and had at least 3 studies with healthy older adults included in the review.
Publications were excluded if: (1) focused on any special clinical group (dementia, diabetes, HIV, frailty, orthopedic surgeries, etc.) or (2) other ages; (3) did not include psychosocial interventions, (4) were not systematic reviews/meta-analyses, (5) no cognitive, affective or functional data from healthy participants were available, (6) were not peer reviewed articles (e.g. conference papers, protocols, etc.) or (7) not written in English. Fig. 1 displays the process of study identification. A list of studies excluded by full text screening is available on Supplementary Material A.
Data extractionThe study was carried out using the Rayyan software (Ouzzani et al., 2016). Two authors (V.V. and S.L.T. or I.B.) independently screened abstracts for inclusion, blinded by the software. Disagreements were resolved after discussion between the authors. Full-text screening was carried out with the same procedure, using independent spreadsheets.
From selected studies, the following information was extracted: authors, year of publication, type of intervention, number of studies included, study design, sample size and mean age, intervention and session duration and frequency, outcome domains, relevant findings and quality/risk of bias assessment. Data were extracted independently by two authors (V.V. and S.L.T or I.B.) and disagreements were resolved by comparing observations and reaching a consensus. Results were summarized and discussed narratively.
We classified the studies by intervention type (e.g., CT, CS, multicomponent interventions) according to definitions established in primary systematic reviews. In addition, practices were highlighted when associated with physical exercises done simultaneously (dual tasks) or sequentially (one followed by the other), or carried out separately in multicomponent interventions. Multicomponent interventions that also had nutritional, medical, and occupational monitoring were also accepted.
Primary reviews that included only cognitive training interventions carried out on a computer or digital device were classified as “computerized cognitive training”. If any type of cognitive training was allowed, including paper and pencil or digital activities, we classified it as “cognitive training” without additional elucidation.
Risk of bias (quality) assessmentThe quality assessment was carried out with the AMSTAR2 tool (Shea et al., 2017), designed specifically for assessing the quality of systematic reviews and meta-analyses. Initially, it was planned to also use the criteria proposed by Kmet et al. (2004), but we observed that the majority of items would only be suitable for evaluating empirical studies.
The following were classified as critical appraisal questions, determining the overall confidence level of each study: (1) “Did the review authors use a comprehensive literature search strategy?”, (2) “Did the review authors describe the included studies in adequate detail?”, (3) “Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review?”, (4) “If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results?”, (5) “If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis?”, (6) “Did the review authors account for RoB in individual studies when interpreting/discussing the results of the review?”, (7) “Did the review authors provide a satisfactory explanation for and discussion of any heterogeneity observed in the results of the review?”.
A partial yes was considered as “yes” for the purpose of overall confidence classification. Results for each quality criteria and overall confidence ratings across included reviews are available on Figs. 2 and 3. Complete AMSTAR 2 checklist (Shea et al., 2017), a description of quality criteria and the scheme for interpreting weaknesses detected in critical and non-critical items are available in Supplementary Material B.
Thirty-nine articles were included, with 21 meta-analyses and 18 qualitative systematic reviews. More than half (23) of the studies also accepted clinical populations. In these cases, data were extracted if (1) clinical trials only included healthy participants or (2) separated meta-data for healthy populations were available. Twenty-nine articles reported the mean population age, of which 23 were between 70 and 80 years. None of them had an average of <60 or >80 years. The largest sample size was 8732 (Mendonça et al., 2022) and the smallest was 163 (ten Brinke et al., 2017). Twenty-three studies included only randomized clinical trials (RCT) study designs.
Most of the studies did not fully describe settings. The majority of reviews included studies with passive (P.C.) and/or active (A.C.) control groups. A few exceptions included no control (e.g. Webb et al., 2021), other interventions (e.g. Ishibashi et al., 2023), or unclear controls (e.g. Fan & Wong, 2019).
Most reviews (29) had low or critically low quality. Only ten reviews (25.64 %) had at least moderate quality, and none were classified as high quality. The main critical flaws were unsatisfactory techniques and insufficient discussion for risk of bias (RoB) assessment and outcomes. A full description of instruments and results for risk of bias/ quality assessment carried out in each systematic review is available in Supplementary Material C.
Almost all studies included PICO (Population, Intervention, Context and Outcome measures; Schardt et al., 2007) descriptions, did a comprehensive search strategy, discussed possible sources of heterogeneity and reported potential conflicts of interest. Results for individual quality domains and overall confidence across reviews are reported in Figs. 2 and 3. Detailed assessment for individual reviews is available in Supplementary Material B. Findings were divided by type of intervention and reported below (for characteristics of the included studies, see Tables 1–3).
Systematic reviews and meta-analysis about cognitive training interventions.
| Main Author (Year) | Studies Included (n) | Study Design | Sample Size (mean age) | Duration and Frequency | Outcome Domains | Review Outcome |
|---|---|---|---|---|---|---|
| Meta - analyses | ||||||
| Papp et al. (2009) | 10 | RCT | 4009 (74.1) | 6 - 90 weeks; 30 - 180 min/sess; 1 - 5 sess/week | GC, WM/Divided Att., Inhibition, Planning/CF, PS, RT/Motor Speed, Mem., VSF, ADLs | Small effect of PS interventions on overall cognition; very small for all cognitive interventions across all outcomes, and for Mem., Reas. and multimodal interventions; similar effects with A.C. and P.C. I2: n/c |
| Valenzuela and Sachdev (2009) | 7 | RCT | 6339 (n.f.d) | 5 - 30 weeks; 60 - 90 min/sess; 1 - 4 sess/week | Att., EF, Mem., Verbal Learning, VSF | Large overall effect size compared with P.C.; RCTs with follow-up > 2 years had similar E.S. as shorter follow-ups (sensitivity analysis) I2: n/c |
| Martin et al. (2011) | n.f.d. | RCT | n.f.d(n.f.d.) | n.f.d. | Mem. | Better Mem. score than P.C. but not than A.C. I2. n.f.d. |
| Hindin and Zelinski (2012) | 25 | pre- post- test with C.G. | 2765 (69.9) | 2 - 12 weeks | EF, Choice RT, Mem. | Small effect on untrained cognitive tasks. Better study quality linked with ESs. I2: n/c |
| Karr et al. (2014) | 23 | clinical trial | 1061 (72.3) | 4 - 96 weeks; 15 - 240 min/sess; < 1 - 5 sess/week | EF (Att., VF, WM, Inhibition, Problem-Solving) | Significant effect for EF. I2: n.f.d. |
| Kelly et al. (2014)1 | 23 | RCT | 5037 (54 - 99) | 2 - 96 weeks; 15 - 120 min/sess; 1 - 5 sess/week | GC, EF (Att., WM, VF, Reas., PS), Mem., SCP, Daily Function | Compared to A.C., moderate (WM; I2: 84 %) to large (PS; I2: 75 %) effects for EF, small ES for cognitive function (I2: 0 %). Compared to A. C. and P.C., mixed findings for different types of Mem., with small to moderate effects. Transfer and maintenance linked with adaptive training (≥ 10 sess and a long-term follow-up). |
| Lampit et al. (2014) | 51 | RCT | 4885 (70.8) | 2 - 16 weeks; 15 - 120 min/sess; 1 - 7 sess/week | GC, Att., EF, WM, PS, Mem., VSF | Small ES on overall cognition (I2: 29.9 %), nonverbal Mem. (I2: 24.5 %), WM (I2: 45.6 %) and VSF (I2: 42.7 %). Moderate ES on PS (I2: 84.5 %). Very small ES for verbal Mem. (I2: 50.1 %). No effect for EF (I2: 31.8 %) and Att. (I2: 62.9 %). Home-based less effective than group training, and > 3 sess/week was ineffective versus ≤ 3. |
| Mewborn et al. (2017) | 48 | RCT | 3718 (77.0) | 1 - 90 weeks; 6 - 180 min/sess; 1 - 7 sess/week | GC, Att., EF, WM, PS, Reas., Mem., Lang.,VSF | Small effect on overall cognition relative to A.C. and P.C. (I2: 57 %). |
| Bruderer-Hofstetter et al. (2018) | 11 | RCT | 670 (71.5) | 4 - 24 weeks; 20 - 90 min/sess; 1 - 3 sess/week | GC, Att., EF, Mem., IADLs, Percep. Motor Function | Effective for overall cognition (I2: 4 %); best ranked: aerobic exercise (interval)+ CT (Israel method). |
| Webb et al. (2018) | 51 | RCT | 4885 (70.8) | 2 - 16 weeks; 15 - 120 min/sess; 1 - 7 sess/week | EF, STM, PS, Fluid Reas., Long-Term Storage/Retrieval, VSF | Differences from Lampit et al. (2014). Moderate effect for PS (I2: 87.3 %). Small ES for VSF (I2: 15.4 %), ES (I2: 24.0 %), long-term storage and retrieval (I2: 67.0 %) and STM (I2: 44.6 %). No effects for fluid Reas. (I2: 61.1 %). |
| Basak et al. (2020) | 161 | RCT | 13,797(70.3) | uni: 1 - 12 multi: 1 - 90 weeks | GC, EF, PS, Reas., Mem., Lang., Daily Function | Small net gain on overall cognition (I2: 82.3 %), for unimodal(I2: 84.0 %) or multimodal training (I2: 82.3 %), and for near (I2: 85.4 %) and far (I2: 82.3 %) transfer. Larger ES for near transfer, lower educational level and fewer outcomes. |
| Gates et al. (2020) | 8 | RCT | 1183 (74.5) | 12 - 26 weeks; 10 - 90 min/sess; 1 - 3 sess/week | GC, Att., EF, WM, PS, VF, Episodic Mem., QoL/ Well-Being | Small effect on global cognition compared to A.C. (after 3 months) (I2: 0 %), and on episodic Mem. compared to P.C. (after 6 months) (I2: n/a). |
| Guo et al. (2020) | 14 | RCT | 1012 (71.8) | 7 - 24 weeks; 15 - 150 min/sess; 1 - 10 sess/week | EF: Complex EF, Inhibition, Shifting | Small effect for EF (I2: 23.3 %). |
| Gavelin et al. (2021) | 27 | RCT | 2620 (73.4) | 4 - 24 weeks; 15 - 105 min/sess; 1 - 6 sess/week | GC, EF, WM, STM, PS, Fluid Reas., Long-Term Mem., Visual Process. | Small effect for overall cognition (I2: n/c). |
| Nguyen et al. (2021) | 37 | pre- post- test with C.G. | 2511 (71.2) | 2 - 16 weeks; 10 - 90 min/sess; 1.3 - 7.5 sess/total | Att., EF, PS, Fluid Reas., Lang., Mem., VSF, Daily Function | After adjusting for publication bias, only small E.S. for PS remained significant (I2: 69.2 %). |
| Yun and Ryu (2022) | 29 | RCT | n.f.d. (70.6) | n.f.d. | GC, ADLs, IADLs, QoL, Depr. | Small effect for overall cognition. (I2: 29.3) |
| Tse et al. (2023)4 | 26 | RCT | 1504 (71.0) | n.f.d. | Prospective Memory | Medium E.S. (I2: 73.0 %), mainly based on single-session training. |
| Wu et al. (2023) | 16 | RCT | 910 (71.4) | 4 - 16 weeks; 30 - 150 min/sess; 1 - 6 sess/week | Working Memory | Small E.S. (I2: 0 %) for combined interventions (PE + CT). |
| Li et al. (2024) | 20 | RCT | 1624 (69.9) | 1 - 16 weeks; | GC, Att., EF, Reas., Mem., Lang., VSF | Small overall ES (I2: n/c). No effect when engagement < 60 % or persistence < 80 %. |
| Systematic Reviews | ||||||
| Kueider et al. (2012) | 38 | pre- post- test design | 3205 (50 - 96) | 2 - 68 weeks; 15 - 240 min/sess;1 - 7 sess/week. | GC, Att., EF, WM, PS, RT, Mem., VSF | Overall, improvement on trained domain. PS and RT outcomes: larger median ESs. Classic CT and neuropsychological softwares: large median ES for PS. Videogames (VG): moderate median ES. CT and VG: moderate median ES for RT. |
| Reijnders et al. (2013)1,2 | 13 | RCT | 1432 (69.7) | 2 - 12 weeks; 20 - 120 min/sess; 2 - 5 sess/week | GC, Att., EF, WM, PS, Reas., Mem., SCP, Percep., Daily Function, Mood | Some efficacy in improving Mem., EF, PS, Att., fluid intelligence, subjective and overall cognition. No generalization for daily functioning. |
| Law et al. (2014) | 3 | RCT, NRCT | 480 (71.8) | 8 - 48 weeks; 40 - 150 min/sess (CT: 40 - 90; PE: 45 - 150); 1 - 3 (CT: 1 - 2; PE: 1 - 3) sess/week | GC, EF, Mem., Episodic Mem., SCP, Somatic Function, Daily Function, Mood, Apathy, Relationships | Mixed findings for GC and Mem. |
| Lauenroth et al. (2016) | 13 | clinical trial | 883 (74.1) | 4–30 weeks; 30–60 min/sess (simul.) or [PE: 30–60 + CT: 10–90] (seq.); 1–5 sess/week (simul.) or [PE: 1–4 + CT: 1–5] (seq.) | GC, Att., EF, WM, RT, Inhibition, Mem., Lang., Calculation, VSF, Praxis, ADLs | Most studies reported post-intervention improvements in trained cognitive functions. |
| Mowszowski et al. (2016) | 13 | RCT, quasi-RCT | 4120 (70) | 2 - 16 weeks; 53 - 90min/sess; 1 - 2 sess/week | WM, CF, Inhibition, Reas., Planning, Phonemic VF, Problem-Solving, IADLs, Daily Function | Most studies with moderate to large ES, focusing on inductive Reas. Evidence of sustained benefits and far transfer. |
| Butler et al. (2017) | 6 | RCT | 4357 (n.f.d.) | 2 - 24 weeks; 20 - 120 min/sess; 1 - 5 sess/week | Att., EF, PS, VF, Reas., Problem-Solving, Mem., Lang., VSF, ADLs, IADLs, Daily Function | Moderate-strength evidence of improvement on the domain trained. Results driven by 1 large trial. |
| Shah et al. (2017) | 26 | RCT, quasi-RCT, follow-up | 5381 (50 - 95) | 3 - 24 weeks; 15 - 75 min/sess; 2 – 5 sess/week | GC, Att., EF, WM, CF, PS, RT, Reas., Problem-Solving, Mem., Lang., VSF, SCP, Praxis,Speech-in-Noise Percep., IADLs., Daily Function, HRQoL, Well-Being | Near transfer for the domain trained (programs with level I and II evidence). Improvement in PS (level II). Far transfer for IADLS and HRQoL only in > 5 years follow-up (level I) and well-being (level III). Twelve out of 19 studies were conducted/funded by the program's company. |
| ten Brinke et al. (2017) | 6 | RCT, quasi-exp. | 163 (69.7) | 1 - 17 weeks; 30 - 60 min/sess; 3 - 6 sess/week | GC, EF, WM, PS, RT, Reas., Mem. | Inconclusive results because most studies have no control group. |
| Alnajjar et al. (2019) | 15 | pre- post- test design | 3199 (57 - 84) | 4 - 32 weeks; 20 - 60 min/sess; 1 - 5 sess/week. | GC, Att., EF, WM, PS, RT, Reas., Controlled Process., Problem- Solving, Mem., Lang., Spatial Navigation, ADLs, Well-Being, Depr. | Inconclusive results due to mixed findings and study designs. |
| Fan and Wong (2019) | 9 | RCT | 6554 (71.0) | 10 - 36 sessions | GC, WM, PS, Reas., Mem., VSF, IADLs | IADLs improved. Evidence of improvement for GC, and for Mem. and Reas. in domain specific interventions (near transfer). |
| Nguyen et al. (2019) | 20 | pre- post- test with C.G. | 635(69.4) | 4 - 24 weeks; 15 - 90 min/sess; 1 - 5 sess/week | GC, Att., EF, WM, CF, Inhibition, PS, RT, Reas., Dual-Task, Multi-task, Mem., VSF | Trained cognitive tasks improved, with mixed findings for untrained tasks. |
| Marr et al. (2020) | 7 | pre- post- test design | 1319 (70.0) | 2 - 16 weeks; 30 - 90 min/sess; 1 - 3 sess/week | EF, WM, Reas., Divergent Thinking, Mem. | Some evidence of efficacy for EF, Reas. and Mem. |
| Masurovsky (2020) | 19 | RCT | n.f.d. (n.f.d.) | n.f.d. | Att., PS, Cognitive Control, Mem., Lang., Visuospatial construction | 12 of 19 studies had near transfer. None which had significant effect for far transfer (6) measured expectations, and only 1 included A.C. |
| Dhir et al. (2021) | 5 | pre- post- test with C.G. | 193 (n.f.d.) | n.f.d. | Inhibition | Only one study reached significance, with large ES for simultaneous combined training on inhibition. |
| Intzandt et al. (2021)3 | 12 | RCT; quasi-exp. | 607 (68.1) | 2 - 24 week;45 - 120 min/sess;1 - 5 sess/week | Att., EF, WM, VF, PS, Reas., Mem. | Most studies reported significant effects on at least one measure of cognitive functioning, especially memory. |
| Webb et al. (2021) | 5 | pre- post- test design | 1687 (72.2) | 2 - 6 weeks; 30 - 120 min/sess; 1 - 3 sess/week | WM, PS, Mem. (objective and subjective) | Inconclusive results due to mixed findings and study designs. |
| Mendonça et al. (2022) | 13 | cohort | 8732 (n.f.d.) | 3 - 140 weeks; 45 - 120 min/sess; 1 - 2 sess/week | Mem. (episodic) | All studies found significant results for episodic memory. |
| Ishibashi et al. (2023) | 9 | pre- post- test with C.G. | 787 (60 - 85) | 5 - 12 weeks; 20 - 60 min/sess; 1 - 5 sess/week | GC, Att., EF, WM, Inhibition, PS, VF, Reas., Learning and Mem., Lang., VSF, Life Satisfaction, Self-Efficacy, Stress, Odor Identification | 6 out of 9 studies reported some effect on at least one measure of cognitive functioning. |
| Tse et al. (2023)4 | 37 | cross-sectional, longitudinal or both | 2061 (71.3) | n.f.d. | Prospective Memory | 23 out of 43 comparisons reported a significant effect. |
| Sáez-Gutiérrez et al. (2024)1 | 13 | RCT | 6822 (71.5) | 3 - 36 weeks; 10 - 120 min/sess; <1 - 10 sess/week | Daily Function | 9 out of 13 studies reported some effect on at least one measure of functionality. |
Note. n/a: not applicable; n/c: not calculated; n.f.d.: not fully described. A.C.: Active control; ADLs: activities of daily living; Att.: attention; CF: cognitive flexibility; Depr.: depression; EF: executive functions; ES: effect size; GC: global cognition; HRQoL: health-related quality of life; IADLs: instrumental activities of daily living; Lang.: language; Mem.: memory; P.C.: Passive Control; Percep.: perception; Process.: processing; PS: processing speed; QoL: quality of life; Reas.: reasoning; RT: reaction time; SCP: subjective cognitive performance; STM: short-term memory; VF: verbal fluency; VSF: visuospatial function; WM: working memory.
Studies presented results for both CS and CT; for ease of interpretation, those results are presented separately on Tables 1 and 2.
1 Clinical study non-RCT was included, but poorly described with no quality evaluation. Therefore, we did not include these results.
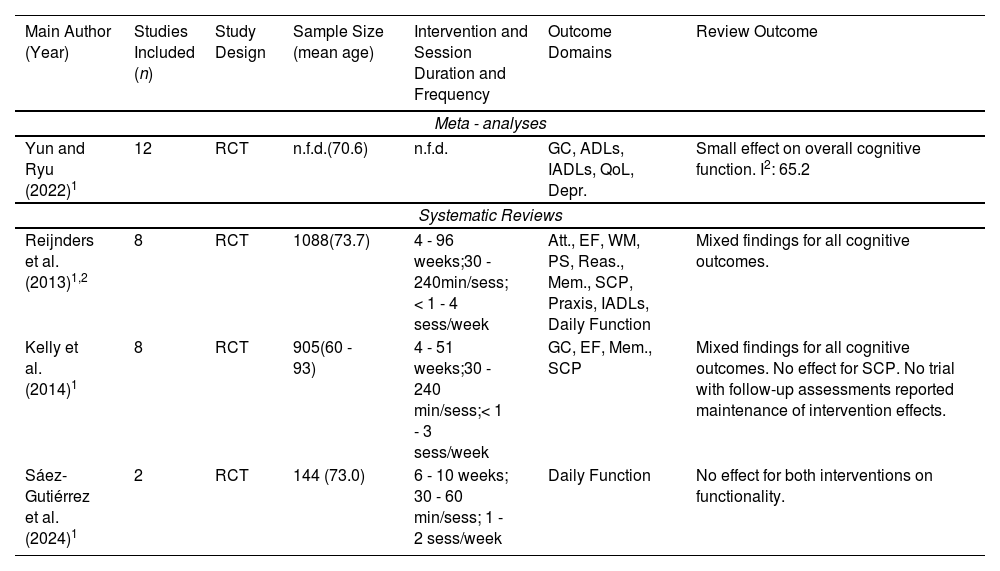
Systematic reviews and meta-analysis about cognitive stimulation interventions.
| Main Author (Year) | Studies Included (n) | Study Design | Sample Size (mean age) | Intervention and Session Duration and Frequency | Outcome Domains | Review Outcome |
|---|---|---|---|---|---|---|
| Meta - analyses | ||||||
| Yun and Ryu (2022)1 | 12 | RCT | n.f.d.(70.6) | n.f.d. | GC, ADLs, IADLs, QoL, Depr. | Small effect on overall cognitive function. I2: 65.2 |
| Systematic Reviews | ||||||
| Reijnders et al. (2013)1,2 | 8 | RCT | 1088(73.7) | 4 - 96 weeks;30 - 240min/sess;< 1 - 4 sess/week | Att., EF, WM, PS, Reas., Mem., SCP, Praxis, IADLs, Daily Function | Mixed findings for all cognitive outcomes. |
| Kelly et al. (2014)1 | 8 | RCT | 905(60 - 93) | 4 - 51 weeks;30 - 240 min/sess;< 1 - 3 sess/week | GC, EF, Mem., SCP | Mixed findings for all cognitive outcomes. No effect for SCP. No trial with follow-up assessments reported maintenance of intervention effects. |
| Sáez-Gutiérrez et al. (2024)1 | 2 | RCT | 144 (73.0) | 6 - 10 weeks; 30 - 60 min/sess; 1 - 2 sess/week | Daily Function | No effect for both interventions on functionality. |
Note. ADLs: activities of daily living; Att.: attention; Depr.: depression; EF: executive functions; GC: global cognition; IADLs: instrumental activities of daily living; Mem.: memory; PS: processing speed; QoL: quality of life; Reas.: reasoning; SCP: subjective cognitive performance; WM: working memory.
Studies presented results for both CS and CT; for ease of interpretation, those results are presented separately on Tables 1 and 2.
Systematic reviews and meta-analysis about multicomponent interventions.
| Main Author (Year) | Studies Included (n) | Study Design | Sample Size (mean age) | Intervention and Session Duration and Frequency | Outcome Domains | Review Outcome |
|---|---|---|---|---|---|---|
| Kim et al. (2022) | 6 | RCT | 1102(74.8) | 6 - 24 weeks;20 - 150 min/sess;< 1 - 2 sess/week. | GC, ADLs, IADLs, HRQoL, Adaptative Strategies, Falls Efficacy, Depr., Anxiety, Confidence on Daily Tasks, Fear of Falling, Loneliness. | Some evidence of efficacy of occupational + physical therapy and cognitive-behavioral therapy + baduanjin qigong on ADLs and IADLs; mixed findings for multicomponent CT. |
Note. ADLs: activities of daily living; Depr.: depression; GC: global cognition; HRQoL: health-related quality of life; IADLs: instrumental activities of daily living.
In total, there were 19 meta-analyses structured on CT. Out of these, 7 included any form of CT (Papp et al., 2009; Valenzuela & Sachdev, 2009; Martin et al., 2011; Kelly et al., 2014, Mewborn et al., 2017; Nguyen et al., 2021; Li et al., 2024), 4 focused only on computerized CT (Lampit et al., 2014; Webb et al., 2018; Basak et al., 2020; Gates et al., 2020), 4 investigated multimodal CT and physical exercise (PE) (Bruderer-Hofstetter et al., 2018; Guo et al., 2020; Gavelin et al., 2021; Wu et al., 2023), 2 compared CT with PE interventions (Hindin & Zelinski., 2012 ; Karr et al., 2014), and 1 included only prospective memory training (Tse et al., 2023). Yun and Ryu (2022) included any form of CT, but also included one study with mixed CS plus CT.
Most (16) studies selected only RCTs. Also, 2 included any pre- and post-test design with a control group (Hindin & Zelinski., 2012; Nguyen et al., 2021) and 1 included any type of clinical trial (Karr et al., 2014). Between 7 to 161 studies were included in each meta-analysis, with a sample size between 670 and 13,797 participants and a mean age of 71.9 years. In these studies, CT (applied with or without other interventions) programs had a duration between 1 and 96 weeks, with a range of 6 to 240 min for each session, and spanned from 10 weekly sessions to frequencies lower than weekly. Sample size and intervention characteristics were not described separately from CS and/or clinical populations in Martin et al. (2011) and Yun and Ryu (2022). Hindin and Zelinski (2012), Basak et al. (2020), Tse et al. (2023) and Li et al. (2024) did not fully describe the intervention characteristics.
Overall, studies found small to large effects for processing speed (Kelly et al., 2014; Lampit et al., 2014; Webb et al., 2018; Nguyen et al., 2021), small to moderate effects for working memory (Kelly et al., 2014; Lampit et al., 2014; Wu et al., 2023), very small to moderate effects for memory (Webb et al., 2018; Gates et al., 2020; Tse et al., 2023), and very small to small effect for global cognitive function (Papp et al., 2009; Kelly et al., 2014; Lampit et al., 2014; Mewborn et al., 2017; Bruderer-Hofstetter et al., 2018; Webb et al., 2018; Basak et al., 2020; Gates et al., 2020; Gavelin et al., 2021; Yun & Ryu., 2022; Li et al., 2024) and executive functions (Hindin & Zelinski., 2012; Karr et al., 2014; Kelly et al., 2014; Guo et al., 2020). Kelly et al. (2014) found moderate to large ESs for executive functions and reported that effects of transfer and maintenance of intervention were most commonly reported with at least 10 adaptive training sessions and a long-term follow-up. Li et al. (2024) found no overall effect when engagement of participants < 60 % (i.e. ratio of enrolled participants to the total number of eligible subjects who were invited to participate in cognitive training), or persistence < 80 % (i.e. calculated by dividing the number of participants who completed the training and post-training assessment by the initial training group size). Findings for specific subtypes of CT or comparisons are reported below.
Computerized cognitive trainingFour meta-analyses focused exclusively on CT interventions that were performed on digital devices (Lampit et al., 2014; Webb et al., 2018; Basak et al., 2020; Gates et al., 2020) and had RCT as the study design. Webb et al. (2018) used the same dataset as Lampit et al. (2014), categorizing cognitive outcomes differently. Between 8 to 161 studies were included in each meta-analysis, with a sample size between 1183 and 13,797 and a mean age of 71.6 years. In these studies, CT had an intervention duration of 1 to 26 weeks, with a range of 10 to 120 min for each session and 1 to 7 sessions per week.
Overall, studies found a small effect of computerized CT on overall cognition. Lampit et al. (2014) and Webb et al. (2018) found moderate effects on processing speed and small effects on visuospatial function. Different from Lampit et al. (2014), Webb et al. (2018) found a small effect of computerized CT on executive functions analyzing the same dataset. Some evidence of improvement in different aspects of memory (Lampit et al., 2014; Webb et al., 2018; Gates et al., 2020). Mixed and inconclusive findings have been observed in other cognitive domains. Basak et al. (2020) found larger effect sizes for near transfer in studies with lower educational levels and with fewer cognitive outcomes.
Cognitive training combined with physical exerciseIn total, there were 4 meta-analyses structured on multimodal approaches combining CT and PE (Bruderer-Hofstetter et al., 2018; Guo et al., 2020; Gavelin et al., 2021; Wu et al., 2023), performed simultaneously or subsequently/sequentially. All selected only RCT as the study design. Between 11 to 27 studies were included in each meta-analysis, with a sample size of between 670 and 2620 and a mean age of 72.0 years. Combined CT and PE had an intervention duration of 4 to 24 weeks, with 15 to 150 min for each session and 1 to 10 sessions per week.
Studies reported a small effect of multimodal interventions for overall cognition (Bruderer-Hofstetter et al., 2018; Gavelin et al., 2021) in comparison with passive, active, and unimodal-intervention controls together. Guo et al. (2020) and Wu et al. (2023) reported small effect in comparison with controls, and no effect in comparison with unimodal intervention (either single CT or single PA) on executive functions (Guo et al., 2020) and working memory (Wu et al., 2023).
Cognitive training compared with physical exerciseIn total, there were 2 meta-analyses focused on comparing CT with PE interventions (Hindin & Zelinski., 2012; Karr et al., 2014). Hindin and Zelinski (2012) included 42 (CT: 25; PE:17) studies with pre- and post-test design and a control group, with a sample size of 3781 and a mean age of 69.2 years (CT: 69.9; PE: 67.9). Karr et al. (2014) included 46 (CT: 21; PE: 23; Both: 2) studies with any type of clinical trial, with a sample size of 2013 (CT: 1061; PE: 1038) and a mean age of 73.6 years (CT: 72.3; PE: 74.9). CT had an intervention duration of 2 to 96 weeks, with a range of 15 to 240 min for each session, and <1 to 5 sessions per week. PE had an intervention duration of 8 to 52 weeks, with a range of 30 to 120 min for each session and 1 to 5 sessions per week.
Karr et al. (2014) found a small and significant effect only for CT in overall executive functions. The largest effect found for executive functions was for problem-solving. Hindin and Zelinski (2012) analyzed aerobic physical interventions along more cognitive outcomes and found a small effect both for aerobic exercise and CT on untrained domains - far transfer for reaction time, memory and executive functions - with a better study quality associated with larger Ess.
Findings from systematic reviewsIn total, there were 20 qualitative systematic reviews structured on CT. Out of these, 9 included any form of CT (Reijnders et al., 2013; Mowszowski et al., 2016; Butler et al., 2017; Fan & Wong, 2019; Nguyen et al., 2019; Marr et al., 2020; Webb et al., 2021; Mendonça et al., 2022; Sáez-Gutiérrez et al., 2024), 6 focused only on computerized CT (Kueider et al., 2012; Shah et al., 2017; ten Brinke et al., 2017; Alnajjar et al., 2019; Masurovsky, 2020; Ishibashi et al., 2023), 3 investigated multimodal approaches combining CT and physical exercise (PE) (Law et al., 2014; Lauenroth et al., 2016; Dhir et al., 2021), 1 compared CT with PE interventions (Intzandt et al., 2021), and 1 accepted only prospective memory training (Tse et al., 2023).
Five studies selected only RCT as the study design (Reijnders et al., 2013; Butler et al., 2017; Fan & Wong, 2019; Masurovsky, 2020; Sáez-Gutiérrez et al., 2024), 5 included any pre- and post-test design with a control group (Kueider et al., 2012; Alnajjar et al., 2019; Nguyen et al., 2019; Dhir et al., 2021; Ishibashi et al., 2023), 2 included RCT and quasi-experimental studies (ten Brinke et al., 2017; Intzandt et al., 2021), 2 included any pre- and post-test design with or without a control group (Marr et al., 2020; Webb et al., 2021), 1 included RCT and non-randomized controlled trials (NRCT) (Law et al., 2014), 1 included any type of clinical trial (Lauenroth et al., 2016), 1 included RCTs and quasi-RCTs (Mowszowski et al., 2016), 1 included RCTs, quasi-RCTs and follow-up studies (Shah et al., 2017), 1 included only cohort studies (Mendonça et al., 2022), and 1 included studies that applied cross-sectional, longitudinal or both study designs (Tse et al., 2023).
Between 3 to 38 studies were included in each analysis, with a sample size between 163 and 8732 participants and a mean age of 70.6 years. In these studies, CT programs (applied with or without other interventions) had a duration of between 1 and 240 weeks, with a range of 10 to 240 min for each session and <1 to 10 sessions per week. Butler et al. (2017) and Mendonça et al. (2022) did not fully describe population age separately for HOA. Fan and Wong (2019) and Tse et al. (2023) did not fully describe intervention characteristics. Masurovsky (2020) and Dhir et al. (2021) did not fully describe either the sample or intervention characteristics. Kueider et al. (2012), Shah et al. (2017), Alnajjar et al. (2019) and Ishibashi et al. (2023) did not describe average age.
Overall, studies have found some efficacy in improvement for trained domains (Lauenroth et al., 2016; Shah et al., 2017; Butler et al., 2017; Fan & Wong, 2019; Nguyen et al., 2019; Masurovsky, 2020), memory (Reijnders et al., 2013; Shah et al., 2017; Butler et al., 2017; Fan & Wong, 2019; Marr et al., 2020; Intzandt et al., 2021; Webb et al., 2021; Mendonça et al., 2022; Tse et al., 2023), reasoning/fluid intelligence (Reijnders et al., 2013; Mowszowski et al., 2016; Shah et al., 2017; Butler et al., 2017; Fan & Wong, 2019; Marr et al., 2020), executive functions (Reijnders et al., 2013; Butler et al., 2017; Marr et al., 2020), attention (Reijnders et al., 2013; Shah et al., 2017; Butler et al., 2017), processing speed (Kueider et al., 2012; Shah et al., 2017; Butler et al., 2017), global cognition (Reijnders et al., 2013; Fan & Wong, 2019; Ishibashi et al., 2023), and for daily functioning in the most recent studies (Fan & Wong, 2019; Sáez-Gutiérrez et al., 2024).
Findings for specific subtypes of CT or comparison are reported below.
Computerized cognitive trainingIn total, 6 qualitative analyses focused exclusively on CT interventions that were performed on digital devices (Kueider et al., 2012; Shah et al., 2017; ten Brinke et al., 2017; Alnajjar et al., 2019; Masurovsky, 2020; Ishibashi et al., 2023). Three studies included any pre- and post-test design with control group (Kueider et al., 2012; Alnajjar et al., 2019; Ishibashi et al., 2023), 1 included RCTs and quasi-experimental trials (ten Brinke et al., 2017), 1 included RCTs, quasi-RCTs and follow-up studies (Shah et al., 2017), 1 included only RCTs (Masurovsky, 2020).
Between 6 to 38 studies were included in each analysis, with a sample size of between 163 and 5381 participants and average ages between 50 and 96 years. Among these, computerized CT interventions had a duration between 1 and 68 weeks, with 15 to 240 min for each session, and 1 to 7 sessions per week. Masurovsky (2020) did not fully describe the sample and intervention characteristics. Only ten Brinke et al. (2017) described the mean sample age.
Overall, there was some evidence of post-intervention improvement in trained cognitive domains (Kueider et al., 2012; Shah et al., 2017; Masurovsky, 2020). Kueider et al. (2012) found moderate to large effects in classical CT, neuropsychological software (NS), and video games (VG) for processing speed, and moderate effects of CT and VG for reaction time. Masurovsky (2020) reported that none of the included studies (published between 2016 and 2018) that found effects for far transfer have measured participants' expectations, and only one used active control. Shah et al. (2017) found good quality evidence of far transfer for Instrumental Activities of Daily Living and Health-related quality of life only in > 5 years of follow-up.
Cognitive training combined with physical exerciseThree qualitative systematic reviews were structured on multimodal approaches combining CT and PE (Law et al., 2014; Lauenroth et al., 2016; Dhir et al., 2021), performed both simultaneously (simul.) or sequentially/ subsequently (seq.). Law et al. (2014) selected RCT and non-randomized clinical trials as the study design and included 3 studies, with a sample size of 480 and a mean age of 71.6 years. Combined CT and PE performed sequentially had an intervention duration of 8 to 48 weeks, and a session duration of 10 to 150 min (CT) + 45 to 150 min of PE. Frequency varied from 1 to 2 CT sessions plus 1 to 3 PE sessions per week.
Lauenroth et al. (2016) selected RCT and clinical trials as the study design and included 13 studies (simul.: 7; seq.: 6) with a sample size of 883 (simul.: 308; seq.: 575) and a mean age of 74.1 years (simul.: 72.5; seq.: 75.6). Combined CT and PE had an intervention duration of 4 to 30 weeks (simul.: 4 - 25; seq.: 8 - 30). Session duration varied within 30 to 60 min of CT and PE performed simultaneously, or within 10 to 90 min of CT plus 30 to 60 min of PE performed sequentially. Frequency varied from 1 to 5 days of simultaneous training per week, or 1 to 5 CT sessions plus 1 to 4 PE sessions per week.
Dhir et al. (2021) included any pre/post test with the control group but did not fully describe either the sample or intervention characteristics. They also did a meta-analysis, but separate meta-analytic data for healthy older adults were unavailable.
Most studies included in Lauenroth et al. (2016) reported post-intervention improvements at least in the trained cognitive function. Law et al. (2014) and Dhir et al. (2021) had limited findings given the small number of studies included for the population of interest.
Cognitive stimulationFindings from meta-analysisThere was 1 meta-analysis structured on cognitive stimulation (CS) which included RCTs analyzing CT, CS and mixed interventions of CS with CT (Yun & Ryu., 2022). The authors included 11 CS studies and 1 study with a mixed intervention using CS and CT. They found a small effect with substantial heterogeneity for overall cognitive functioning and did not describe sample sizes or intervention characteristics separately for HOA or CS studies.
Findings from systematic reviewsThere were 3 qualitative reviews structured on CS (Reijnders et al., 2013; Kelly et al., 2014; Sáez-Gutiérrez et al., 2024), which included 18 RCTs. CS interventions had a duration between 4 and 96 weeks, with 30 to 240 min for each session, and <1 to 4 sessions per week. Reijnders et al. (2013) found 8 CS studies, including 1088 participants with 73.7 years of age on average. Kelly et al. (2014) found 8 CS studies, including 905 participants with 60 to 93 years of age. Both reviews reported mixed findings for cognitive outcomes. Sáez-Gutiérrez et al. (2024) found 2 CS studies, including 144 participants with 73 years of age on average; they found no effect of both interventions on daily functioning.
Multimodal interventionsAlso, there was 1 qualitative review structured on multimodal interventions in general, defined by the authors as “multicomponent approaches that combine two or more intervention strategies” (Kim et al., 2022, p.2). Six RCTs were included. The sample size was 1102 and the mean age was 74.8 years. Multicomponent programs had a duration between 6 and 24 weeks, with 20 to 150 min for each session, and <1 to 2 sessions per week. Results underlined some efficacy of occupational plus physical therapy, and cognitive-behavioral therapy plus Baduanjin qigong (a set of eight qigong practices that are a part of traditional Chinese medicine and include either movement or contemplative breathing practices), on ADLs and IADLs. CT multicomponent interventions that involve diverse types of CT resulted in mixed findings regarding IADL outcomes.
DiscussionThis meta-review summarizes existing evidence regarding cognitive training, cognitive stimulation, multimodal and multicomponent protocols aimed at preventing or reducing cognitive decline in HOA. The most frequent flaws in the available knowledge were revealed through a rigorous quality assessment. Meta-analyses and narrative reviews were analyzed separately, contributing to a comprehensive understanding of the field.
Results indicated CT interventions as the most promising ones, considering the number of included studies and corresponding effect sizes. Results from meta-analysis reviews suggested larger CT effects for speed of processing, which was found to be a predictor for functional decline or high-functioning cognitive aging (Wahl et al., 2010; Ticha et al., 2023). Moreover, CT has shown moderate effects on long-term and working memory, with the latter having, potentially, a role in encoding and retrieval and being associated with episodic memory performance (Bosnes et al., 2020; Melrose et al., 2020). However, vast heterogeneity of effect sizes suggests important mediators need to be further investigated.
An important issue in relation to CT is the capacity to generalize the skills acquired, namely transfer (Sala et al., 2019). Overall, qualitative systematic reviews provided more evidence for near transfer. The distinction between near and far transfer as described by Barnett and Ceci (2002) is not simple, but generally signifies the generalization of skills in similar domains/tasks, and the transfer of skills in domains/tasks that are not or very weakly related to each other. One example of far transfer is the effect on everyday functioning.
However, far transfer and effects on everyday functioning – which are clinically more significant – were under-investigated. In Shah et al. (2017), evidence of far transfer could be observed only some years after training, which represents cognitive decline prevention instead of an actual improvement. The fact that most studies only examined immediate effects suggests a systematic bias. According to the evidence collected, near transfer could have an immediate impact, which could potentially prevent cognitive decline years later. Nevertheless, the two most recent systematic reviews that analyzed daily functioning found consistent immediate improvement for daily functioning (Fan & Wong, 2019; Sáez-Gutiérrez et al., 2024).
Two reviews examined commercial computerized cognitive training. Shah et al. (2017) and Nguyen et al. (2021) observed improvements in processing speed but highlighted the lack of direct evidence supporting clinically significant outcomes. Shah et al. (2017) noted near transfer effects in most trials, with some indication of far transfer effects at least 5 years post-training, albeit based on data from only one commercial program. The fast expansion of this market (Market Research Report, 2020) has outpaced the evidence supporting these interventions.
A vast diversity of intervention durations, session durations and frequencies were presented. Based on the included meta-analyses, an effective pattern seems to include adaptive training with 10 sessions or more (Kelly et al., 2014), delivered <3 times a week in groups (Lampit et al., 2014). The findings are in line with the cognitive training employed in the FINGER study, the first long-term RCT to demonstrate the efficacy of multidomain lifestyle interventions in reducing cognitive decline among older adults at a higher risk of dementia (Ngandu et al., 2015; Rosenberg et al., 2019). The computer-based training took place for two 6-month periods, during which participants attended 72 sessions of the adaptive CT program, three times a week (Kivipelto et al., 2013).
Nonetheless, a program with a slightly different population had different conclusions. In an analysis published by Andrieu et al. (2017), they investigated the effects of a multidomain intervention and polyunsaturated fatty acids supplementation, either alone or in combination. CT consisted of 12 group sessions lasting 60 min each, with reasoning and memory training. In the first month, there were two sessions per week, while in the second month, there was only one session per week. Over the course of 3 years, there were no significant effects on cognitive decline in older people with memory complaints.
In addition, there was limited evidence for further benefits when combining cognitive training with physical activity. Small improvements were found for combined interventions when compared to controls, but this effect was not consistent when compared to unimodal intervention (either CT or PE). Also, when considered individually, CT yielded more consistent results than PE. This is consistent with a recent meta-analysis which found no significant differences between combined interventions and cognitive activity alone (Gheysen et al., 2018). However, physical activity has been largely recognized to improve a myriad of health outcomes, prevent several chronic medical conditions, enhance mobility and cognition, and promote independent functioning (Penedo & Dahn, 2005; Warburton & Bredin, 2017; Eckstrom et al., 2020).
Moreover, it influences cognitive functions and neuronal mechanisms that are most at risk of age-related changes, such as attention, executive functions and episodic memory (Blanchet et al., 2018) being associated with a reduced risk of developing cognitive impairment (Erickson et al., 2019). Physical activity even prevents the progression of cognitive deficits and/or improves psychological well-being in people with diagnosed mild cognitive impairment or dementia (Blanchet et al., 2018; Du et al., 2018; Nuzum et al., 2020).
Considering the vast evidence of the benefits of physical activity for a number of health outcomes, the lack of findings in the current review may indicate a ceiling effect of interventions on short-term outcomes. All included reviews analyzing interventions combining or comparing PA and CT only considered immediate post-intervention effects. A future review that examines combined interventions and considers long-term outcomes could possibly aid in elucidating this question. On the other hand, the heterogeneity of the combined arrangements may be concealing the effect of the most effective models, which could be addressed by expanding evidence with further moderator analysis.
For cognitive stimulation and multicomponent interventions, it was not possible to find a shared effect. This can be attributed to the vast heterogeneity of stimulation interventions developed and the relatively small number of studies included in each analysis. Alternatively, it could be that the majority of already designed protocols did not include the appropriate features for stimulating cognitive plasticity in the healthy population. Gómez-Soria et al. (2023) carried out a systematic review and meta-analysis about cognitive stimulation and found improvements in general cognitive functioning for healthy older adults. However, this review included only two studies for this subgroup analysis, combining effects of different tests and follow-ups.
The lack of evidence for CS effects on HOA contrasts with the actual guidance for people with established cognitive decline. World Alzheimer Report 2022 recommends Cognitive Stimulation Therapy (CST; Spector et al., 2003) as a best practice to improve cognitive function in people with mild to moderate dementia (Gauthier et al., 2022). Beyond the cognitive gains, CST is recognized to be cost effective and was shown to be feasible in low-resource settings (Gauthier et al., 2022). It is possible that a CS protocol that complies with specific appropriate principles could be advantageous for the healthy population according to this literature. Given the multiple possibilities that the term 'cognitive stimulation' can encompass, it could be that the most effective protocol has yet to be created.
Expanding the number of studies on CS and multicomponent interventions is necessary to draw a more comprehensive panorama in the future. For example, physical activity that is either linked to or separate from cognitive interventions, despite limited current evidence, may be used as well. Other examples of future research can be carried out in an exploratory way, applying different theoretical principles to achieve this goal, for example: (1) studying the effect of cognitive stimulation on processing speed and working memory, to increase the comparability between cognitive stimulation and cognitive training studies, (2) using a more rigorous definition of cognitive stimulation, due to the fact that many of the primary studies included here involved just one leisure activity and labeled it as cognitive stimulation, making it difficult to compare studies with different interventions, or (3) adapting what has already been learned in the area of cognitive stimulation into a preventive strategy for people with cognitive decline.
The main limitations of this meta-review were the quality and risk of bias of included studies. However, this was due to a previous limitation of the reviews included here, suggesting an intrinsic and systemic limitation of the actual state of art of this field. Future investigations should select a proper method for assessing risk of bias (RoB) and provide a satisfactory discussion of its implications. Another potential limitation was the vast range of interventions and methodologies included, which may have led to high heterogeneity and difficulty to summarize results. The broad inclusion criteria provided a wide perspective about the field but may have limited comparability between results. This limitation was addressed by providing separate results.
ConclusionThe current evidence supports CT activities more decisively, with at least 10 adaptive sessions delivered less than three times weekly in group meetings and encourages ongoing research into CS and multicomponent protocols. Nevertheless, the issue related to the transfer of effects for clinical outcomes remains under-investigated, with urgent need for its examination both short and long-term. Longer follow-ups seem to be a key issue to find combined and clinically significant results. Rigorous risk of bias and quality assessment is necessary to improve current evidence on cognitive interventions.
GlossaryActive Control: a standard treatment that is comparable to the intervention is given.
ADLs: activities for daily living, including basic, instrumental and advanced activities.
Attention: ability to direct cognitive resources towards specific targets.
Daily functioning: basic daily home and work requirements, including ADLs.
Executive Functions: abilities associated with specific high-level cognitive processes.
Global Cognitive Function: a composite index combining a range of abilities across domains.
IADLs: instrumental activities of daily living; activities essential to function autonomously.
Memory: ability to retain information or representations of past experiences.
Meta-analysis: a technique that uses quantitative data to synthesize results of multiple studies.
Other Intervention: group for comparison that receives an alternative intervention of interest.
Passive Control: group for comparison that receives no intervention or only treatment as usual.
Processing Speed: the speed of nonverbal processing.
Qualitative Systematic Review: a review that uses a systematic and explicit methodology to identify, select, and critically evaluate the results of studies included.
Quality of Life: measures how much a person enjoys life.
Reaction Time: the interval between the beginning of a stimulus and a specific response.
Setting: the place where the program is conducted.
Trained Domains: the cognitive domains that were trained during the intervention/program.
Visuospatial Function: ability to perceive the spatial features of a figure or object.
Working Memory: ability to briefly retain information in a highly accessible state.
Data statementConsidering that this is a systematic meta-review of systematic reviews, primary data are fully available in these previously published primary reviews.
This work was supported by the Fundação Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), the Conselho Nacional de Pesquisa (CNPq), and the Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ). Funding sources had no involvement in the study design, data collection, analysis and interpretation of data, writing of the report and decision to submit the article for publication.