The majority of pancreatic tumours are primary, with ductal adenocarcinoma being the main histological lineage. Invasion by metastasis of tumours from other organs is a rare clinical finding, accounting for <2% of pancreatic cancers. Renal cell carcinoma is the primary cancer which most commonly spreads to the pancreas, followed by colorectal cancer, melanoma, breast cancer and lung cancer. Cases of pancreatic metastasis from sarcoma are limited and can be a diagnostic and therapeutic challenge due to their rarity and the difficulty in distinguishing between primary and metastatic tumours.1 We present the cases of two patients diagnosed with pancreatic metastasis from sarcoma.
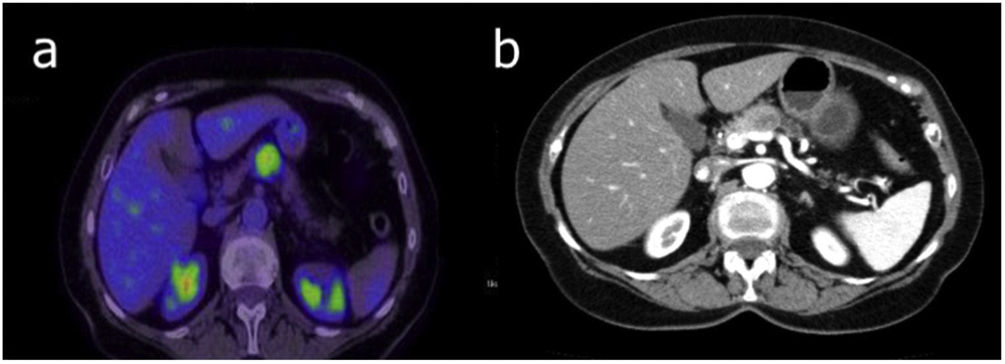
Case 1. This was a 76-year-old woman who had a hysterectomy, double adnexectomy and bilateral iliac lymphadenectomy in 2019 for an 18-cm, high-grade endometrial tumour with sarcomatous degeneration. Postoperative period was uneventful, Clavien-Dindo I. Histology was consistent with subserous uterine leiomyosarcoma T2N0M0, vimentin +++, S100 −, actin ML +++, Ki67 40%. She was started on adjuvant chemotherapy with adriamycin–dacarbazine. At nine months follow-up computed tomography (CT) (Fig. 1) detected a mass measuring 2 × 2 × 1.9 cm with dilation of the main pancreatic duct and pathological uptake in positron emission tomography (PET)/CT (Fig. 1) and left gluteus maximus. Endoscopy confirmed sarcoma metastasis. The patient had a laparoscopic distal pancreatectomy (head and tail) + splenectomy and gluteal mass resection, both compatible with leiomyosarcoma metastasis. She did not receive subsequent adjuvant therapy and after one year of follow-up there is no evidence of recurrence.
Case 2. This was a 67-year-old patient operated on in 1969 for retroperitoneal spindle cell synovial sarcoma, with multiple recurrences over the course of follow-up: pulmonary in 1989, 1991, 2001 and 2010 (atypical lung resection); right femur in 2005 (resection and prosthesis); retroperitoneum with gastric, adrenal and right kidney infiltration in 2012 (total gastrectomy, left nephrectomy and adrenalectomy, and resection of the splenic flexure of the colon); and body of the pancreas in 2017 (distal pancreatectomy + splenectomy). The pathology report on all the lesions confirmed recurrence of spindle cell synovial sarcoma. The patient died as a result of nosocomial pneumonia in the postoperative period of the last surgical intervention.
Pancreatic metastases from sarcoma are asymptomatic in 20%–60% of cases. The diagnosis is usually made incidentally or during follow-up of the primary cancer. Where they do cause symptoms, the main ones are abdominal pain and obstructive jaundice.2 Improvements in the treatment and survival of patients with sarcoma are increasing the frequency of detection of metastasis in unusual sites. However, no standard treatment regimen has been established for pancreatic metastatic sarcoma. The increasing reporting of cases in the scientific literature is helping to improve knowledge of this disease and, added to the decrease in morbidity and mortality rates associated with pancreatic surgery, means a surgical approach is an option in a large number of cases.3
The patient selection criteria for pancreatic surgery should include: type of primary cancer associated with a good outcome; control of the primary tumour; absence of extra-pancreatic metastatic disease; resectability of the lesions; and suitability of the patient in terms of tolerating the pancreatectomy.4 Although there are reports of cases of enucleation or parenchyma-sparing pancreatectomy, the usual surgical approach is pancreaticoduodenectomy or distal pancreatectomy.
The benefit of surgery in terms of survival has been found for renal cell carcinoma metastasis, whereas for other primary tumours, such as lung and breast cancers, the role of surgery is primarily palliative. Essentially, resection of pancreatic metastatic sarcoma is only justified in very select patients.
Patients with pancreatic metastasis must be assessed by a multidisciplinary committee, with surgery being a part of the multimodal treatment. More studies are needed to establish how to combine surgery with medical treatments in the different metastatic diseases of the pancreas.5
FundingThe authors have no sources of funding to declare.
Conflicts of interestThe authors declare that they have no conflicts of interest.