Biliary papillomatosis is a rare type of papillomatosis. Depending on the location of the disease, radical surgical resection or liver transplants are the treatment of choice. These radical surgical options may be unrealistic in patients who are not surgical candidates or who are unwilling to consider surgery.
AimsTo evaluate the effectiveness of endoscopic electrocoagulation for the biliary papillomatosis.
MethodsIn this case series, we report six patients with unresectable biliary papillomatosis who underwent cholangioscopic electrocoagulation using needle knife and their clinic follow up information.
ResultsAfter patients received cholangioscopy with electrocoagulation of the residual biliary papilloma, the daily T-tube drainage volume increased to 200–400ml with improvement in the drainage content and significant relief of clinical symptoms, such as jaundice and abdominal pain.
ConclusionThis method of using electrocoagulation to directly target and destroy tumor tissue is a safe and effective alternative for those with unresectable disease, and this method has shown to enhance T-tube drainage volume and improve patients’ overall clinical symptoms.
La papilomatosis biliar es un tipo raro de papilomatosis. Dependiendo de la localización de la enfermedad, la resección quirúrgica radical o los trasplantes de hígado son el tratamiento de elección. Estas opciones quirúrgicas radicales pueden ser poco realistas en pacientes que no son candidatos a la cirugía o que no están dispuestos a considerarla.
ObjetivosEvaluar la eficacia de la electrocoagulación endoscópica para la papilomatosis biliar.
MétodosEn esta serie de casos, informamos de 6 pacientes con papilomatosis biliar irresecable que fueron sometidos a electrocoagulación colangioscópica mediante bisturí de aguja, y de su información de seguimiento clínico.
ResultadosDespués de que los pacientes recibieran la colangioscopia con electrocoagulación del papiloma biliar residual, el volumen de drenaje diario del tubo en T aumentó a 200-400ml con mejora del contenido del drenaje y alivio significativo de los síntomas clínicos, como la ictericia y el dolor abdominal.
ConclusiónEste método de uso de la electrocoagulación para apuntar directamente y destruir el tejido tumoral es una alternativa segura y eficaz para aquellos con enfermedad no resecable, y este método ha demostrado mejorar el volumen de drenaje del tubo T y mejorar los síntomas clínicos generales de los pacientes.
Biliary papillomoatosis (BP) is a rare type of papillomoatosis that was initially described by Chappet in 1894.1,2 The etiology and pathogenesis remains unknown.3 This rare disease entity is characterized by multiple papillary (villous) excrescences producing blood, mucous and cell debris leading to dilation of the bile duct.2,4 BP often occurs in middle-aged men with a male-to-female ratio of 2:1.3,5–7 The initial diagnosis of BP is challenging due to its none-specific clinical presentations of jaundice, recurrent cholangitis, abdominal pain, and laboratory tests which often mimic choledocholithiasis.6,8 It is imperative that BP receives prompt diagnosis as it carries high mortality rate and malignant transformation in approximately 35–64% of the cases in addition to septic complications and progression from biliary cirrhosis to liver failure.2,5,9–11,8,12,17
Modern cross-sectional image studies are often inadequate in making conclusive diagnosis since these modalities often show bile duct filling defects or choledocholithiasis.2,10,13–15 However, recent advancements in endoscopic retrograde cholangiopancreatography (ERCP), cholangioscopy and intra-operative ultrasound have become important adjuncts in making the elusive BP diagnosis and in determining resectability.8,16 Depending on the location of the disease, radical surgical resection or liver transplants are the treatment of choice.17 These radical surgical options may be unrealistic in patients who are not surgical candidates or who are unwilling to consider surgery. In this group of patients alternate treatment options such as local ablative procedures, palliative stenting and drainage may be feasible. These modalities can be performed with ERCP or cholangioscopy.11,13,18,19
In this case series, we report six patients with unresectable BP who underwent cholangioscopic electrocoagulation using needle knife and their clinic follow up information.
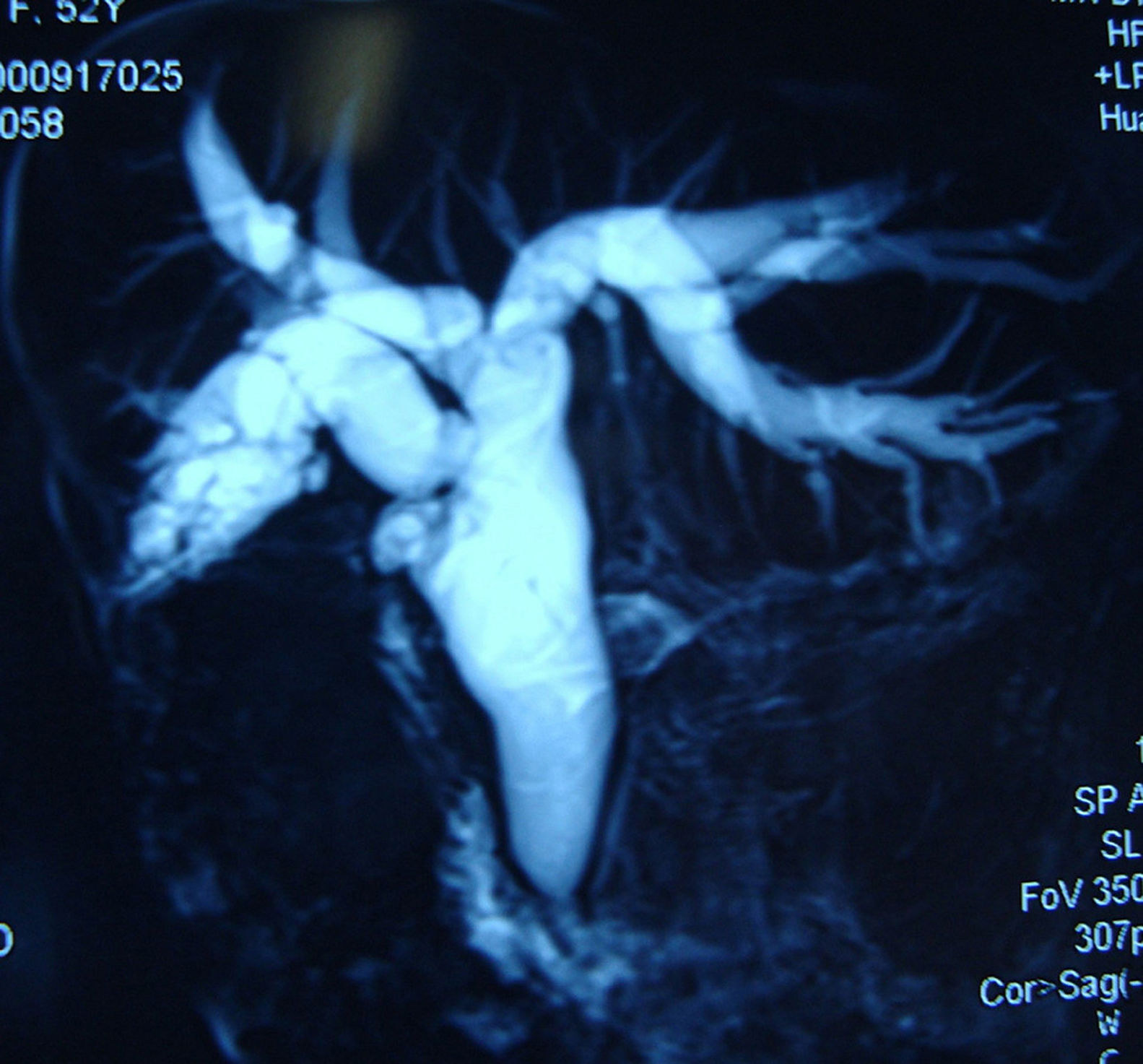
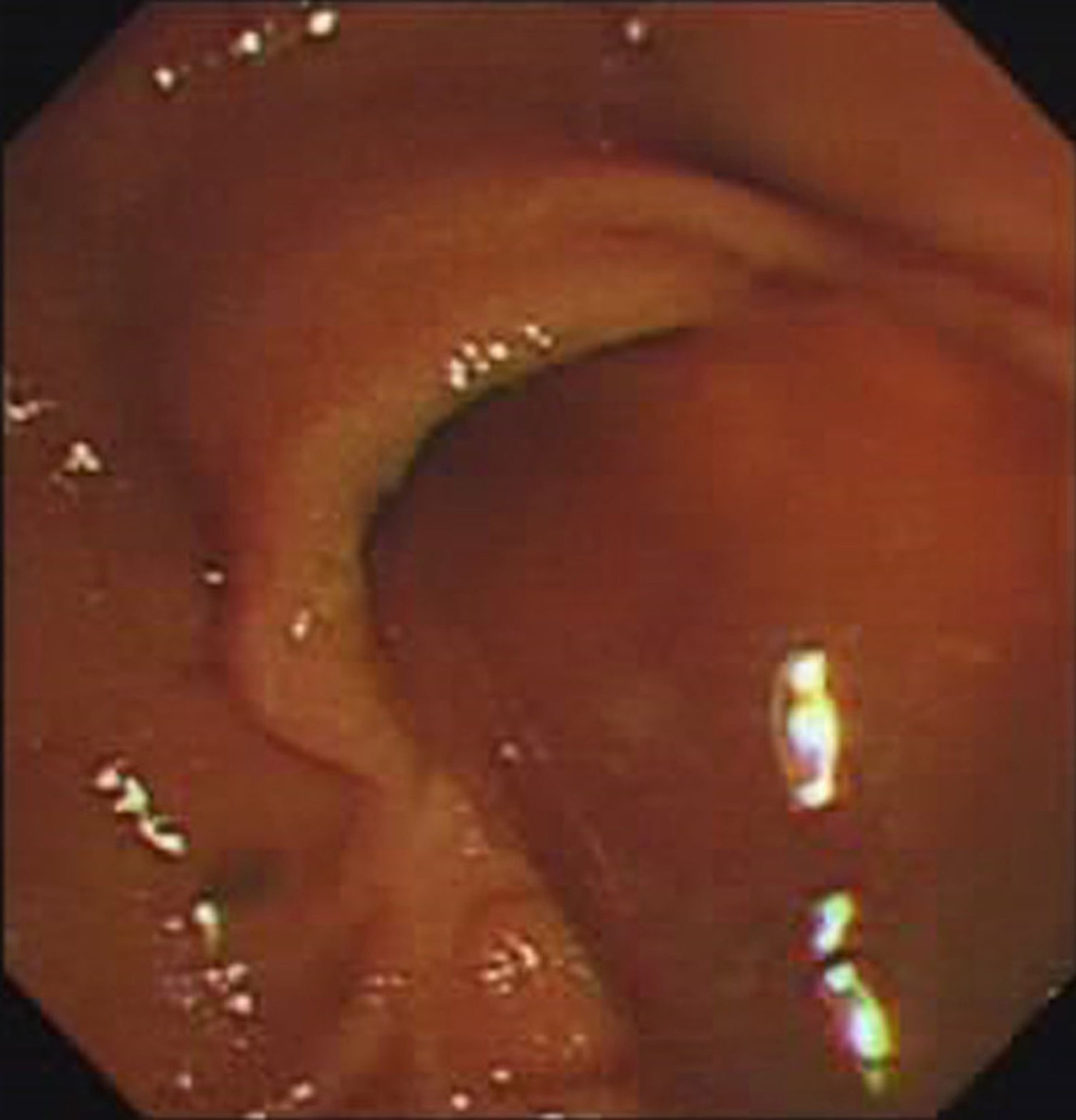
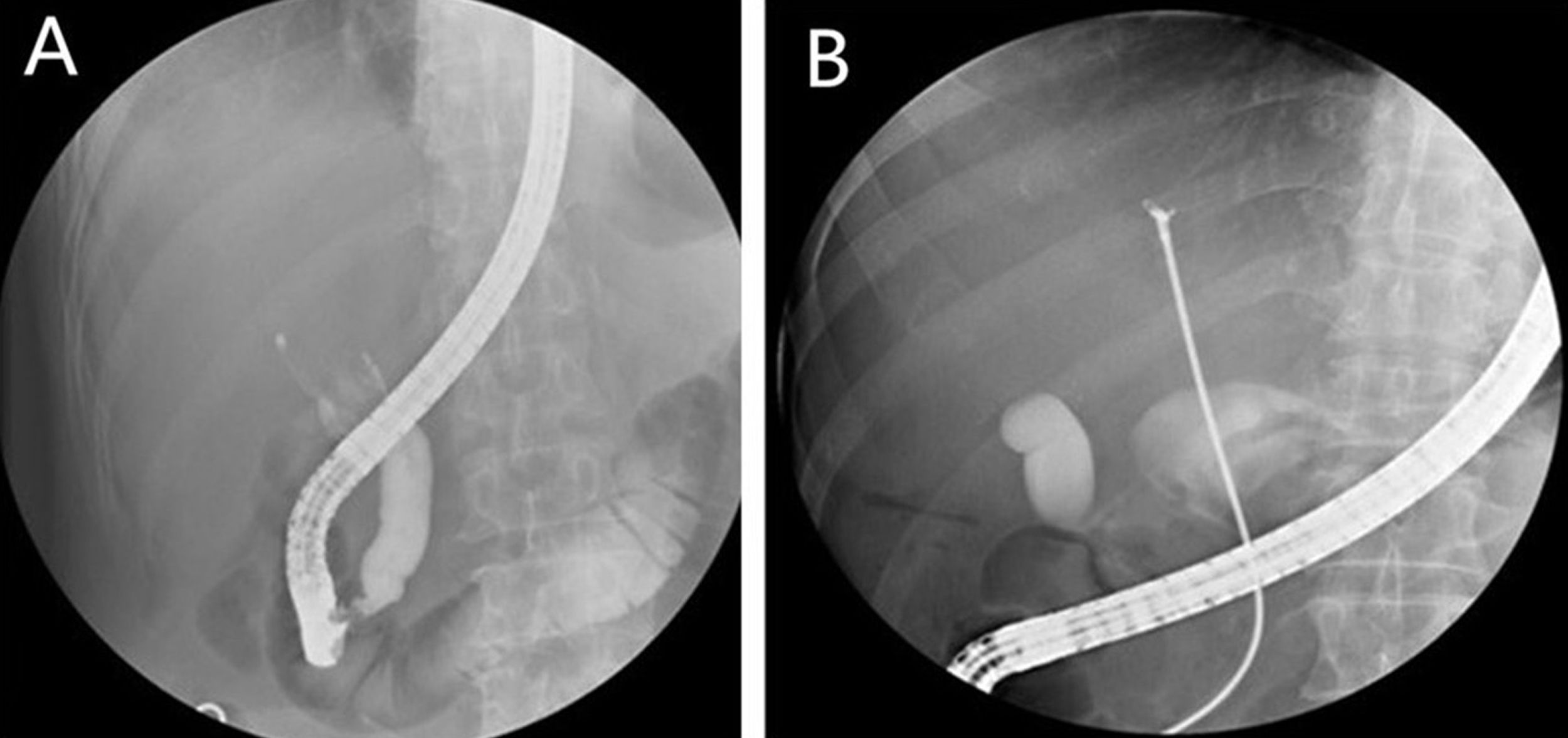
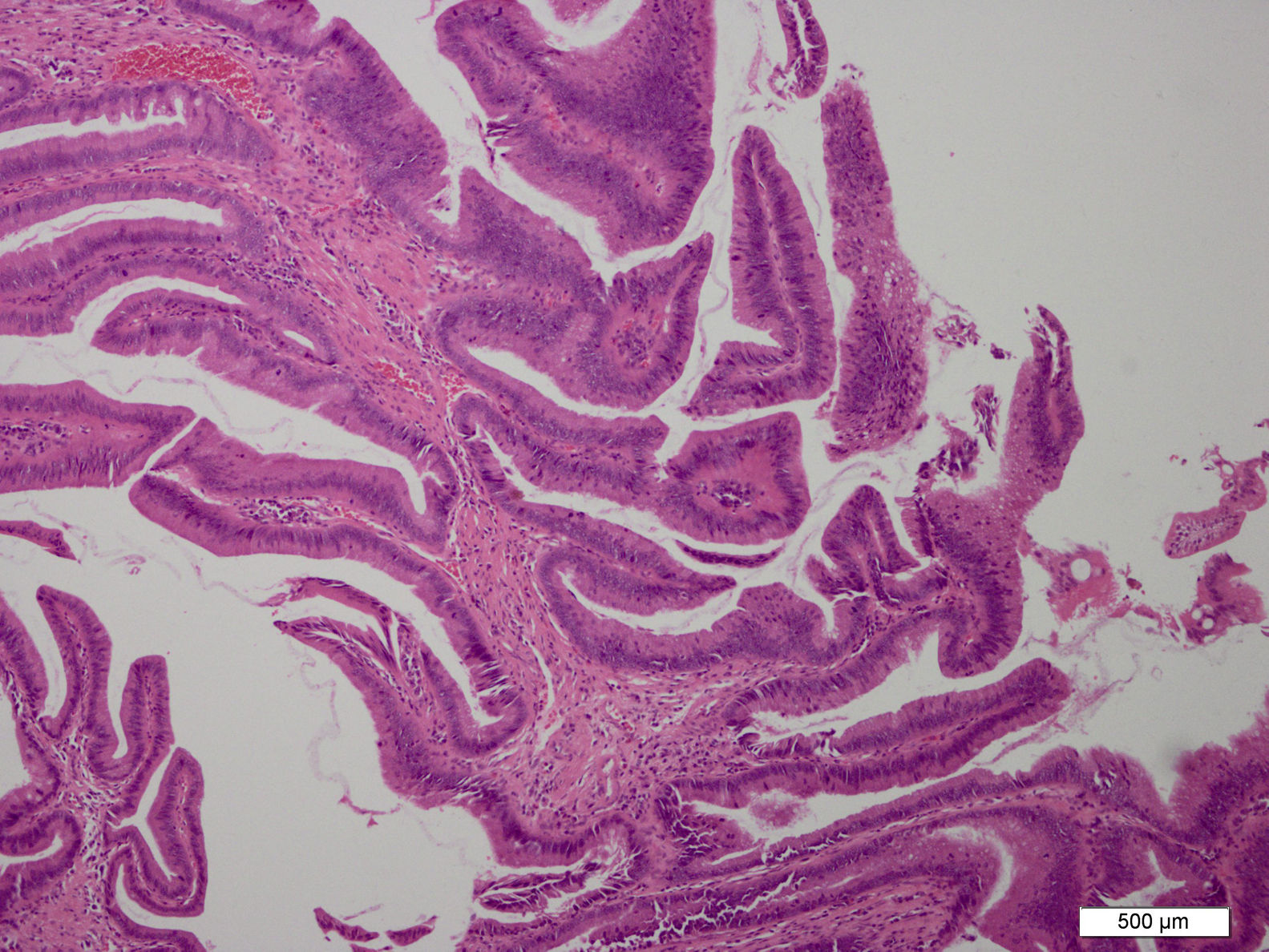
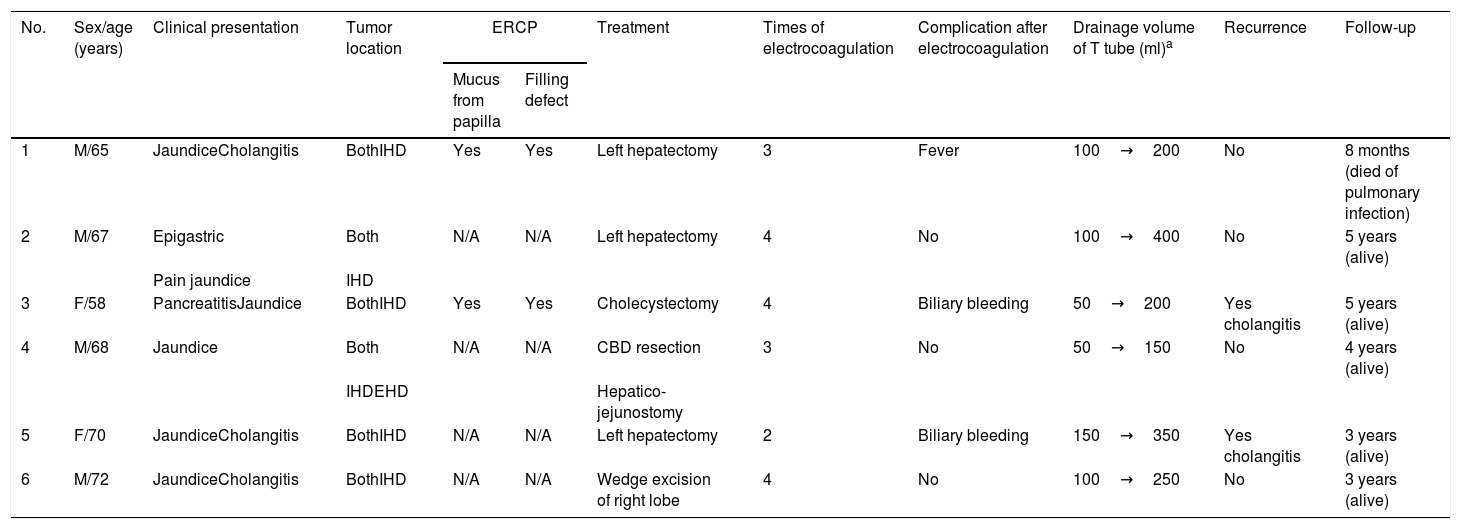
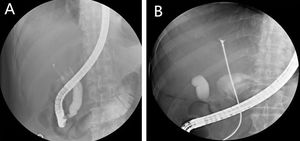
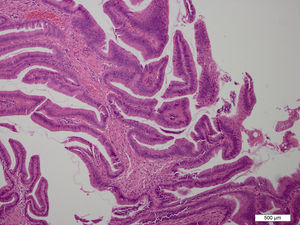
MethodsSix patients with histological diagnosis of BP were treated with cholangioscopic electrocoagulation at West China Medical Center (Sichuan, PR China) from October 2011 to January 2014. Patient details are summarized in Table 1. All six patients showed both intrahepatic and extrahepatic dilations on both CT and MRI (Fig. 1). Patient 1 and patient 2 underwent pre-operative ERCP with characteristic finding of the classic “fish-eye appearance” at the ampulla of Vater (Fig. 2). Subsequent cholangioscopy showed persistent intrahepatic and extrahepatic biliary dilations and irregular filling defects despite vigorous washing (Fig. 3A). These areas underwent extensive bile duct biopsy under fluroscopy (Fig. 3B). The biopsy specimens showed benign papillary adenomas of biliary type without dysplasia in histopathologic examination, confirming the diagnosis of BP (Fig. 4).
Details of patients with biliary papillomatosis.
| No. | Sex/age (years) | Clinical presentation | Tumor location | ERCP | Treatment | Times of electrocoagulation | Complication after electrocoagulation | Drainage volume of T tube (ml)a | Recurrence | Follow-up | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mucus from papilla | Filling defect | ||||||||||
| 1 | M/65 | JaundiceCholangitis | BothIHD | Yes | Yes | Left hepatectomy | 3 | Fever | 100→200 | No | 8 months (died of pulmonary infection) |
| 2 | M/67 | Epigastric | Both | N/A | N/A | Left hepatectomy | 4 | No | 100→400 | No | 5 years (alive) |
| Pain jaundice | IHD | ||||||||||
| 3 | F/58 | PancreatitisJaundice | BothIHD | Yes | Yes | Cholecystectomy | 4 | Biliary bleeding | 50→200 | Yes cholangitis | 5 years (alive) |
| 4 | M/68 | Jaundice | Both | N/A | N/A | CBD resection | 3 | No | 50→150 | No | 4 years (alive) |
| IHDEHD | Hepatico-jejunostomy | ||||||||||
| 5 | F/70 | JaundiceCholangitis | BothIHD | N/A | N/A | Left hepatectomy | 2 | Biliary bleeding | 150→350 | Yes cholangitis | 3 years (alive) |
| 6 | M/72 | JaundiceCholangitis | BothIHD | N/A | N/A | Wedge excision of right lobe | 4 | No | 100→250 | No | 3 years (alive) |
All six patients fixed T-tube (at least 20Fr) drainage post-operation. The daily bile flow was between 50ml and 150ml. Mucous was found in all the drainage content and serum bilirubin remained persistently elevated. Cholangioscopy with electrocoagulation (VIO 200S, ERBE, German. Endo cut Q mode, coagulation current, 40W) of the residual papilloma with high frequency electric needle knife (Olympus, Japan) was performed in 6–8 weeks post-operation (Video 1). At the beginning of cholangioscopy, we pulled out the T-tube, the cholangioscope (Fuji, Japan) went through the sinus tract formed by T-tube into the common bile duct. As usual, T-tube drainage was replaced post therapy and another cholangioscopic treatment was performed one week after endoscopic treatment. The maximum numbers of endoscopic treatments was four times.
ResultsAfter patients received cholangioscopy with electrocoagulation of the residual biliary papilloma, the daily T-tube drainage volume increased to 200–400ml with improvement in the drainage content and significant relieve clinic symptoms, such as jaundice and abdominal pain. However, patient No.1 developed fever of 101.3°F (38.5°C) three days post-operative that was conservatively treated. Patient No. 3 and No. 5 developed a small amount of biliary bleeding that spontaneously resolved without treatment.
These patients were followed for three to five years. Patient Nos. 2, 4 and 6 did not have any recurrent jaundice or abdominal pain. Patient No. 3 and No. 5 developed recurrent cholangitis one year post cholangioscopic treatment. Patient No. 1 was followed for 8 month prior to succumb to severe pulmonary infections.
DiscussionFollowing advancement in endoscopy, ERCP and cholangioscopy are now the modality of choice in making the BP diagnosis.20,21 The characteristic findings of BP during ERCP include excessive mucous discharge observed from the papilla in addition to the multiple filling defects found during cholangioscopy.22,23 Diagnosis of BP can often be made by bile duct biopsy.
BP is in fact premalignant disease with high malignancy potential and high rate of recurrence.2,5,8,9 Therefore, surgical resection or liver transplant are often recommended due to its high malignant transformation and diffuse pattern of the disease.10,24 Recently, new approaches such as percutaneous cholangioscopic laser ablation, iridium-192 intraluminal therapy, and photodynamic therapy and argon plasma coagulations are shown to improve survival.25–28
Here, we report that all six patients had diffuse BP involving bilateral hepatic lobes, which make radical surgical resection impossible. Among them, four patients that underwent partial hepatectomy in lobes with higher disease burden should be considered as tumor reduction surgery, therefore there were still residual diseases in the remaining livers. These patients all underwent post-operative cholangioscopic electrocoagulation in effort to destroy the residual tumor, to decrease mucous secretion, to enhance bile drainage, and to improve liver function as well as clinical symptoms.
During the operation of cholangioscopic electrocoagulation within the bile duct, it is vital that the tip of the needle knife is close to or gently touch the target lesion, do not press the lesion or bile duct wall with force as this maneuver will result in increased risk of bleeding and biliary tract perforation. Electrocoagulation current can be used to destroy tumor tissue. When working, sparks can be seen at the tip of the needle knife under endoscope. As long as the spark contacts the lesion, the lesion can be destroyed. Alternative method such as argon plasma coagulation (APC) can be also considered, but APC does not fit into the cholangioscopy and the water used during cholangioscopy procedures will create large amount of bubbles that would affect procedure.
ConclusionThis cases series demonstrate that cholangioscopic electrocoagulation is a feasible therapeutic option for patients who are not candidates for surgical intervention of biliary papillomatosis. This method of using electrocoagulation to directly target and destroy tumor tissue is a safe and effective alternative for those with unresectable disease, and this method has shown to enhance T-tube drainage volume and improve patients’ overall clinical symptoms. Further studies are needed to further investigate the safety and efficacy of this method in the treatment of biliary papillomatosis.
Author contributionsFind the patient and get the idea: Chuncheng Wu, MD; Bing Hu, MD.
Performed the treatment: Chuncheng Wu, MD; Bing Hu, MD; Qiongying Zhang, RN.
Collected the information the patient: Chuncheng Wu, MD; Qiongying Zhang, RN; Ke Liao, MS.
Collected the figure of the patient: Chuncheng Wu, MD; Qiongying Zhang, RN; Ke Liao, MS.
Discussed the diagnose and treatment for the patient: Chuncheng Wu, MD; Juliana F. Yang, MD; Qiongying Zhang, RN; Wei Liu, MD; Bing Hu, MD.
Analysis and interpretation of the data of the patient: Chuncheng Wu, MD; Juliana F. Yang, MD; Qiongying Zhang, RN; Wei Liu, MD; Bing Hu, MD.
Drafted and revised the article: Chuncheng Wu, MD; Juliana F. Yang, MD; Ke Liao, MS; Bing Hu, MD.
Final approval of the article: Chuncheng Wu, M.D.; Juliana F. Yang, M.D.; Qiongying Zhang, RN; Wei Liu, M.D.; Bing Hu, M.D; Ke Liao, M.S.
Conflict of interestAll authors have no conflicts of interest to disclose.
The authors want to thank Sichuan Province Science and Technology Department (China) (2018SZ0134) for their support.Financial disclosure
All authors have no financial relationships relevant to this article to disclose.