Streptococcus pneumoniae (Sp) is the main cause of community-acquired pneumonia in the elderly, hence the importance to establish the prevalence of nasopharyngeal colonization by different Sp serotypes in adults.
Methodsfrom December 2009 to June 2010, nasopharyngeal cultures were taken from adults living in rural communities in Mexico for the isolation and serotyping of Sp by the Quellung reaction. Penicillin and ceftriaxone susceptibility tests were performed by the microdilution method.
Resultstwo hundred and thirty-six adults over 50 years old, were included. The prevalence of colonization by Sp was 21.6%. The most frequent serotypes were 19A (21%), 6A (13%), 6B and 11A (11%). All isolates were susceptible to ceftriaxone, and 52.8% of the isolates showed penicillin minimal inhibitory concentrations ≥0.12mg/L.
Conclusionthis is the first study analyzing the nasopharyngeal colonization by Sp in adults in Mexico. Serotypes not included in any of the pneumococcal vaccines were frequently identified.
Streptococcus pneumoniae (Sp) es la principal causa de neumonía adquirida en la comunidad en ancianos, de ahí la importancia de conocer la prevalencia de colonización nasofaríngea y los serotipos de Sp.
MétodosDe diciembre de 2009 a junio de 2010 se realizaron cultivos nasofaríngeos en mayores de 50 años de comunidades rurales de México para la detección y serotipificación de Sp (reacción de Quellung). Se determinó la sensibilidad a penicilina y ceftriaxona mediante la técnica de microdilución.
ResultadosSe incluyeron 236 sujetos. La prevalencia de colonización por Sp fue del 21,6%. Los serotipos más frecuentes fueron 19A (21%), 6A (13%), 6B y 11A (11%). El 100% eran sensibles a ceftriaxona y en el 52,8% la concentración mínima inhibitoria de penicilina fue ≥0,12mg/l.
ConclusiónEste es el primer estudio de colonización nasofaríngea por Sp en adultos realizado en México. Se identificaron con frecuencia serotipos circulantes no incluidos en ninguna de las vacunas neumocócicas.
Airway mucosa is colonized by various bacteria through host dependent mechanisms and microorganisms present in a certain moment.1 Colonization by Streptococcus pneumoniae is usually associated with a specific number of serotypes which commonly cause invasive and localized infections.2
S. pneumoniae is considered the main pathogen affecting pediatric patients, young children and adults; it might be manifested as invasive pneumococcal disease (IPD), and is associated with high morbidity and mortality rates in adults older than 65 years and subjects with underlying diseases, which increases substantially with age.3
Epidemiological studies have shown that one of the major risk factors for colonization in adults is the coexistence with children of less than 5 years old4; it has already been observed that this tendency decreases with polysaccharide conjugate vaccine (PCV) administration, by herd effect.
Currently in Mexico, two available pneumococcal vaccines exist for adults; the polysaccharide vaccine of 23 serotypes (PPV23) and the conjugate vaccine of 13 serotypes (PCV13).5
In Mexico, PPV23 was included in the vaccination scheme in 1993, targeting population with risk factors: 60 to 64 years old as well as 65 or older. However, PPV23 does not impact on nasopharyngeal colonization, an important factor in the epidemiology of pneumococcal infections; thus, it does not confer significant protection against these mucosa infections or against a decrease of pneumococcal antimicrobial resistant strains.
At the moment of the present study only PCV7 and PPV23 existed. There are few data available on S. pneumoniae serotypes that cause IPD in Mexican population. From 2014 to 2017, the Dirección General de Epidemiología has reported an annual average of approximately 40 IPD cases.6
In addition, adult populations are not as studied as pediatric ones, although it is important to understand that PCV introduction impacts in adults, specially in the high-risk age group of 65 years and older.3 So, it is noteworthy to know the prevalence of nasopharyngeal colonization as a surrogate indicator of S. pneumoniae serotypes in adults in Mexican rural communities as well as the resistance to penicillin in these strains, in order to implement preventive programs that could impact the burden of disease in these groups.
MethodsCross sectional epidemiological, descriptive study; carried out from December 2009 to June 2010 in rural communities of Tequisquiapan, Amealco and Colon in Queretaro, México, an area with 1,840,000 inhabitants and 18 municipalities. Data recorded were: active and passive smoking, previous respiratory infection, use of antibiotics 1–3 months prior to the sample collection, cohabitation with children less than 5 years old and previous immunization within the last 5 years, with the 23-valent polysaccharide vaccine. Ethics committees of participating institutions approved the study; all participants signed an informed consent. A nasopharyngeal specimen was obtained from each participant; S. pneumoniae was identified by standardized microbiological methods.7 The serotyping was conducted using the Quellung reaction with serum produced by the Statens Serum Institute (Copenhagen, Denmark); the serogroup and serotype were identified according to Danish nomenclature.8
Penicillin and ceftriaxone susceptibility tests were performed by the microdilution method following the Clinical and Laboratory Standards Institute procedures.9 Isolates with penicillin minimal inhibitory concentrations (MICs) of ≤0.06mg/L, 0.12–1mg/L, and ≥2mg/L were considered susceptible, intermediate, and resistant, respectively. For the purpose of this study strains with intermediate susceptibility to penicillin were clustered into the resistant strains.
Statistical analysisStatistical analysis was performed with the SPSS 16.0 software. Data were reported with measures of central tendency and dispersion. An association between S. pneumoniae colonization and nominal variables of interest by means of Xi-squared or Fisher's exact test was considered as more convenient, the odds ratio and its 95% confidence interval were calculated.
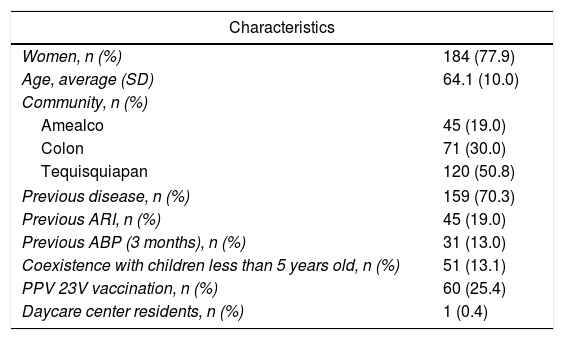
ResultsTwo hundred and thirty-six adults over 50 years old were included: 184 (77.9%) were women and 159 (67.4%) subjects had comorbidities, their general characteristics are shown in Table 1.
General characteristics of 236 subjects over 50 years in a Mexican rural community in Querétaro, México (2009–2010).
| Characteristics | |
|---|---|
| Women, n (%) | 184 (77.9) |
| Age, average (SD) | 64.1 (10.0) |
| Community, n (%) | |
| Amealco | 45 (19.0) |
| Colon | 71 (30.0) |
| Tequisquiapan | 120 (50.8) |
| Previous disease, n (%) | 159 (70.3) |
| Previous ARI, n (%) | 45 (19.0) |
| Previous ABP (3 months), n (%) | 31 (13.0) |
| Coexistence with children less than 5 years old, n (%) | 51 (13.1) |
| PPV 23V vaccination, n (%) | 60 (25.4) |
| Daycare center residents, n (%) | 1 (0.4) |
ARI: acute respiratory tract infection; ABP: antibiotic prescription; PPV 23V: polysaccharide pneumococcal vaccine of 23 serotypes.
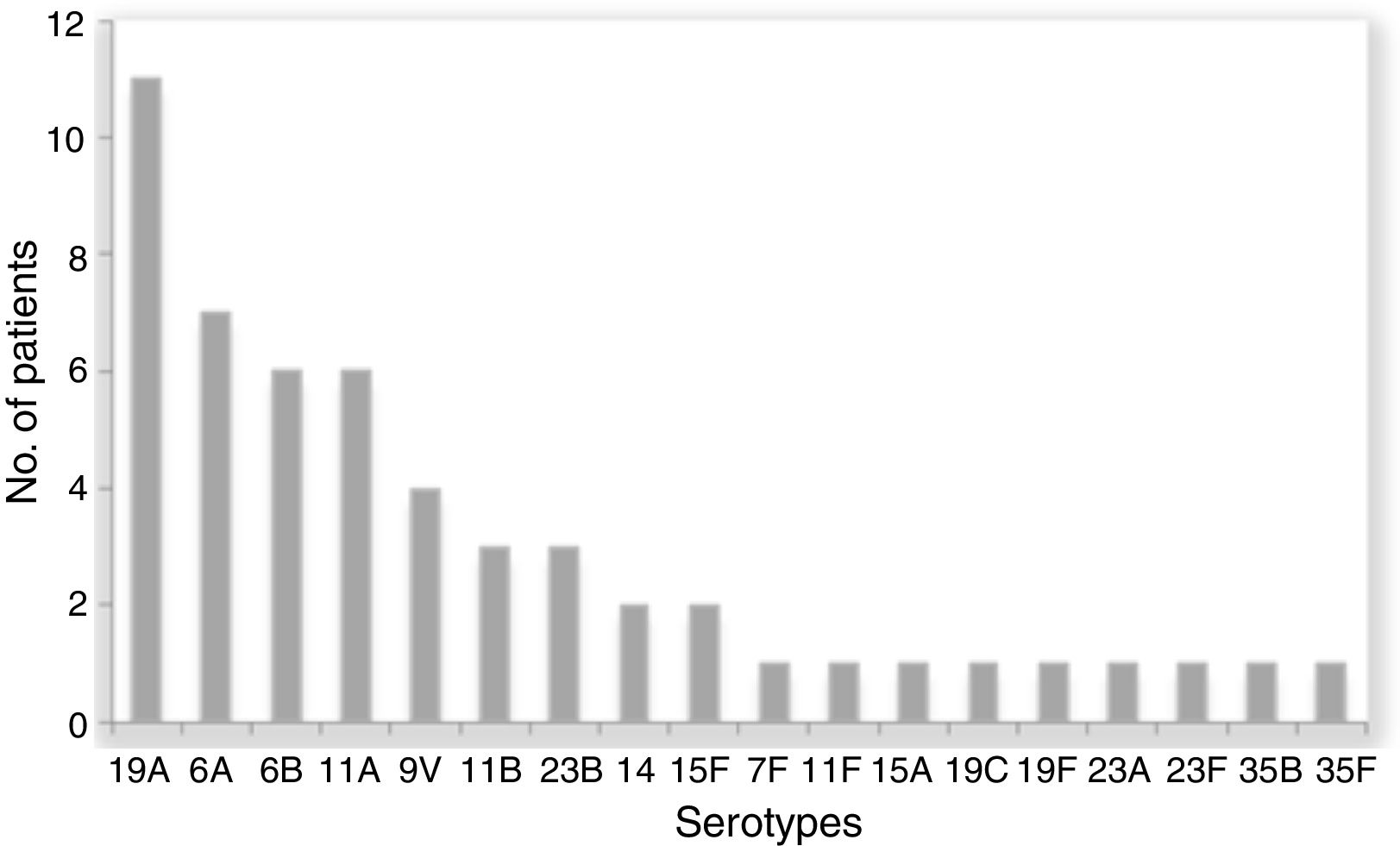
The prevalence of colonization by S. pneumoniae in the studied population was 21.6% (51/236) 95% CI 16.35–26.85. Two subjects were colonized by two different serotypes and we recovered a total 53 S. pneumoniae isolates. The most frequent serotypes were 19A (11), 6A (7), 6B (6) and 11A (6). The distribution of serotypes is shown in Fig. 1.
Twenty-five percent (13/53) of the serotypes were included in the PCV7, 26% (14/53) in the PCV1O, 62% (33/53) in the PCV13, and 60% (32/53) in the PPV23.
Penicillin resistance (intermediate plus resistant isolates) was detected in 52.8% (28/53). All isolates were susceptible to ceftriaxone.
There was no association between any of the variables studied with S. pneumoniae colonization or with penicillin-resistant isolates.
DiscussionThe studied population was mestizo from rural environment, living in communities with few day care centers for adults. It should be noted that only 13.5% (32/236) of the subjects had contact with children less than 5 years.
Despite of the absence of risk factors for S. pneumoniae carriage in our population, 21.6% (51/236) of adults with nasopharyngeal colonization represents a prevalence among the highest described in the world3 and indirectly shows the S. pneumoniae serotypes that circulate in the community.
Previous reports have indicated a prevalence between 3.7% and 38%,10–13 with differences attributed to ethnic, geographical and social development situations. The lowest prevalence has been found in the Jewish population in Israel and the highest in Australian aborigines, who have been described with a higher risk of colonization and invasive pneumococcal disease. In addition, a study performed in Nigeria shows a 26% prevalence of nasopharyngeal colonization prior to the introduction of PCV7.12
In Mexico, it is not mandatory to report cases of S. pneumoniae invasive disease, so, nowadays its incidence is unknown in all age groups. Since 2009, Mexico adopted a vaccination scheme of 3 doses of PCV7 in children less than one year old, however, in 2011 it was replaced with the PCV13.6
In previous reports from other municipalities, the proportion of PCV7 vaccination with 3 doses was approximately 60%,14 and as expected, circulating serotypes were not included in the vaccine. This possibility was confirmed with our results, finding that serotype 19A showed the highest prevalence, also reported by Carnalla-Barajas et al.15 as the main IPD agent in the USA. The proportion of 19A serotype, isolated from invasive and non-invasive pneumococcal disease in Mexican population, has increased with time.
In regard to bacterial resistance, Mexico has recently applied a policy on antibiotic selling restriction that started prior to the recruitment of our research subjects. The rate of bacterial resistance was similar to that found in strains colonizing the nasopharynx of young children immunized with PCV7 in rural communities.16 However, in a previous study in daycare centers, a higher rate of resistance to penicillin was found (64%).17
In the present study, we did not found antimicrobial resistance associated factors, and there were no ceftriaxone resistant strains, possibly because at rural communities in Mexico the use of third generation cephalosporins at outpatient level is still limited.
To our knowledge, this is the first study that analyzes the nasopharyngeal colonization by S. pneumoniae in adults in Mexico (21.6%). At the time of the study, there was approximately a 60% vaccination rate (PCV7) in the pediatric population and 25% of the identified serotypes are present in the PCV7. Children are the main reservoirs for the transmission of pneumococcal serotypes responsible of invasive disease in adults, but epidemiological changes observed among them should not only be attributed to the use of PCV7 or PCV13 among children, since other factors might also play an important role, for example, PPV23 vaccination in adults. However, it is unknown whether this herd effect will be similar across all serotypes and subgroups in the population. These effects might differ in populations with different serotype distributions and with higher or lower prevalence of chronic diseases among older adults. In order to choose the best prevention option, it is important to know exactly the serotypes that colonize the adult population, as well as the serotypes causing invasive and noninvasive diseases in our country.
There are several limitations in this study, it was performed during winter, thus, it was not possible to assess the seasonal variation in the colonization rate, and we did not performed molecular analysis. An analysis of a larger sample size and molecular analysis will improve our knowledge of invasive pneumococcal disease in our population.
FundingThis study was funded by the Hospital General Dr Manuel Gea Gonzalez, Ciudad de México, México.
Conflict of interestsThe authors declare no conflict of interests.
The authors thank Dr. Martha Mónica Alvarado Gallegos, from the Sanitary Jurisdiction II of San Juan del Río Querétaro, Mexico for her valuable cooperation in the realization of his work and Maricruz Juárez Brito, Epidemiology and Research, “Hospital para el Niño Poblano”, Mexico for her valuable suggestions to the manuscript.