Little is known about recurrent tuberculosis (TB) among HIV-infected patients and the influence of highly active antiretroviral therapy (HAART).
MethodsA population-based retrospective longitudinal study was conducted on all HIV-infected TB patients in Barcelona (Spain) notified in 1987–2003, and followed up until 2005. TB recurrence and HAART influence were analysed according to calendar period.
ResultsPatients with no-treatment and those in pre-HAART had more risk of TB recurrence (RR: 2.3; CI: 1–5.8 and RR: 4.8; CI: 2–12).
ConclusionsHAART decreases probability of TB recurrence and should be extended to all cases.
Se conoce poco sobre recurrencias en tuberculosis (TB) en pacientes infectados por VIH y la influencia del tratamiento antiretroviral de gran actividad (HAART).
MétodosEstudio poblacional longitudinal retrospectivo de todos los pacientes con TB infectados por VIH en Barcelona (España) notificados entre 1987-2003 y seguidos hasta 2005. Se analizó la influencia del HAART sobre las recurrencias en TB según el periodo calendario.
ResultadosLos pacientes sin antiretrovirales los del periodo pre-HAART tuvieron más riesgo de recurrencia en TB (RR:2.3;CI:1-5.8 y RR:4.8;CI:2-12).
ConclusionesEl HAART disminuye la probabilidad de recurrencia en TB por lo que debería extenderse su uso a nivel global.
The morbidity and mortality of patients co-infected with tuberculosis (TB) and HIV have been improved in the recent years due to the introduction of highly active antiretroviral therapy (HAART) in many settings. In Spain HAART is free and was extended to all population since 1997.1–3 Different studies have shown that being HIV-infected is a risk factor associated with TB recurrence and relapse.4–7 It is suggested that patients under HAART have a lower risk of TB recurrence.5–7 However, the impact on TB recurrence and the role of treatment in different eras (HAART, pre-HAART and the period without antiretrovirals) from a population based longitudinal study perspective is still not well known. Therefore, the objective of this study was to measure the incidence of TB recurrence, and analyse the influence of HAART in Barcelona city among all TB and HIV-infected cases during the period 1987–2005.
MethodsA population based retrospective longitudinal cohort study was performed in Barcelona (Spain). All HIV-infected TB patients notified to Barcelona TB Prevention and Control Program (TBPCP) who had initiated treatment between 1987 and 2003 were included. The TBPCP involves a high coverage and active epidemiologic surveillance of TB cases. All patients were residents of Barcelona (population according to the 1996 census was 1,508,805 inhabitants). The follow-up period lasted until December 31st, 2005.
Demographic and clinical data were obtained from the epidemiological questionnaire used by TBPCP.3 Recurrence was defined as a new clinical and/or microbiological diagnosis of TB in any patient who had correctly completed treatment for their first episode, and who had been free of the disease for at least one year, otherwise they were considered a relapse of the same episode. Because HAART is free and extended to all population in Spain since 1997, we formed three groups according to the year of TB diagnosis and assuming from a populational perspective that all patients were under the recommended antiretroviral treatment according to the HAART calendar period or era: HAART group of patients, patients diagnosed since 1997; pre-HAART group, patients diagnosed from 1993 to 1996; and patients without antiretroviral treatment (NoART), all of whom TB diagnostic was until 1992. Other analysed variables were age and sex.
In the data collection and checking process, information from the TB and AIDS registers of the city was compared. Since most of the people who move usually go to other areas of Catalonia, the TB register, and the Mortality Register of Catalonia served to check for possible recurrence events among patients who had moved away from Barcelona during the follow-up period.
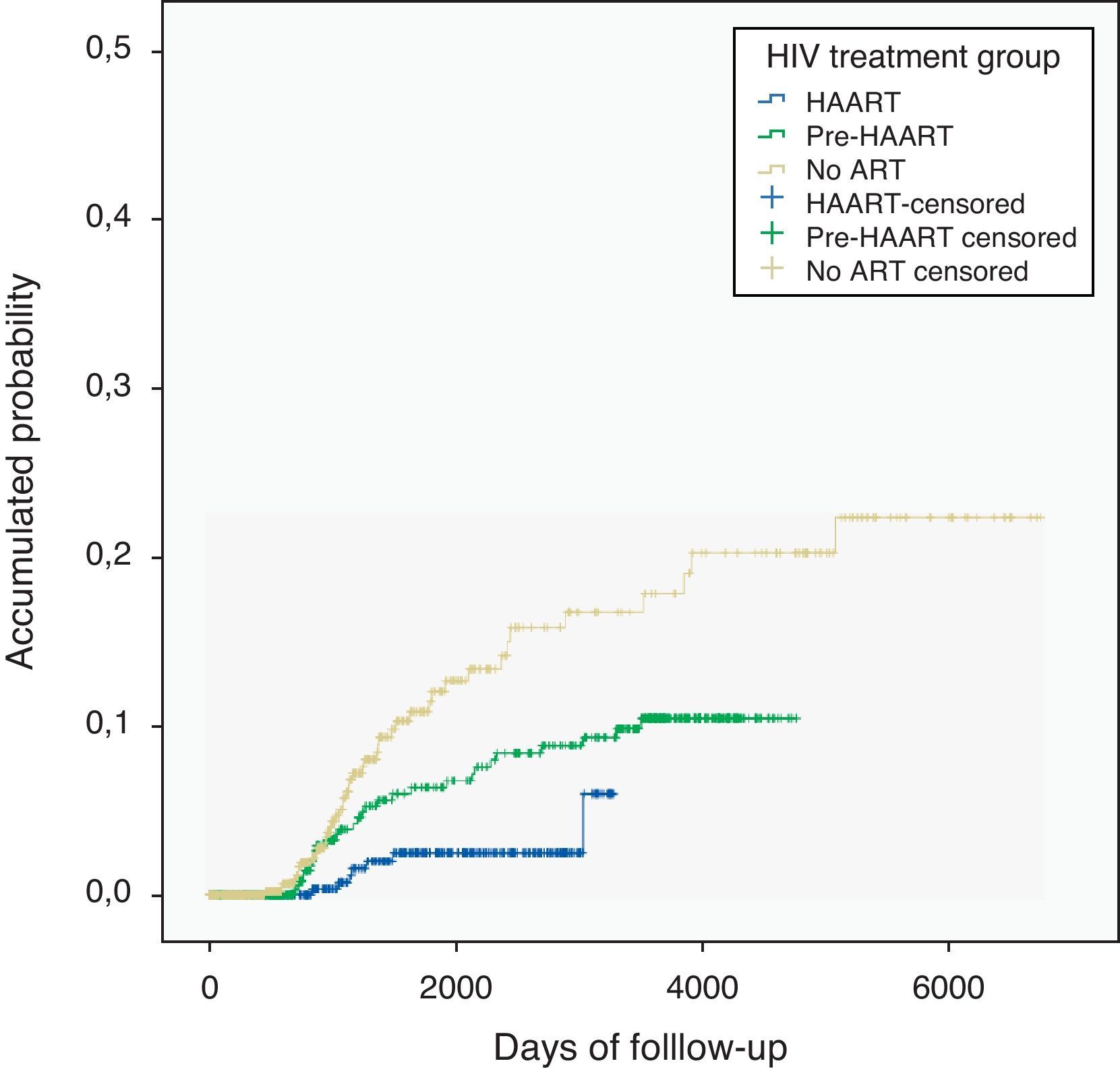
A descriptive analysis of the variables was performed. Quantitative variables were described using medians and ranges. The duration of follow-up was calculated as the interval from the date when TB treatment was initiated until recurrence, death, moved away (transferred), or the end of the study. In calculating density of recurrence incidence, the denominator was person-years (PY) of follow-up. We calculated the Incidence and Relative Risk (RR) with a confidence interval (CI) of 95% and estimated the probability of recurrence among the three groups with Kaplan–Meier (KM) method to construct survival curves at univariate level, with differences between curves assessed with the Log-rank test, considering a p-value<0.05 as statistically significant.
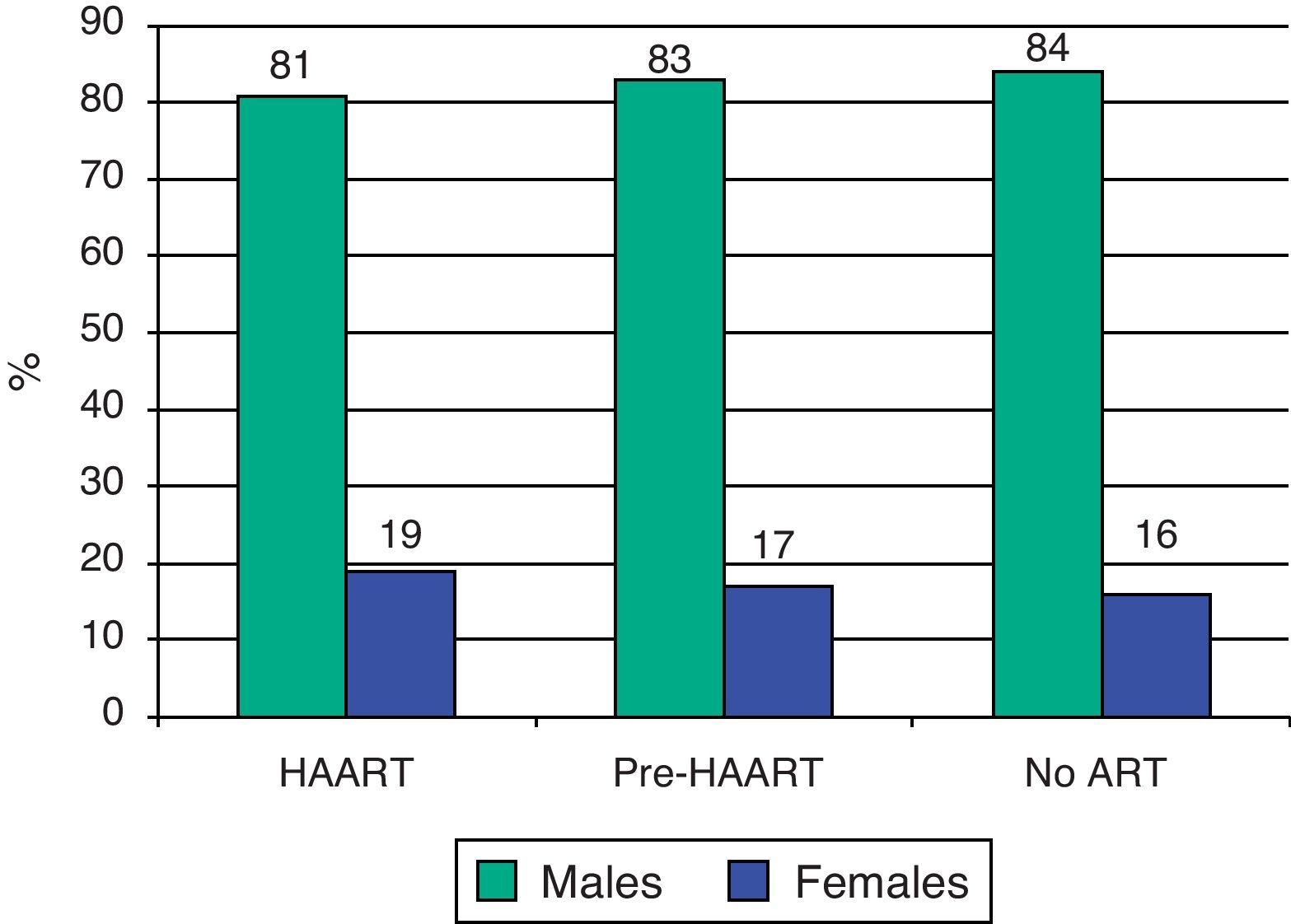
ResultsA total of 1865 patients were analysed during the study period, 444 (23.8%) in the HAART group, 665 (35.7%) in the pre-HAART group, and 756 (40.5%) patients in the noART group. The median age (Range) of the HAART group was 36 (19–88) years, and 32 (19–72) years for the pre-HAART group (p=0.04). The median age in the NoART group was 30 (16–70) years with no statistically significant differences with the pre-HAART group (p=0.09). Males were more frequent in all groups, at 81, 83 and 84%, respectively (Fig. 1).
Among 61 recurrences, incidence was 0.39 events per 100-person year (PY) of follow-up with HAART, 0.92 PY with pre-HAART and 1.9 PY with NoART group. The pre-HAART group had two times more risk of TB recurrence than the HAART group (RR: 2.3; CI 1–5.8) and NoART almost five times compared to the HAART group (RR: 4.8; CI 2–12). Differences in KM curves were observed between the three groups (p value<0.001) (Fig. 2).
DiscussionThis study shows that HIV-infected patients under HAART have a lower risk of TB recurrence compared to patients under antiretroviral mono or biotherapy, and patients with no antiretroviral treatment. Moreover, patients with noART had five times more risk for TB recurrence compared to patients under HAART. TB recurrence in the HAART group (0.39 PY) was similar to recurrence found in the general population in Barcelona during the period 1995–2005 (0.53 PY).8 Differences in age among groups could be explained by the high mortality in the pre-HAART period and the increased survival after the extension of HAART treatment.9 Regarding sex, males were more frequent in all groups probably due to the influence of main route of HIV-infection (male who had sex with male and injecting drug use practice are preferently used among males).8–10
This high TB recurrence rate among HIV-infected patients without HAART is still higher in high burden TB countries such are those in the sub-Saharian Africa. Our high recurrence rate could still be much higher if the survival of these patients would be better.10–13 That HIV-infection is a risk factor for TB recurrence was already described in high TB and low TB incidence settings such as South Africa, United States, England, Wales or Spain among others.4,10,14 However, little studies have assessed the implication of antiretroviral treatment on TB recurrence from a populational-based perspective in low and middle burden TB countries. In countries with high incidence of TB, recurrence rate is elevated, being reinfection the main cause, especially when HIV prevalence is high. In a low TB burden incidence settings (less than 20 cases per 100,000 population), recurrence is low and mostly due to endogenous reactivation, even if patient was considered cured.2–5,15 A limitation of the study was that we could not analyse the effect of some confounders such as CD4 cell count, transmission category or differences in follow-up period.
TB recurrence is an important problem for TB control and well related to the HIV status. Besides to intensification of TB case finding and proper case and contact latent TB infection treatment, the TB burden could be decreased with the HAART extension worldwide, but especially in countries with high TB incidence and HIV-infection prevalence.
Conflict of interestThe authors have no conflict of interest to declare.