A Ukrainian woman of 35 years, with no relevant medical history, consulted for a skin lesion, located in the pubis, of one and a half months of evolution, treated with oral and topical antibiotics, and topical antifungals, without having obtained any improvement. The skin lesion was very painful, especially when walking. The patient had no fever or systemic symptoms. No other skin lesions were observed in the clinical examination. The patient worked in a chicken farm.
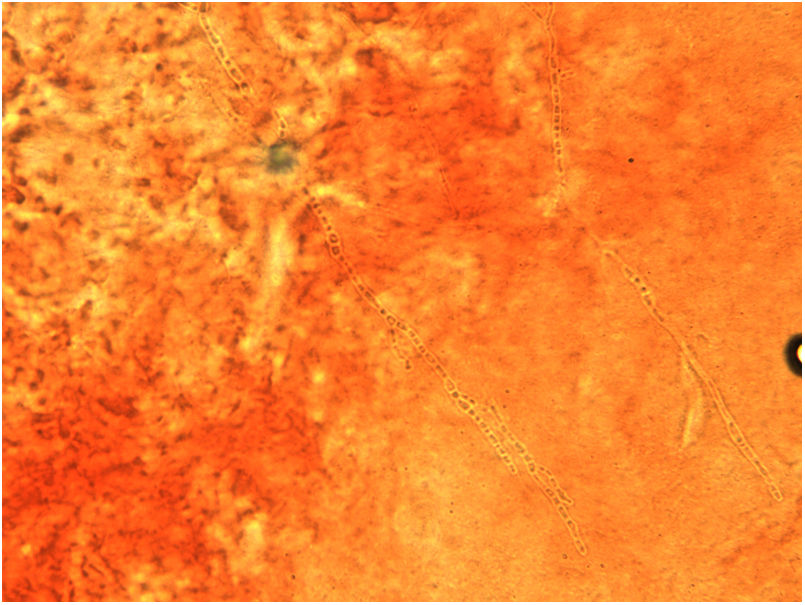
Physical examination revealed an erythemato-edematous plaque on the pubis and the inguinal region, with follicular and non-follicular pustules, yellowish crusts and edema of the labia majora (Fig. 1). No adenopathies were detected on palpation. There were no alterations in the blood count, biochemistry or coagulation. The serology of HIV was negative.
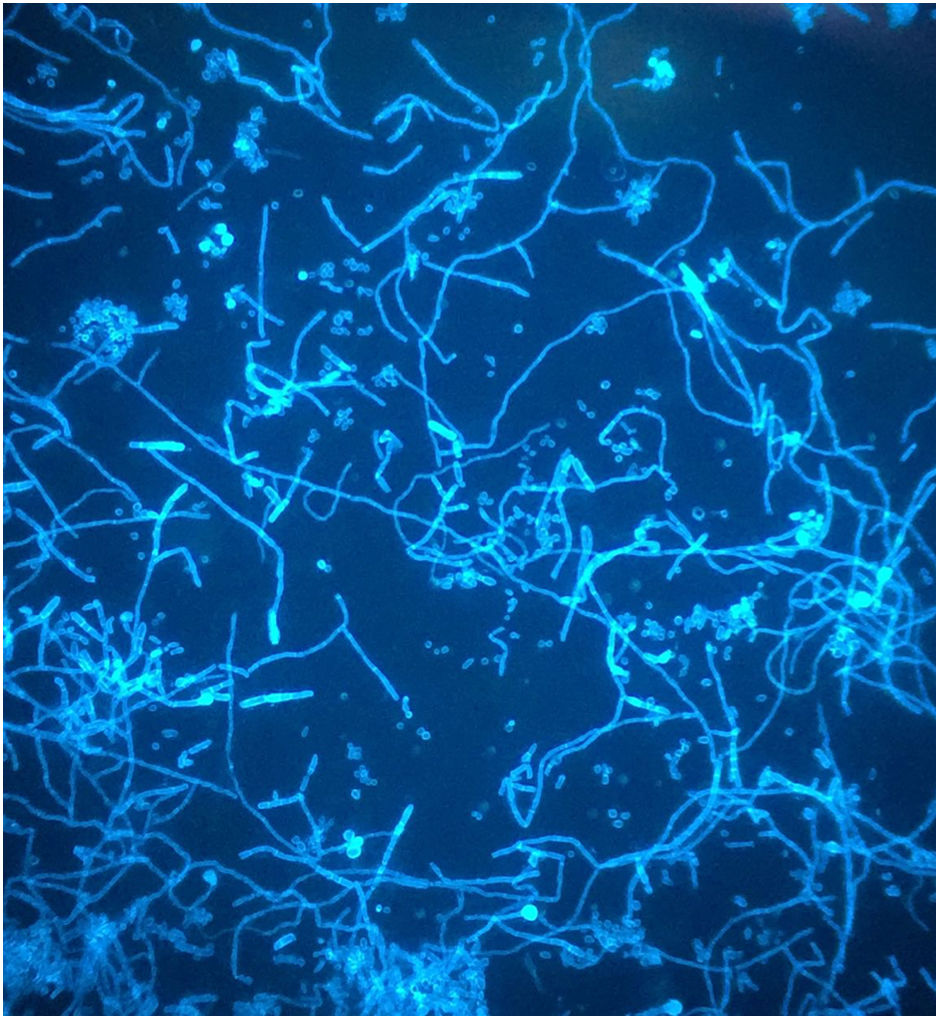
A dermatophytosis was suspected, and a scraping of the lesion was performed to carry out a microbiological culture, as well as direct examination with 40% potassium hydroxide, which allowed the visualization of fungal structures (Fig. 2). After 5 days of incubation at 30°C on Sabouraud agar, the growth of a filamentous fungus with a powdery texture and a high central button was observed. It had irregular edges, cream white colored on the surface, with an ocher reverse and a yellowish pigment that diffused to the medium. Microscopic examination of the colony revealed hyaline, septate hyphae, some of them spirally branched conidiophores, bearing numerous spherical conidia arranged in grape-like clusters (Fig. 3). The macro and microscopic identification of the fungus was completed with the urea hydrolysis test, which was positive at 3 days, identifying the fungus as Trichophyton mentagrophytes complex.
Majocchi granuloma (MG) was diagnosed. Treatment was started with oral fluconazole of 100mg/day and topical terbinafine for 8 weeks, achieving resolution of the lesions without alopecia or residual scars.
Final commentMajocchi described the “trichophytic granuloma” in 1883 as an intracutaneous or subcutaneous granulomatous inflammation resulting from the invasion of Trichophyton tonsurans.1
Two forms of MG have been defined. A follicular form due to the occlusion of the follicle after a previous cutaneous trauma, which causes the passive transfer of the dermatophyte to the dermis together with keratin or necrotic material. It usually occurs in immunocompetent patients, more frequently in women after shaving her legs. In this form, hair infection is endothrix and granuloma formation is favored by the use of corticosteroids.2 The subcutaneous form is typical of immunocompromised patients, and it is characterized by the appearance of subcutaneous nodules on the scalp, face or forearms.3
Deep pubic dermatophytosis is very rare.2,4,5 Frequently, the direct examination of the scraping of the lesion is negative because the dermatophyte is found in the deeper layers of the stratum corneum. Therefore, in case of suspicion, it is important to carry out a culture, and in case of doubt, a biopsy.3 The differential diagnosis should be made with cellulitis of bacterial or fungal origin, eosinophilic cellulitis, bacterial folliculitis, actinomycosis, and hidradenitis suppurativa.2–5
The pathogenic species that most frequently cause MG are Trichophyton rubrum, T. mentagrophytes, Trichophyton violaceum and Epidermophyton floccosum.6
T. mentagrophytes complex7 is an anthropophilic and zoophilic dermatophyte fungus of worldwide distribution that affects the human species and a wide variety of animals. Transmission of the pathogen can occur through contact with other people or infected animals, autoinoculation or through the soil.8 When human beings are infected by this type of fungus, especially when it is due to zoophilic dermatophytes, a great immune response occurs, with formation of microabscesses and pustules,9 which could explain the severe inflammation in our patient.
MG treatment should include systemic antifungals. Topical antifungals in monotherapy are ineffective, as occurred initially in our patient, due to their inability to penetrate through the dermis. The best result is obtained with the combination of topical and systemic antifungals.2–5
Deep dermatophyte infections can spread, affecting both the lymph nodes and other organs, such as the liver or brain, so they can become lethal.6
AuthorshipAll authors had access to the data and played a role in writing this manuscript.
Conflict of interestsThe authors declare that they have no conflicts of interest.
The authors thank Javier Pemán for his assessment.