A 60-year-old man presented with a one-month history of a mildly pruritic growing plaque on his left leg. Pertinent history included diffuse large B-cell lymphoma. The patient had received six cycles of bendamustine–rituximab therapy, which had ended 10 months prior, and was currently under rituximab maintenance therapy. The patient had developed severe lymphopenia (0.2×103/μL lymphocytes, normal range: 1–3×103/μL) and hypogammaglobulinemia (low Ig G: 376mg/dL, normal range: 767–1590mg/dL; low Ig A: 38mg/dL, normal range: 90–450mg/dL; and low Ig M: 8mg/dL, normal range: 70–280mg/dL).
The patient recalled a minor trauma with a chair in his house and denied visiting non-urban areas in the previous three months. Moreover, he denied contact with animals or plants, and he had not been in contact with other people with similar skin lesions. Physical examination revealed a non-tender violaceous crusted plaque on the posterolateral aspect of his left leg (Fig. 1). The patient did not have other cutaneous lesions, fever, or any other systemic symptoms.
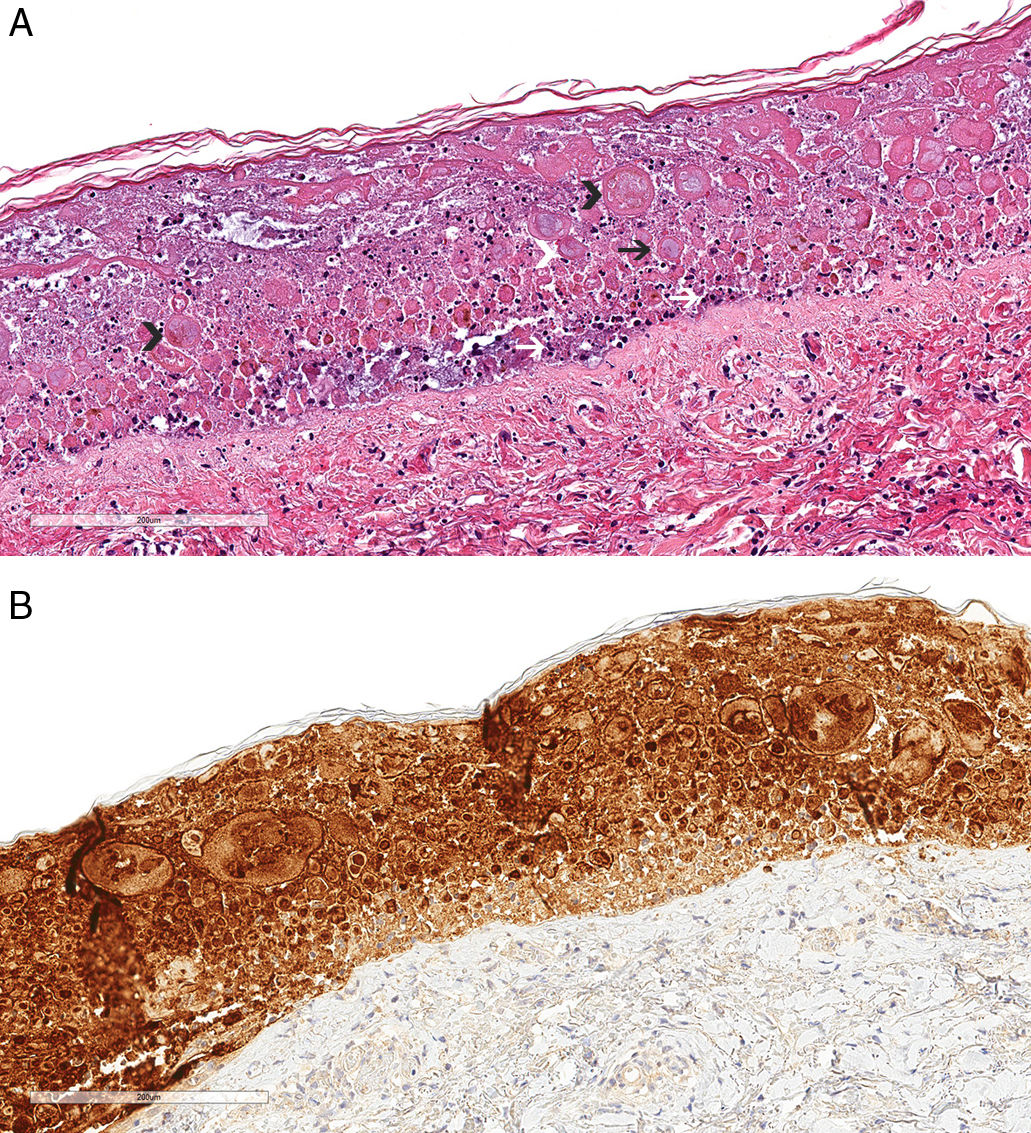
Diagnosis and evolutionAn initial suspicion of an opportunistic infection was proposed. Consequently, a skin biopsy was performed for histopathological study and culture of bacteria, mycobacteria, and fungi. The pathological examination revealed a widely necrotic epidermis with multinucleated acantholytic keratinocytes, nuclear molding, and ballooning (Fig. 2A). Epidermal cells exhibited positive immunohistochemistry staining for type 1 Herpes simplex virus (HSV-1) (Fig. 2B). Staining for fungi and mycobacteria, as well as cultures, were negative. The patient was treated with 1g of oral valacyclovir twice daily during three weeks. At follow up, one month after initiating treatment, the patient had achieved complete healing (Fig. 3).
Histopathologic study revealed a widely necrotic epidermis with multinucleated acantholytic keratinocytes (black arrowhead), steel-gray nuclei (black arrow), nuclear molding (white arrowhead), and nuclear dust (white arrow) (hematoxylin and eosin, 20×) (A). Immunohistochemical study showed positive staining for type 1 Herpes simplex virus (20×) (B).
Abnormal function of the immune system creates an increased susceptibility to infections by common and atypical pathogens. The interactions between HSV-1 and the immune response are complex. In fact, even though innate immunity is needed to suppress HSV-1, specific CD8-positive and CD4-positive T cells are essential to inhibit viral infection and prevent HSV-1 reactivation.1
Our patient had initially received six cycles of bendamustine and rituximab for treatment of diffuse large B-cell lymphoma. After that, the patient had continued with rituximab maintenance therapy. Bendamustine, a nitrogen mustard, can result in lymphopenia, especially a reduced number of CD4-positive cells.2 Rituximab targets CD20 antigen on B lymphocytes and has a cytotoxic effect, causing their depletion. However, B-cell depletion has also been found to impair the survival of CD4 memory T cells.2 This has been confirmed by a study that found prolonged CD4 and CD8 lymphopenia during rituximab maintenance therapy after bendamustine–rituximab therapy in patients with B-cell malignancies.2 Severe impairment of adaptive immunity, including both T- and B-cell depletion, has affected our patient's response to viral infections.
Cutaneous herpesvirus infection commonly presents as painful vesicles, preceded by paresthesia at the site of inoculation. Nevertheless, immunocompromised patients might develop unusual clinical presentations.3 Furthermore, these patients can present with infections resistant to usual antivirals.3 Histopathological study characteristically shows epidermal necrosis and viral cytopathic changes with ballooning degeneration.3 Immunohistochemical study can detect viral antigens and identify the type of virus.
Immunosuppression in patients with an underlying hematologic or solid organ malignancy, or due to their treatment, results in a high susceptibility to heterogeneous skin infections. Although HSV-1 infection is typically considered based on clinical history and examination, immunocompromised patients, especially those with cellular immunity impairment, might develop atypical chronic presentations, as in our case. Consequently, it is important to consider herpetic infections in the differential diagnosis to provide adequate and prompt treatment.
FundingThis article has no funding source.
Authors’ contributionsAll authors had access to the data and contributed to writing this manuscript.
We confirm that this manuscript contains original, unpublished work that is not being considered for publication elsewhere at the same time.
Informed consentThe patient in this manuscript provided written informed consent for publication of his case details.
Conflicts of interestNone of the authors have any conflicts of interest to declare.