This study aimed to evaluate trends and clinical characteristics of Mycobacterium bovis human tuberculosis cases, describe the epidemiological features, and compare risk factors associated with extrapulmonary and pulmonary tuberculosis.
MethodsA retrospective cohort analysis was conducted on M. bovis infection cases confirmed by culture from seven clinical microbiology laboratories in Madrid, Spain, from 2010 to 2022. Sociodemographic and clinical data were extracted from the hospital database. Tuberculosis (TB) cases were classified as extrapulmonary (EPTB) and pulmonary tuberculosis (PTB), with disseminated TB cases excluded from statistical analysis.
ResultsAmong 3670 patients with Mycobacterium tuberculosis complex infection, M. bovis was identified in 66 patients, representing 1.8% of the total. PTB and EPTB were identified in 45.5% and 39.4% of cases, respectively, with 15.1% having disseminated TB. PTB was significantly associated with males and Spanish nationality, while EPTB was more prevalent among females and those with a rural lifestyle.
ConclusionsThe study revealed an escalating trend in M. bovis tuberculosis cases. Middle-aged patients, including a substantial immigrant population, were predominantly affected. Female gender and a rural lifestyle were associated to extrapulmonary disease.
Este estudio tiene como objetivo evaluar las tendencias y las características clínicas de los casos de tuberculosis humana por Mycobacterium bovis, describir las características epidemiológicas y comparar los factores de riesgo asociados a la tuberculosis extrapulmonar y pulmonar.
MétodosSe realizó un análisis de cohortes retrospectivo de los casos de infección por M. bovis, confirmados por cultivo, procedentes de 7 laboratorios de microbiología clínica de Madrid, España, entre 2010 y 2022. Los datos sociodemográficos y clínicos se extrajeron de la base de datos hospitalaria. Los casos de tuberculosis (TB) se clasificaron como tuberculosis extrapulmonar (TBEP) y tuberculosis pulmonar (TBP), excluyéndose del análisis estadístico los casos de tuberculosis diseminada.
ResultadosDe los 3.670 pacientes con una infección por Mycobacterium tuberculosis complex, se identificó M. bovis en 66 pacientes, lo que representa el 1,8% del total. Se identificaron TBP y TBEP en el 45,5 y el 39,4% de los casos, respectivamente, con un 15,1% de tuberculosis diseminada. La TBP se asoció significativamente con el sexo masculino y la nacionalidad española, mientras que la TBEP fue más prevalente entre las mujeres y las personas con un estilo de vida rural.
ConclusionesSe ha identificado una tendencia ascendente en los casos de tuberculosis causada por M. bovis. La mayoría de los pacientes afectados fueron de mediana edad, con una significativa representación de la población inmigrante. Observamos una asociación entre el sexo femenino y el estilo de vida rural con la manifestación extrapulmonar de la enfermedad.
Mycobacterium tuberculosis complex (MTBC) is a group of organisms that includes pathogens like M. tuberculosis, Mycobacterium africanum and Mycobacterium bovis.1M. bovis is the classical causative agent of bovine tuberculosis (TB) but can also be responsible for TB in humans.2 In Spain, human TB cases caused by M. bovis constitute a small proportion of all TB cases, and the disease is mainly considered a zoonosis that affects largely cattle and secondarily other mammals, like humans.3 A high percentage of cases are related to occupational exposure, explained for direct contact with tuberculous animals. Other route of transmission is consumption of unpasteurized dairy products or improperly cooked meat and come from bovine TB-endemic countries.4,5
The disease produced by M. bovis is clinically and radiographically indistinguishable from the rest of members of MTBC and the symptoms include fever, weakness, and weight loss.1 However, distinguishing M. bovis from M. tuberculosis holds significant importance in patient management. Unlike other members of the MTBC, M. bovis inherently exhibits resistance to pyrazinamide. Beyond its utility for the specific identification of M. bovis, this natural resistance holds particular significance. Pyrazinamide is typically included in classical first-line TB treatment due to its effectiveness as a sterilizing drug, which aids in shortening TB therapy through synergistic effects with rifampicin. Consequently, in the case of a M. bovis infection, the inclusion of pyrazinamide in a patient's anti-TB regimen would be ineffective and adds only secondary effects.2,3
Even in high-income countries like Spain, human TB caused by M. bovis may be underestimated. This underestimation may be attributed to the widespread use of identification techniques that do not specifically differentiate M. bovis from other members of the MTBC. Additionally, susceptibility testing for pyrazinamide is not routinely conducted, contributing to the potential oversight of cases involving this pathogen.
The aim of this study is to evaluate the trends in human TB cases caused by M. bovis in our region from 2010 to 2022, to describe the clinical and epidemiological characteristics of cases of human TB caused by M. bovis, and to compare risk factors associated with extrapulmonary versus pulmonary disease.
Material and methodsWe conducted a retrospective cohort analysis of M. bovis infection cases confirmed by culture from seven clinical microbiology laboratories in Madrid, Spain, between 2010 and 2022, excluding patients with Bacillus Calmette-Guérin strains. Sociodemographic and clinical information for all cases were extracted from the hospital database.
The cases of TB were classified as either extrapulmonary or pulmonary TB. Patients with disseminated TB were excluded from our statistical analysis. We considered appropriate therapy for M. bovis infection when the standard regimen was extended to 9 months due to the ineffectiveness of pyrazinamide. For patients with drug-resistant M. bovis infections, we defined appropriate therapy as treatment guided by drug susceptibility testing.6
Associations between localization of TB and demographic, microbiological and clinical information were analyzed using Stata/BE 17.0. Categorical variables were expressed as number (%) and compared by Pearson's chi squared test or Fisher's exact test (if any value was <5). Results were considered significant when p-values were <0.05. Ethical approval was not required for the study due to its retrospective nature.
Samples were processed according to the standard procedures for each hospital, which include acid-fast staining and decontamination of the samples prior to inoculation onto liquid and/or solid medium. Liquid medium used included MGIT™ 960 tubes (Becton, Dickinson, USA) in 5 laboratories, BacT/Alert®bottles (bioMérieux, France) in 1 laboratory, or VersaTREK™ (Thermo Scientific, USA) bottles in 1 laboratory.
Positive cultures, identified as acid-fast bacilli (AFB) positive by microscopy, underwent further identification through an immunochromatographic test for the detection of the SD Bioline™ TB Ag MPT64 rapid kit (Abbott, USA). Drug susceptibility testing for streptomycin, isoniazid, rifampicin, ethambutol, and pyrazinamide was performed on all cultures identified as members of the MTBC according to the standard procedures. Strains exhibiting resistance to pyrazinamide were further identified to the species level through Genotype® MTBC assay (Hain Lifescience, Germany). The use of this assay enabled the precise differentiation between M. bovis subsp. bovis and M. bovis subsp. caprae, facilitating a more specific and effective diagnosis of infections caused by these subspecies. Molecular detection of MTBC was performed upon the physician's request, prompted by a high clinical suspicion of TB.
ResultsDuring the study period, a total of 371,846 clinical samples were processed for mycobacterial culture. Among these, 8700 isolates of the MTBC were identified, corresponding to 3670 patients. Out of these patients, 66 were specifically identified as having M. bovis, constituting 1.8%. All M. bovis isolates demonstrated monoresistance to pyrazinamide, but no other resistances against first-line antituberculous agents.
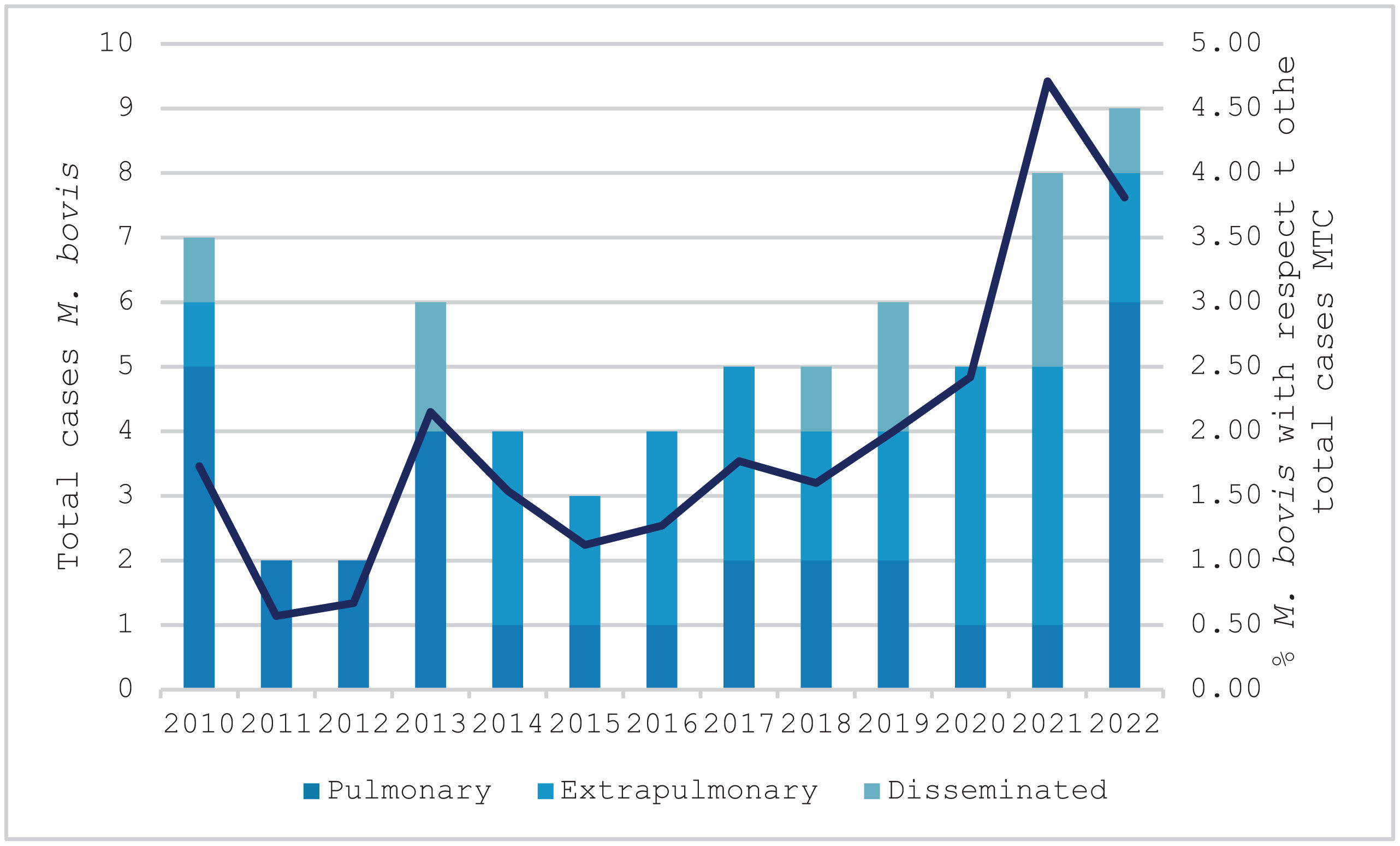
The trend of M. bovis cases over the course of the study is shown in Fig. 1, with the minimum recorded number of cases being 2 in 2011 and the maximum being 9 in 2022.
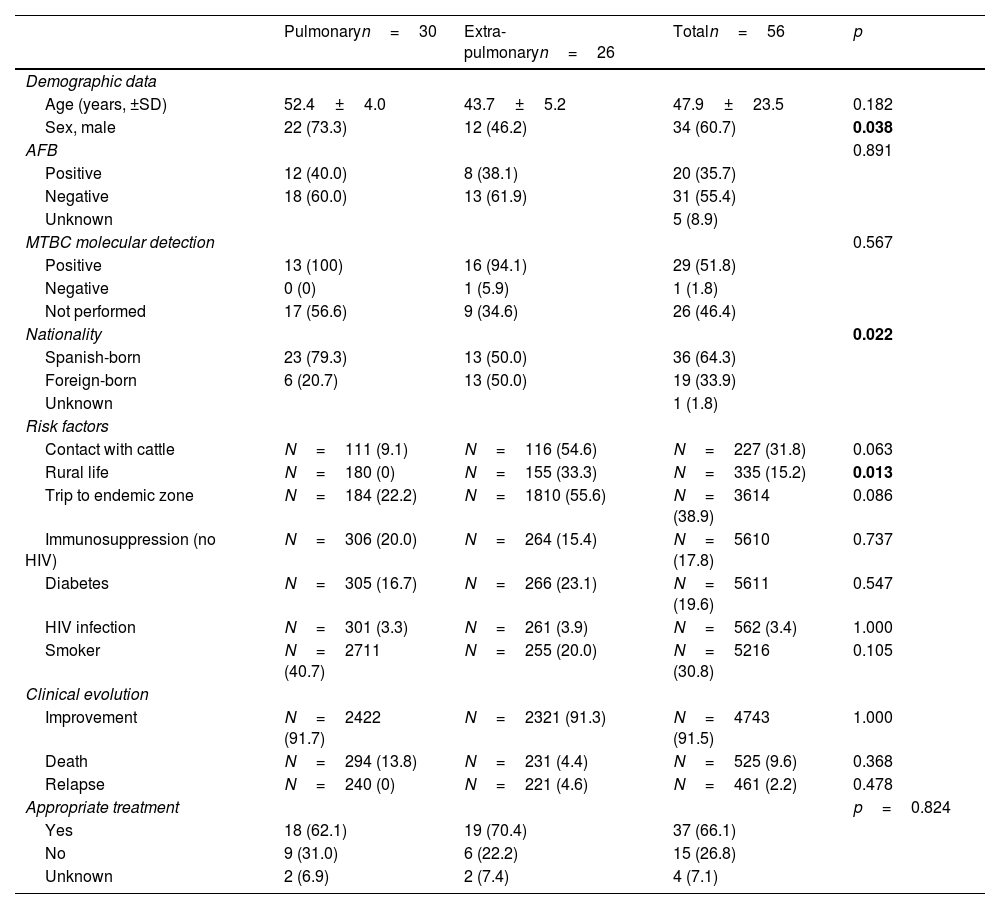
Data on risk of exposure to M. bovis were available in 50 (75.8%) of the 66 cases, with 26 (52%) registering a probable or possible risk of exposure and 24 (48%) registering no risk. Probable exposure mainly included occupational exposure, residing in a rural area, or having undertaken a trip to an endemic zone, and possible exposure included patients born in areas with a high prevalence of bovine TB, where reactivation may have occurred.3 Among the 66 patients with M. bovis, 30 (45.5%) developed pulmonary TB (PTB), 26 (39.4%) extrapulmonary TB (EPTB), and 10 (15.1%) disseminated TB. The epidemiological, microbiological, and clinical features of TB caused by M. bovis, stratified by location (PTB vs. EPTB), are presented in Table 1. PTB cases exhibited a statistically significant association with males and individuals of Spanish nationality. In contrast, EPTB was notably more prevalent among females and individuals with a rural lifestyle.
Characteristics of pulmonary and extrapulmonary tuberculosis caused by M. bovis.
| Pulmonaryn=30 | Extra-pulmonaryn=26 | Totaln=56 | p | |
|---|---|---|---|---|
| Demographic data | ||||
| Age (years, ±SD) | 52.4±4.0 | 43.7±5.2 | 47.9±23.5 | 0.182 |
| Sex, male | 22 (73.3) | 12 (46.2) | 34 (60.7) | 0.038 |
| AFB | 0.891 | |||
| Positive | 12 (40.0) | 8 (38.1) | 20 (35.7) | |
| Negative | 18 (60.0) | 13 (61.9) | 31 (55.4) | |
| Unknown | 5 (8.9) | |||
| MTBC molecular detection | 0.567 | |||
| Positive | 13 (100) | 16 (94.1) | 29 (51.8) | |
| Negative | 0 (0) | 1 (5.9) | 1 (1.8) | |
| Not performed | 17 (56.6) | 9 (34.6) | 26 (46.4) | |
| Nationality | 0.022 | |||
| Spanish-born | 23 (79.3) | 13 (50.0) | 36 (64.3) | |
| Foreign-born | 6 (20.7) | 13 (50.0) | 19 (33.9) | |
| Unknown | 1 (1.8) | |||
| Risk factors | ||||
| Contact with cattle | N=111 (9.1) | N=116 (54.6) | N=227 (31.8) | 0.063 |
| Rural life | N=180 (0) | N=155 (33.3) | N=335 (15.2) | 0.013 |
| Trip to endemic zone | N=184 (22.2) | N=1810 (55.6) | N=3614 (38.9) | 0.086 |
| Immunosuppression (no HIV) | N=306 (20.0) | N=264 (15.4) | N=5610 (17.8) | 0.737 |
| Diabetes | N=305 (16.7) | N=266 (23.1) | N=5611 (19.6) | 0.547 |
| HIV infection | N=301 (3.3) | N=261 (3.9) | N=562 (3.4) | 1.000 |
| Smoker | N=2711 (40.7) | N=255 (20.0) | N=5216 (30.8) | 0.105 |
| Clinical evolution | ||||
| Improvement | N=2422 (91.7) | N=2321 (91.3) | N=4743 (91.5) | 1.000 |
| Death | N=294 (13.8) | N=231 (4.4) | N=525 (9.6) | 0.368 |
| Relapse | N=240 (0) | N=221 (4.6) | N=461 (2.2) | 0.478 |
| Appropriate treatment | p=0.824 | |||
| Yes | 18 (62.1) | 19 (70.4) | 37 (66.1) | |
| No | 9 (31.0) | 6 (22.2) | 15 (26.8) | |
| Unknown | 2 (6.9) | 2 (7.4) | 4 (7.1) | |
Out of the 66 cases of bovine TB, 40 (60.6%) were Spanish nationality, 24 (36.4%) were foreign-born, and 2 (3.0%) cases had unknown nationality. Among patients with non-Spanish nationality, 13 (54.2%) were from Morocco, 3 (12.5%) from Peru, 2 (8.3%) from France, and one each from Colombia, Honduras, El Salvador, Mali, Equatorial Guinea, and China (4.2%, respectively).
Regarding the treatment received, 37 patients (66.1%) received appropriate treatment, of which 18 (62.1%) were from the PTB group and 19 (70.4%) from the EPTB group. The treatment adjustment time was obtained from 23 patients, with a mean of 47.6±20.0 days, and no statistically significant differences were found between the PTB and EPTB groups, respectively (46.1±22.3 vs. 48.9±18.6, p=0.744).
DiscussionThis study reveals a growing trend in the prevalence of M. bovis infections in the Autonomous Community of Madrid (a 7-million inhabitant area, mainly in urban zones) over time. We observed that M. bovis accounted for 1.8% of TB cases, a percentage consistent with findings reported previously in Spain (1.9% in 2004–2007)3 and in other industrialized countries such as the UK (1.5% in 2003).7
Traditionally, M. bovis has been linked to extrapulmonary disease. However, it remains uncertain whether this association is influenced by the mode of transmission, the immune condition of the host, or specific virulence traits exhibited by M. bovis.7–9 In our study, consistent with observations in other countries within our context, we found a slight prevalence of PTB over EPTB. As noted by other authors,10 this predominance of PTB may be attributed to the respiratory route becoming the primary mode of transmission, following the widespread adoption of milk pasteurization and the increased diagnostic challenges, leading to a decreased clinical suspicion until advanced stages of the disease.
In regions like ours, where bovine TB has been virtually eradicated, residual cases occur in elderly patients and are associated with the reactivation of a latent lesion. The mean age of patients in our study was not as high as one might expect, likely due to a significant percentage of migrant patients. We identified 17.8% of patients as immunocompromised ones. Cases involving elderly patients with immunosuppressive conditions may be associated with a reactivation of the infection.11
With respect to the nationality of patients, in comparison to other studies conducted in Spain,3 we observed a high percentage of M. bovis TB cases among foreign patients, accounting for 36.4% (24/66). This phenomenon may be attributed to the high immigration rate in the area where the study was conducted.
EPTB were more frequent in women, in accordance with other studies on TB caused by M. bovis.3,5 Additionally, our study found a higher likelihood of EPTB caused by M. bovis among individuals with a rural lifestyle, aligning with research investigating the epidemiology of EPTB cases.12
There is very limited evidence supporting the current recommendations for the treatment of human disease caused by M. bovis. According to the recommendations from the Centers for Disease Control and Prevention (CDC), the standard treatment for M. bovis infections typically includes rifampicin, isoniazid, and ethambutol. The duration of treatment is usually extended to 9 months due to the exclusion of pyrazinamide, as all M. bovis strains are resistant to this drug.6 In our study, 66% of the patients received an appropriate treatment regimen, with treatment adjustments occurring at an average of 47.6±20.0 days. A substantial proportion of participants (91.5%) showed positive clinical outcomes, with only one case of infection relapse. These favorable results, even in patients without an appropriate treatment duration, may be attributed to the fact that all M. bovis isolates were susceptible to first-line antituberculous drugs.
Our study has several limitations. The retrospective nature of the study hindered the exploration of critical variables dependent on the quality of the initial interview, including established risk factors for M. bovis infection, such as the consumption of unpasteurized dairy products and contact with cattle. Additionally, the population of our region may not precisely represent the demographics of the entire country, especially because our region is a highly urbanized one. Another limitation of the study was the inability to genotype the strains, as their recovery was not feasible due to the retrospective and multicenter nature of the study. However, to differentiate between M. bovis subsp. bovis and M. bovis subsp. caprae strains, the Genotype® MTBC assay was used, which allows for precise differentiation.
In summary, we noted an increasing trend in the prevalence of M. bovis isolations in the Autonomous Community of Madrid over time. M. bovis affected middle-aged patients, among whom there was a considerable percentage of immigrants. Female gender and a rural lifestyle were associated to extrapulmonary disease. This study provides essential insights into the epidemiology of M. bovis-related TB, emphasizing the necessity of continuous monitoring and understanding associated risk factors.
Ethics approvalThis study was approved by the Research Ethics Committee of the hospital where the research was conducted (22/547). Additionally, the local committees of all participating institutions also approved the study.