An adult with community-acquired Capnocytophaga canimorsus meningitis presented with a subacute course, deafness, and a predominantly lymphocytic CSF cell count.
MethodsEighteen reported cases of C. canimorsus meningitis in adults were analyzed.
ResultsIn about half the cases, CSF contained less than 1,000 leukocytes/μL or lymphocyte percentages ⩾30%. These figures differ from those usually seen in meningitis caused by the classic meningeal pathogens.
ConclusionsC. canimorsus should be included among the causes of sporadic lymphocytic meningitis in adults, in particular if the presentation involves deafness.
se presenta el caso de un adulto con meningitis comunitaria por Capnocytophaga canimorsus (MCCC) de presentación subaguda, con sordera y un líquido cefalorraquídeo (LCR) de predominio linfocitario.
Métodosse han analizado los 18 casos de MCCC descritos en adultos.
Resultadosen aproximadamente la mitad de los casos el LCR muestra menos de 1.000 leucocitos/μl, o un porcentaje de linfocitos ⩾30%, lo que difiere de la meningitis causada por los patógenos meníngeos clásicos.
ConclusionesC. canimorsus se debe incluir en la lista de causas de meningitis linfocítica de presentación esporádica en adultos, especialmente si cursa con sordera.
Capnocytophaga canimorsus (formerly referred to as DF-2) is a slow-growing, facultative anaerobic, gram-negative bacillus found in the oral flora of certain animals, such as dogs and cats. The microorganism was first described in 1976 by Bobo and Newton1. Typically, following a dog bite or close contact with dogs, Capnocytophaga canimorsus can cause systemic infections, most often in individuals with a previous splenectomy, alcohol abuse, or other types of immunosuppression, although up to 41% of cases have occurred in healthy individuals2.
To the best of our knowledge, we report the 30th case of Capnocytophaga canimorsus meningitis in the literature. Our patient was a previously healthy adult male who presented with a prolonged clinical course without fever, a predominantly lymphocytic CSF cell count, and deafness as an outstanding sign. This clinical presentation prompted us to review data that had not been thoroughly analyzed in previous reviews of this disease3,4, such as the duration of the illness before diagnosis, CSF white cell count, and sensorial and neurological complications.
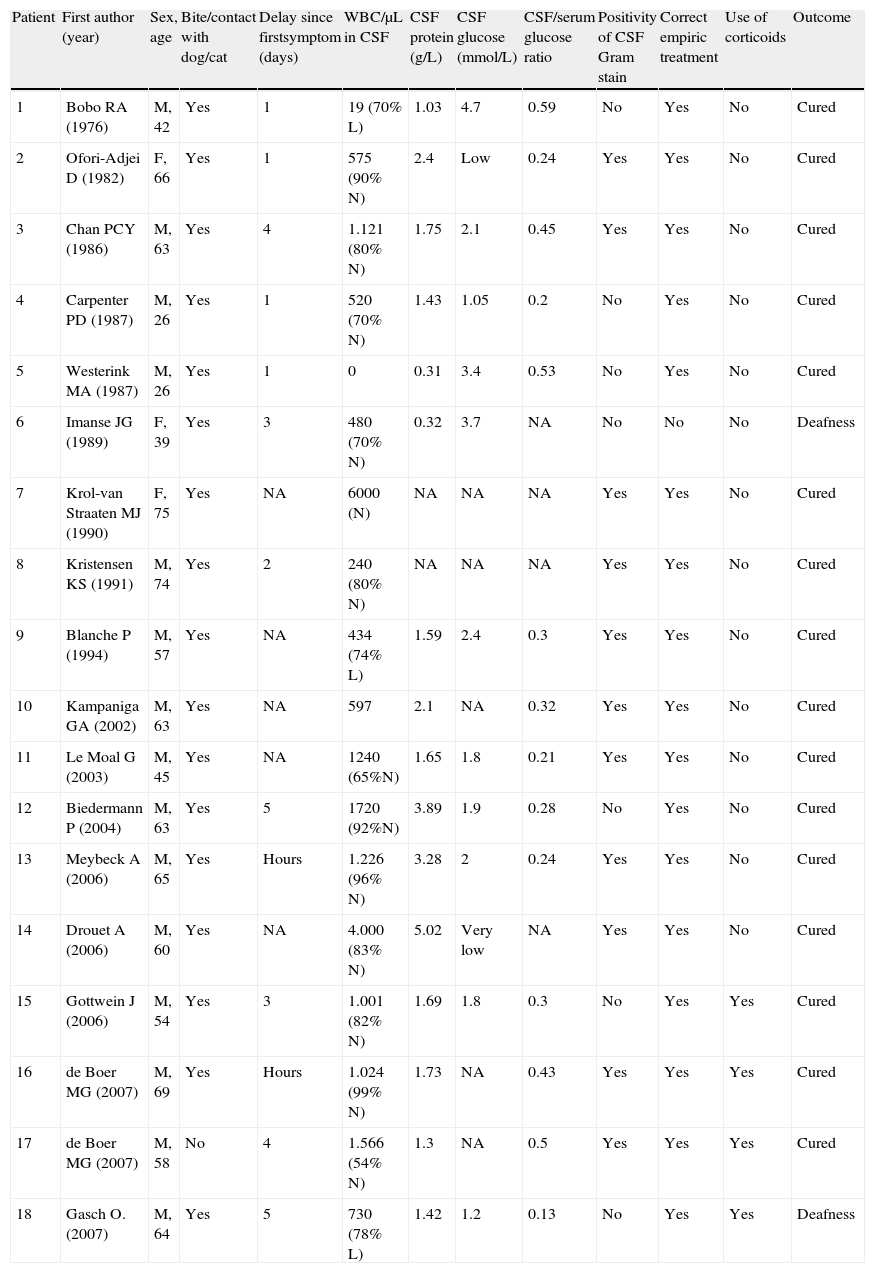
MethodsAll 30 cases of C. canimorsus meningitis reported in the English, Spanish and French literature were reviewed. Seven patients reported as having meningitis and whose specific clinical and CSF data were lacking were excluded, as well as 3 other patients who presented with severe sepsis and shock, because their clinical presentation was completely different from the presentation of patients with meningeal syndrome. One pediatric case and one hospital-acquired case were also excluded. In total, 18 cases of community-acquired C. canimorsus meningitis (CACCM) in adults (Table 1) were analyzed.
Cases of community-acquired Capnocytophaga canimorsus meningitis in adults
| Patient | First author (year) | Sex, age | Bite/contact with dog/cat | Delay since firstsymptom (days) | WBC/μL in CSF | CSF protein (g/L) | CSF glucose (mmol/L) | CSF/serum glucose ratio | Positivity of CSF Gram stain | Correct empiric treatment | Use of corticoids | Outcome |
| 1 | Bobo RA (1976) | M, 42 | Yes | 1 | 19 (70% L) | 1.03 | 4.7 | 0.59 | No | Yes | No | Cured |
| 2 | Ofori-Adjei D (1982) | F, 66 | Yes | 1 | 575 (90% N) | 2.4 | Low | 0.24 | Yes | Yes | No | Cured |
| 3 | Chan PCY (1986) | M, 63 | Yes | 4 | 1.121 (80% N) | 1.75 | 2.1 | 0.45 | Yes | Yes | No | Cured |
| 4 | Carpenter PD (1987) | M, 26 | Yes | 1 | 520 (70% N) | 1.43 | 1.05 | 0.2 | No | Yes | No | Cured |
| 5 | Westerink MA (1987) | M, 26 | Yes | 1 | 0 | 0.31 | 3.4 | 0.53 | No | Yes | No | Cured |
| 6 | Imanse JG (1989) | F, 39 | Yes | 3 | 480 (70% N) | 0.32 | 3.7 | NA | No | No | No | Deafness |
| 7 | Krol-van Straaten MJ (1990) | F, 75 | Yes | NA | 6000 (N) | NA | NA | NA | Yes | Yes | No | Cured |
| 8 | Kristensen KS (1991) | M, 74 | Yes | 2 | 240 (80% N) | NA | NA | NA | Yes | Yes | No | Cured |
| 9 | Blanche P (1994) | M, 57 | Yes | NA | 434 (74% L) | 1.59 | 2.4 | 0.3 | Yes | Yes | No | Cured |
| 10 | Kampaniga GA (2002) | M, 63 | Yes | NA | 597 | 2.1 | NA | 0.32 | Yes | Yes | No | Cured |
| 11 | Le Moal G (2003) | M, 45 | Yes | NA | 1240 (65%N) | 1.65 | 1.8 | 0.21 | Yes | Yes | No | Cured |
| 12 | Biedermann P (2004) | M, 63 | Yes | 5 | 1720 (92%N) | 3.89 | 1.9 | 0.28 | No | Yes | No | Cured |
| 13 | Meybeck A (2006) | M, 65 | Yes | Hours | 1.226 (96% N) | 3.28 | 2 | 0.24 | Yes | Yes | No | Cured |
| 14 | Drouet A (2006) | M, 60 | Yes | NA | 4.000 (83% N) | 5.02 | Very low | NA | Yes | Yes | No | Cured |
| 15 | Gottwein J (2006) | M, 54 | Yes | 3 | 1.001 (82% N) | 1.69 | 1.8 | 0.3 | No | Yes | Yes | Cured |
| 16 | de Boer MG (2007) | M, 69 | Yes | Hours | 1.024 (99% N) | 1.73 | NA | 0.43 | Yes | Yes | Yes | Cured |
| 17 | de Boer MG (2007) | M, 58 | No | 4 | 1.566 (54% N) | 1.3 | NA | 0.5 | Yes | Yes | Yes | Cured |
| 18 | Gasch O.(2007) | M, 64 | Yes | 5 | 730 (78% L) | 1.42 | 1.2 | 0.13 | No | Yes | Yes | Deafness |
CSF: cerebrospinal fluid; L: lymphocytes; N: neutrophils: NA: not aported; WBC: white blood cells.
The patient was a previously healthy 64-year-old man who was admitted to our hospital on 23 May 2006 with fever, headache, and severe hearing loss. Seven days prior to admission, he had chills and one episode of vomiting. Two days later he noticed a transient erythematous skin rash and reported moderate holocranial headache, severe hearing loss, and dizziness, which persisted when he came to the emergency room. The main reason for his decision to come to the hospital was the hearing loss. He had received three doses of 600mg ibuprofen, but no antibiotic treatment. He reported that his dog had bitten his right hand seven days before his symptoms appeared.
Physical examination disclosed slight neck stiffness, horizontal nystagmus to the right, and severe bilateral hearing deficit. Axillary temperature was 37.1°C. His right hand showed no signs of an animal bite or inflammation. The cranial CT study was normal. The results for routine hematological and chemical blood components were normal, with the exception of blood glucose at 172.8mg/dL, and C-reactive protein at 68.6mg/L. Analysis of lumbar puncture specimens revealed clear CSF with 730 white blood cells (WBC)/μL (78% lymphocytes and 22% neutrophils), 142mg/dL proteins, and 21.6mg/dL glucose. CSF Gram stain was negative. Therapy with intravenous ampicillin (4.5g every 6h) and dexamethasone (4mg every 6h) was started, and the patient experienced rapid clinical improvement with the exception of his hearing loss, which persisted unchanged. Audiometric study demonstrated severe bilateral neurosensorial deafness, whereas CT of the ears was normal.
Two days after the start of therapy, CSF culture (blood agar and chocolate agar plates, both incubated in 5% CO2 at 35–37°C) yielded a number of small, smooth, shiny, non-hemolytic bacteria. Gram stain identified some long, thin, spindle-shaped, gram-negative rods. Catalase and cytochrome oxidase reactions were positive. On conventional biochemistry reactions, the bacilli did not reduce nitrates, did not hydrolyze urea, and did not produce indole. Glucose and lactose were fermented, but raffinose, sucrose, and inulin were not. Esculin was not hydrolyzed. The ONPG assay and arginine dihydrolase reaction were both positive. The rods were identified as C. canimorsus. Antibiotic susceptibility of the microorganism was investigated by disk diffusion method using Mueller-Hinton agar with 5% sheep blood, and incubation in 5% CO2 atmosphere at 35–37°C for 48h. The microorganism did not produce beta lactamase, was susceptible to ampicillin, cefotaxime, imipenem and ciprofloxacin, and was resistant to aminoglycosides. Minimal inhibitory concentrations of antibiotics were not performed. Blood cultures were negative. Intravenous treatment with ampicillin (at the same initial dosage) plus dexamethasone (at tapering doses) was maintained for 14 days. A new lumbar puncture was performed five days after admission, and clear CSF was obtained, with 42WBC/μL (85% lymphocytes), 79mg/dL proteins, and 55.8mg/dL glucose. No additional lumbar punctures were performed. Blood glucose levels were normal at discharge. The patient was discharged with severe hearing loss as the only sequela. A second audiometric study performed one month later showed no changes relative to the previous one, and nearly total deafness persisted 6 months later.
DiscussionIn the cases we reviewed, the duration of symptoms before hospitalization of adults with community-acquired Capnocytophaga canimorsus meningitis varied from less than 24h to 5 days (median of 2 days), a period similar to that seen in classical bacterial meningitis. However, the clinical presentation can be subacute4, as was the case of our patient.
The authors of previous reviews of C. canimorsus meningitis concluded that the clinical manifestations and CSF findings are similar to those of classical bacterial meningitis3,4. They state that, apart from a possible bite wound found upon physical examination, no other symptom is known to discriminate between this rare form of meningitis and meningitis caused by other microorganisms. The authors of these studies conclude that a recent bite or contact with dogs should be investigated in cases of bacterial meningitis with no apparent microbiological cause. Overall, we agree with these conclusions. After reviewing the CSF data of published cases, however, we found that the CSF characteristics were not necessarily indistinguishable from those of classical bacterial meningitis. In about 20% of cases of community-acquired pyogenic meningitis, CSF contains less than 1000WBC/μL5,6. However, CSF WBC count was less than 1000cells/μL in 50% (9 of 18 cases) of CACCM in adults. In addition, CSF analysis in most cases of community-acquired pyogenic meningitis showed a more than 80% neutrophil content, with only 10% of cases showing a predominance of lymphocytes6,7. Nonetheless, lymphocytes predominated in 3 of the 15 cases (20%) of CACCM in adults in which CSF differential WBC count was reported, and the percentage of lymphocytes was higher than or equal to 30% in 7 of them (47%) (Table 1). Therefore, it seems that CSF in C. canimorsus meningitis often exhibits a lesser degree of pleocytosis and a higher percentage of lymphocytes than meningitis caused by classical pyogenic meningeal pathogens. These findings are similar to those usually seen in adults with meningitis due to Listeria monocytogenes6,8. This fact is interesting, because if CSF Gram stain is negative, as in 39% of the cases we analyzed (Table 1), proper diagnosis and antibiotic treatment may be delayed. Hence, we believe that previous contact with dogs (or cats) should be investigated not only in cases of clearly purulent meningitis without an apparent cause, but also in sporadic acute, and particularly, subacute meningitis with a significant or predominant percentage of lymphocytes in CSF.
Among the published cases, we found one that was quite similar to ours, a patient who presented with headache of 3 days’ duration, a high percentage of lymphocytes in CSF, and deafness9. The patient was diagnosed as having viral meningitis complicated with deafness and received no antibiotic treatment. He recovered spontaneously from the infection, but remained deaf. The authors of that report concluded that C. canimorsus should be added to the list of causes of acute deafness, and our case confirms that assertion. With the exception of this patient, the remaining patients with C. canimorsus meningitis received correct empirical antibiotic treatment, most often ampicillin and/or a third generation cephalosporin.
Our patient received empirical treatment with dexamethasone to improve his hearing loss. However, deafness was already established when the treatment was initiated and we did not perceive any favorable effect of the corticoid treatment. Among the cases reviewed, only three recently reported patients received corticoids as adjuvant therapy, as has been recommended for the initial treatment of bacterial meningitis until the cause is known10. The other reported patients did not receive adjuvant treatment with corticoids and none developed neurological complications attributable to meningitis other than deafness in the two aforementioned patients. This fact might indicate another difference with classic bacterial meningitis, in which neurological complications are frequent.
The duration of antibiotic therapy for C. canimorsus meningitis has not been established. Some authorities recommend 21 days of antibiotics, as has been recommended for gram-negative bacillary meningitis6. However, in view of the rapid clinical improvement in our patient after initiation of treatment, the duration of antibiotic therapy was limited to 14 days.
In summary, CACCM in adults is an uncommon disease that may present with a subacute course and frequently shows rather mild CSF pleocytosis with a variable but significant percentage of lymphocytes. Therefore, if CSF Gram stain does not demonstrate microorganisms, an initial diagnosis of bacterial meningitis may be difficult, especially if a background of contact with dogs is not found by performing a meticulous anamnesis. Contact with animals should also be investigated in all cases of sporadic meningitis with CSF lymphocyte predominance. Finally, we believe that C. canimorsus should be added to the possible causes of sporadic lymphocytic meningitis in adults, particularly when it presents with a subacute course and deafness.