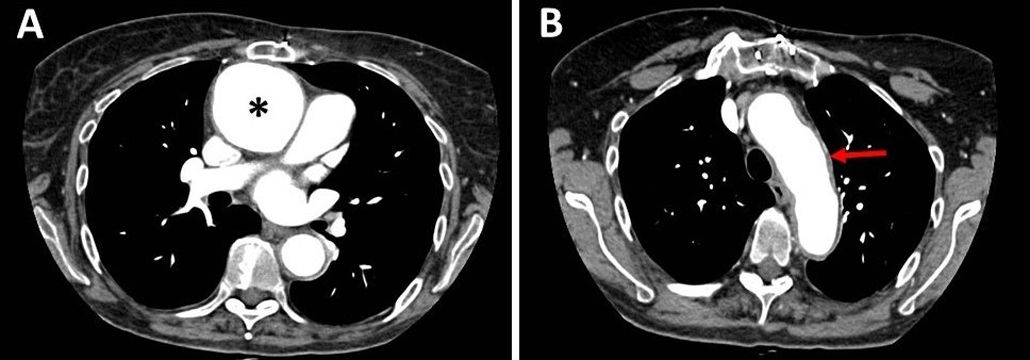
A 54-year-old woman diagnosed with end-stage idiopathic dilated cardiomyopathy underwent heart transplantation (HT). The immediate postoperative period elapsed without complications. One month later, the patient attended a follow-up appointment complaining of nonspecific chest pain and sternal wound discomfort. She was diagnosed with a postoperative mediastinal collection, after undergoing a chest computed tomography (CT) which showed an encapsulated collection extending from the superior vena cava to the anterior portion of the right atrium and right ventricle, and surrounding the aortic root. Antimicrobial treatment was not prescribed because there were no signs of infection. Cyclosporine, mycophenolate mofetil and prednisone were continued. The patient remained asymptomatic. Eight years after transplantation, a scheduled transthoracic echocardiography (TTE) described a saccular aneurysm of the ascending aorta, measuring 55mm×64mm, and significant aortic wall thickness. No vegetation or aortic valve dysfunction were observed. The aortic arch, the descending aorta and the left ventricular systolic function were normal. A CT angiography confirmed the aneurysm of the ascending aorta, which was located immediately above the aortic suture. Signs of aortitis were also seen (Fig. 1A and B). The patient mentioned slight weight loss and dyspnea on exertion, but denied having fever. On physical examination there were no stigmata of infective endocarditis. The leukocyte count was within normal range and the C-reactive protein was normal. Blood cultures were sterile. Tuberculosis, syphilis and autoimmune inflammatory disorders were excluded. The aortic aneurysm was excised and a tubular prosthesis was placed.
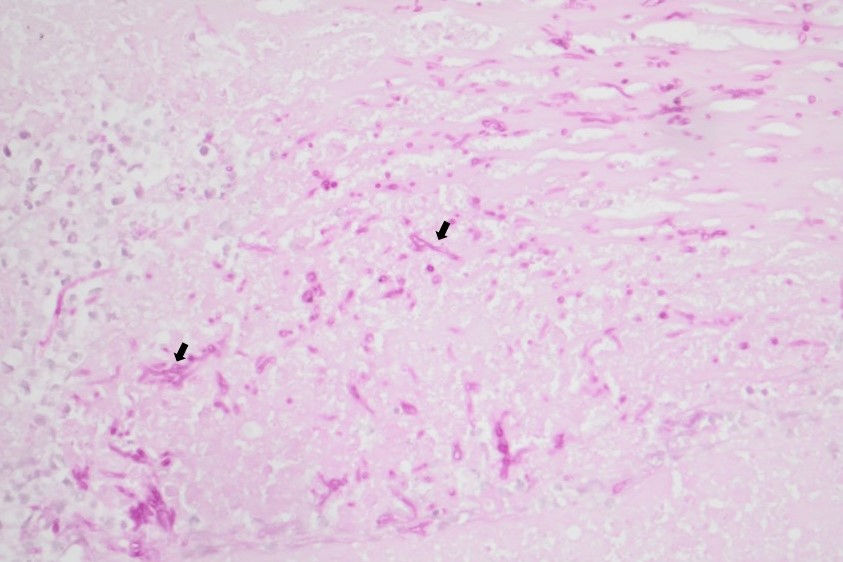
Evolution and diagnosisMacroscopic examination of the aneurysm revealed an aortic ulcer measuring 10mm×5mm. The histopathological examination of the tissued described a polymorphonuclear neutrophilic infiltrate, and a mold with septate hyphae, invading the aortic wall (Fig. 2). Microbiological cultures revealed Aspergillus flavus, which was subjected to antifungal susceptibility testing using the E-test method. The minimum inhibitory concentrations (MIC) obtained for voriconazole, posaconazole, isavuconazole, and caspofungin were 0.094mg/L, 0.064mg/L, 0.125mg/L and 0.084mg/L, respectively. According the proposed EUCAST clinical breakpoints, the isolate was informed as susceptible to azoles and echinocandins.
Aspergillus spp. aortitis is an extremely rare complication following HT, with only three cases reported to date.1–3 The elapsed time between transplantation and the diagnosis of the Aspergillus spp. infection ranged from the first weeks to several months after transplantation.
Airborne dissemination of the spores during surgery, haematogenous dissemination from the paranasal sinuses or bronchopulmonary lesions, contaminated grafts, and direct contamination of the suture lines or the aortic cannulas during surgery have been proposed as possible causative mechanisms.2 Despite our thorough investigation, the origin of our patient's infection remained elusive. Our patient had no evidence of Aspergillus spp. involvement in the lungs or other organs, and the donor, who had only spent two days in the intensive care unit before the transplant procedure, had no signs of fungal infection. Aspergillus spp. was never isolated in the different samples taken from the air filters of the cardiac surgery operating room. No other cases of Aspergillus spp. infection in contemporaneous HT recipients were diagnosed.
Diagnosis of Aspergillus spp. aortitis is difficult because patients can be asymptomatic, blood cultures are frequently negative and the TTE can overlook changes in the ascending aorta wall.1,3 In non-neutropenic patients, such as our HT recipient, both serum galactomannan and β-d-glucan assays show low sensitivity and positive predictive value, and are less useful tools for the diagnosis of aspergillosis than in neutropenic patients. Specific polymerase chain reaction (PCR) could help identify the mold in the blood. Due to the late diagnosis, it is common that, at the onset of symptoms, Aspergillus spp. has already established an extensive endovascular disease. Subsequently, several cases have only been diagnosed after death.
Treatment requires early surgical resection of the aneurysm and prolonged antifungal therapy.3 Several questions remain unanswered. It is unknown if a preoperative antifungal therapy can improve the prognosis, although delaying surgery could also increase the risk of fungal dissemination. It is unknown whether a combination of antifungal drugs has an impact in prognosis. Another unsolved question is the full length of the antifungal therapy. Most patients receive antifungal treatments for many months. The use of positron emission tomography–computed tomography (PET-CT) could help guide the duration of the antifungal treatment.
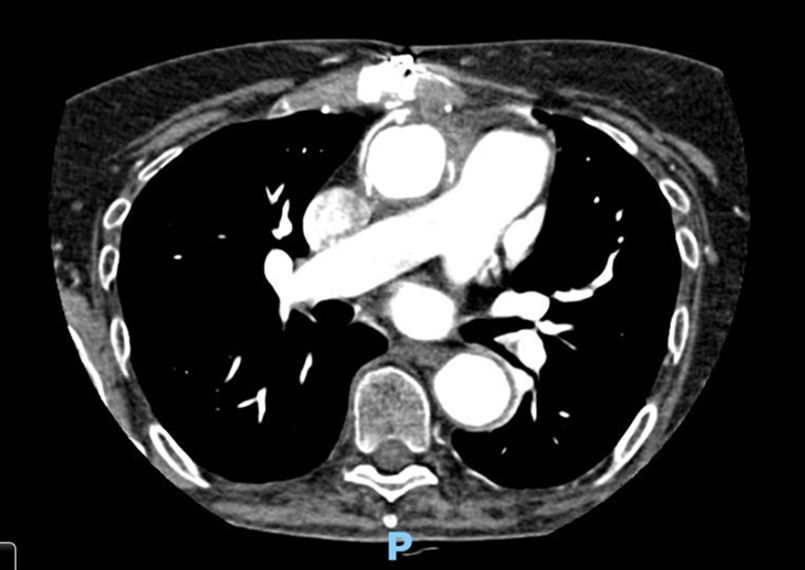
Our patient received voriconazole (400mg every 12h loading dose, followed by 200mg every 12h) combined with caspofungin (70mg/day loading dose, then 50mg/day) for 10 days, followed by voriconazole monotherapy. A CT of the thorax, brain, and paranasal sinuses did not show signs of Aspergillus spp. infection. Two serum galactomannan assays, performed 7 days apart, were also negative. Serum β-d-glucan (BDG) determination was not performed. A follow-up TTE was informed as normal, and a chest CT angiography performed three months later did not show new aneurysms or mechanical complications associated to the aortic tubular prosthesis (Fig. 3). Antifungal treatment was stopped two years later.
The patient died five years after the aortic aneurysm surgery due to a complication unrelated to her Aspergillus spp. infection. The Aspergillus spp. infection did not recur during follow-up.
In conclusion, Aspergillus spp. aortitis is extremely rare after HT, and should be suspected in HT recipients who present an aneurism of the aorta, despite the absence of fever, positive blood cultures or increased serum inflammatory biomarkers. Early surgical debridement combined with prolonged antifungal therapy is essential to improve the patient's outcome.
FundingThis manuscript did not receive any specific grant from any funding agency in the public, commercial or non-profit sector.
The authors declare that they have no conflict of interest.