This is a case of a patient diagnosed with myasthenia gravis and clinical predictors of difficult intubation and ventilation undergoing emergency surgery for eventroplasty and bowel resection. The patient was successfully intubated asleep, with no neuromuscular relaxation, using a C-MAC videolaryngoscope and difficult intubation d-Blade, following inhaled induction and topical anesthesia of the airway.
We do want to stress the clinical value of videolaryngoscopy in patients with positive predictors of difficult intubation, the applicability of Sevoflurane for the maintenance of spontaneous ventilation in a patient asleep, as well as the use of Sugammadex for reversal of neuromuscular block in a myasthenia patient.
Se describe el caso de un paciente, diagnosticado de miastenia gravis, con factores predictores de intubación y ventilación difícil, al que se practica cirugía de eventroplastia y resecciónintestinal de urgencia, que fue intubado dormido, sin relajación neuromuscular, de forma exitosa con un videolaringoscopio C-MAC y pala específica para intubación difícil (d-Blade), tras inducción inhalatoria y anestesia tópica de la vía aérea. Destacamos la utilidad clínica de la videolaringoscopia en pacientes con predictores positivos para intubación difícil, la aplicabilidad del sevoflurano para el mantenimiento de la ventilación espontánea en un paciente dormido, así como el empleo de sugammadex para revertir el uso de relajantes neuromusculares en un paciente miasténico.
The use of optical devices, as shown in the videolaryngoscopes (VDLs) picture, represents one of the major advancements in the management of the airway during the last decade. These devices provide a panoramic view of the glottis, without the need to align the axis resulting in improved glottis exposure by at least one grade in the Cormack–Lehane (C-L) scale, as compared to conventional laryngoscopy. This may very well be a legitimate option in difficult airway (DAW) situations, with a lower risk of airway trauma.1 There are different types of VDLs available but there are no conclusive trials about the superiority of one versus another.
This is the case of a patient diagnosed with myasthenia gravis (MG), with predictive factors of difficult airway, who underwent eventroplasty and emergency bowel resection and was intubated successfully with a C-MAC d-Blade VAD, following inhaled induction and topical anesthesia of the airway. We stress the clinical value of videolaryngoscopy in patients with positive predictors of difficult intubation, the applicability of Sevoflurane to maintain spontaneous ventilation in a patient asleep, as well as the use of sugammadex for reversal of neuromuscular block in a Myasthenia patient.
Clinical case67-year-old patient, 100kg and 1.65m tall (BMI 36.73kg/m2) requiring emergency bowel resection and eventroplasty surgery, diagnosed with MG with 5 years of evolution, undergoing IV immunoglobulin treatment and classified as Grade IIa according to Osserman's scale (extra-ocular disease, involvement of the limbs and axial muscles with no need for mechanical ventilation). Seven years back the patient had undergone right knee total replacement under locoregional anesthesia.
The airway evaluation showed evidence of edentation, moderate prognatism, mouth opening 2.5cm, greater mandibular branch over 10cm, cervical diameter 48cm, distance from chin to thyroid 6.2cm, chin to sternum distance 11.8cm, class two bite test, Mallampatti Class IV and extension of the atlanto-occipital joint less than 15°. These findings led to decide that the patient met the difficult airway criteria, further exacerbated by the non-deferrable surgical indication and the fact that the patient had an illness that demanded particular care with the use of neuromuscular blockers. The anesthetic technique suggested was inhaled induction and videolaryngoscopy (VDL C-MAC with DAW specific d-Blade) with local anesthetic instillation according to the spray as you go (SAYGO) technique to avoid the use of NMB in the induction of anesthesia.
Non-invasive monitoring resulted in a sinus rate of 77 beats per minute, blood pressure 140/79, peripheral oxygen saturation 93% with room air and depth of anesthesia of 94 according to the bi-spectral index BIS.
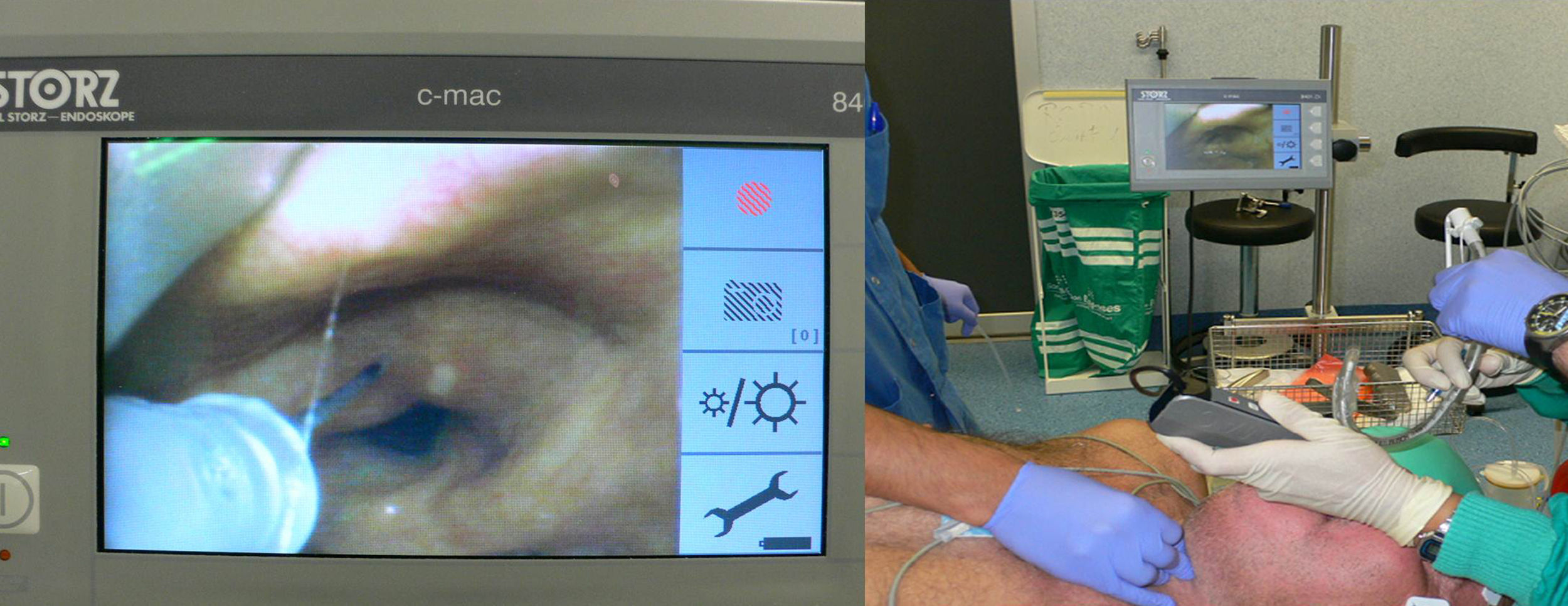
The patient was pre-oxygenated and started with 5% sevoflurane administered through facemask, according to the inhaled induction regimen at tidal volume until achieving a Guedel grade III anesthetic depth in plane I. The patient exhibited spontaneous ventilation confirmed through capnography, SaO2 96% and a BIS of 55–60, HR 70bpm and BP 123/63. At this point a diagnostic laryngoscopy with a number 4 MacIntosh blade determined a Grade C-L III-B and hence the C-MAC d-Blade laryngoscope was introduced, a grade C-L I was obtained and an epidural catheter was introduced for the administration of topical anesthesia to the epiglottis, the arytenoid, the glottis and the trachea, with the administration of 250mg of 2% Lidocaine according to SAYGO (Fig. 1).
The patient then underwent orotracheal intubation (OTI) with an 8.0 endotracheal tube (ETT). The intubation was confirmed using capnography, and then 40mg of rocuronium were administered followed by intraoperative monitoring of the degree of neuromuscular block using a TOF-Watch monitor. The surgery was uneventful. After the spontaneous neuromuscular recovery of T2, 2mg/kg of sugammadex were administered reversing the NMB (T4/T1≥90%) at 90s. The patient was extubated uneventfully. The evolution during the immediate postoperative period was favorable and the patient was discharged to the hospital floor after a few hours.
DiscussionThis clinical case gives rise to several interesting aspects. First and foremost, proper knowledge and interpretation of the algorithms proposed by the American society of Anesthesiologists (ASA) to identify and manage a DAW2 is mandatory. In the event of a predicted difficult airway the recommended technique of choice is intubation with the patient in spontaneous ventilation, upon receiving the required information and preparation. This means adequate pre-oxygenation and sedation aimed at preventing the loss of spontaneous breathing and muscle tone, in addition to topical anesthesia of the oropharynx or nasopharynx and the laryngotracheal region.3 Once a Grade C-L IIIb was determined through diagnostic laryngoscopy, the patient was intubated using the VDL C-MAC d-Blade in order to achieve a patent airway isolated from the GI tract, considering the risk of regurgitation of patients with MG and the high incidence of paralysis of the soft palate.4
Secondly, the management of the difficult airway requires a fundamental premise: safety. The hypnotic agent used must meet three basic goals: low airway irritability, minimum respiratory depression and rapid reversibility. Sevoflurane meets the three conditions and hence is suitable for managing the dubious or predicted difficult airway, maintaining the patient's spontaneous ventilation and controlling the depth of anesthesia, generating a respiratory pattern, which is above all predictable and controllable. Thus Sevoflurane may be a suitable drug for anesthetic induction in patients with MG.5–7
A third point to debate is the ability to deal with neuromuscular diseases such as MG with no risk of residual curarization.8 In this regard, the generalized use of sugammadex and the adoption of the new neuromuscular relaxation monitors to the clinical practice seems critical.8–10
Although the use of VDLs has been described in multiple cases, it is in cases of predicted or unexpected DAW where its use has been most attractive for the solution of such a feared problem. However, there are a limited number of studies assessing the superiority of any particular type of VDL in case of DAW.
The most relevant study includes 200 patients with positive predictors for DAW (Mallampati III and IV) and compares C-MAC against Macintosh laryngoscope. The trial concludes that C-MAC provides better vision, higher success rate in intubation (99% versus 92%), shorter time and use of optimization maneuvers such as BURP, bougie or changes in the head position.11
Another study in morbid obese patients (150 patients in total) found that C-MAC is also superior to either the Glidescope or Mc-Grath videolaryngoscopes. C-MAC provides for easier intubation, less stylet use, shorter intubation time and higher first attempt success rate.12 McElwain at al compared the videolaryngoscopes C-MAC, Glidescope, Airtraq and the Macintosh laryngoscope in dummies, and concluded that C-MAC was the easiest to use, with shorter intubation times in DAW.13
The C-MAC videolaryngoscope has a more angulated special blade (d-Blade) particularly helpful in situations in which the glottis vision with the C-MAC traditional Macintosh blade is just partial or deformed as a result of a laryngeal tumor or due to external compression. Hence, it is considered a wise and fast option as salvage intubation in DAW.14 Likewise, C-MAC facilitates the use of a bougie as an adjunct in the management of these situations.15
The evidence available so far leads us to consider that VDLs are the first choice for the management of the unexpected difficult airway or for approaching positive predictor patients who may be intubated.16 The process may be more effective using an inhaled induction technique and topical anesthesia of the airway.6–7
Notwithstanding the fact that until know fibrobronchoscopy and intubation with the patient awake has been the standard practice,2,3 the reliability and safety offered by the VDL has consolidated it as an efficacious alternative for managing these situations.17
FundingNone
Conflicts of interestThe authors hereby declare no conflicts of interest.
Please cite this article as: Gutiérrez JCG, et al. Inducción inhalatoria y anestesia tópica de la vía aérea guiada por videolaringoscopio pala en un paciente con miastenia gravis y vía aérea difícil. Rev Colomb Anestesiol. 2013;41:287–290.