Pemphigoid gestationis (PG) is one of the main dermatoses of pregnancy that must be recognized and treated promptly, since it is related to worsening of foetal prognosis. Although skin involvement has been investigated, there is a lack of morphological and functional studies of the placenta in this pathology.
Main symptoms and/or clinical findingsErythematous vesicular rash at 32+1 weeks of gestation.
Main diagnosesPG.
Therapeutic interventions and resultsImmunogammaglobulin in severe cases refractory to oral corticosteroids with complete disappearance of the lesions.
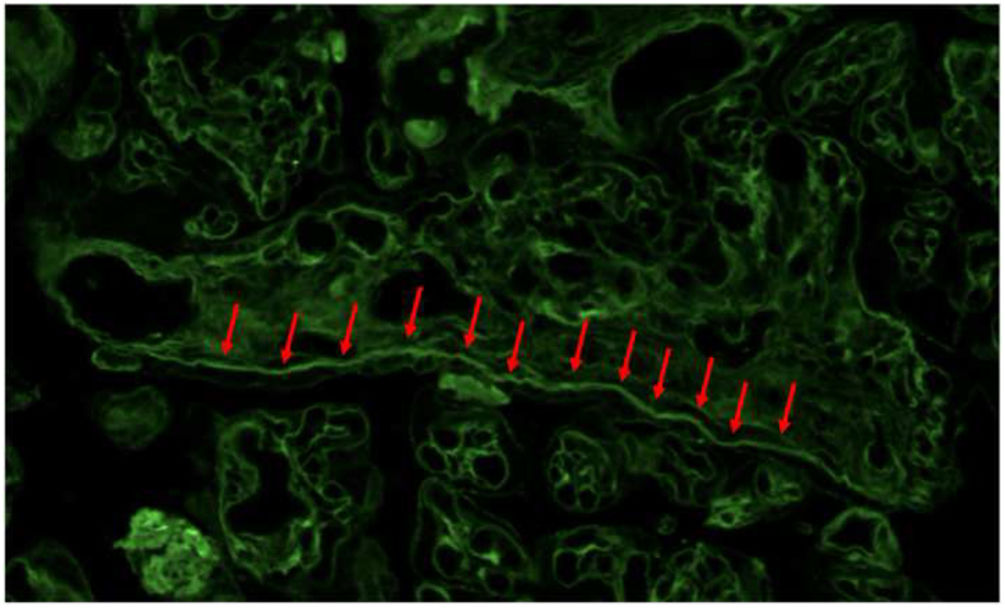
ConclusionTo our knowledge, this is the first case to report a detailed analysis of IgG and C3 deposits in the basement membrane of the placental villi by means of an immunofluorescence study. These findings could be related to a slight malfunction of the placenta that may explain the adverse neonatal effects.
El herpes gestationis (HG) es una de las principales dermatosis del embarazo que debe ser reconocida y tratada oportunamente ya que se relaciona con un empeoramiento del pronóstico fetal. Aunque se ha investigado la afectación cutánea, hay escasez de estudios morfológicos y funcionales de la placenta en esta patología.
Principales síntomas o hallazgos clínicosErupción vesicular eritematosa a las 32+1 semanas de gestación.
Diagnósticos principalesHG.
Intervenciones terapéuticas y resultadosInmunogammaglobulina en casos graves refractarios a los corticoides por vía oral con desaparición completa de las lesiones.
ConclusiónHasta donde sabemos, este es el primer caso que reporta un análisis detallado de los depósitos de IgG y C3 en la membrana basal de las vellosidades de la placenta mediante un estudio de inmunofluorescencia. Estos hallazgos podrían relacionarse con el ligero mal funcionamiento de la placenta que puede explicar los efectos neonatales adversos.
Skin changes are frequent during pregnancy. They can be classified into physiological benign changes, alterations in pre-existing skin diseases due to immunohormonal changes and pregnancy-specific dermatoses. Pemphigoid gestationis (PG) is belongs to these last ones. In this article we will try to illustrate the pathophysiological bases of this disease.
Patient informationA 44-year-old Caucasian primigravid woman with a singleton pregnancy conceived by IVF. No personal medical history of interest except for pregestational hypothyroidism. Current treatment: acetylsalicylic acid 100mg/d, levothyroxine 125mcg/d, vitamin D 5gouts/d and multivitamin complex for pregnancy. The patient gave her informed consent for the publication of the case.
Clinical findings and temporal lineThe pregnancy was uneventful until week 32+1 when she presented erythematous plaques which appeared periumbilically and spread all around the body affecting both limbs, legs, and feet in less than 24h.
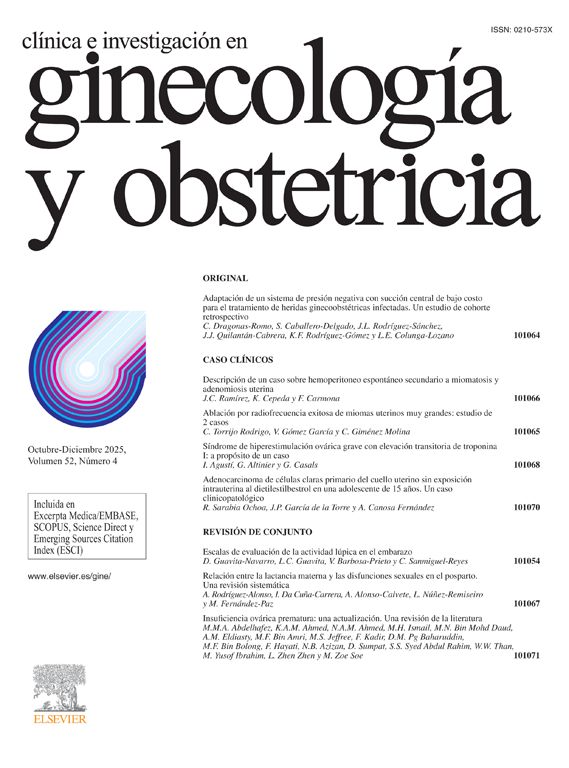
Diagnostic evaluationThe patient was referred to the Department of Dermatology where a skin biopsy was performed. In the pathological study a subepidermal blister with numerous eosinophils inside was observed. Spongiotic epidermis and superficial perivascular lymphocyte infiltrate were also seen. By direct immunofluorescence (DIF), a linear IgG and complement (C3) deposits were observed all through the dermoepidermal junction (Fig. 1). This last finding was the key piece for the diagnosis of pemphigoid gestationis.
Therapeutic interventionPrior to final diagnosis, empiric treatment with dexchlorpheniramine (2mg/8h) and deflazacort (60mg/d) was initiated. After descending deflazacort dose to 45mg/d, the patient attended the emergency department because a worsening of the eruption, so the initial dose was recovered. After the absence of clinical remission, we considered, in consensus with the dermatological team, to administer non-specific intravenous immunoglobulin at a dose of 1g/kg/day for two consecutive days. Another cycle was repeated after 4 weeks (36+4 weeks). After Ig therapy the skin lesions quickly subsided. Nevertheless, antihistamines and corticosteroids were needed until the end of the pregnancy for symptomatic control.
Follow up and resultsFollow-up of the pregnancy was normal, with foetal scans performed every two weeks showing normal growth. No side effects were reported during the treatment.
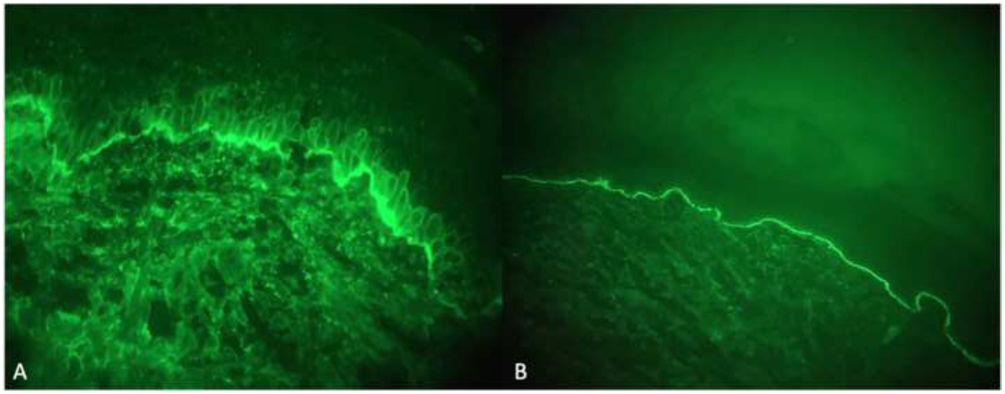
We programmed induction of labour at 37+4 weeks of gestation. A girl was born by normal vaginal delivery, with good vital signs, Apgar 9/10 at 1 and 5min, arterial cord blood pH 7.29. There was an uneventful placental delivery, which was sent to the Department of Pathology for macroscopical, histological and IF examination. Macroscopic and histological examination did not show significant alterations. DIF examination showed a linear deposit of IgG and complement (C3) in villous basement membrane, predominantly in medium and large villi, widely distributed in the placenta (Figs. 2 and 3).
After hospital discharge, corticosteroids with deflazacort 45mg/d was continued for two weeks and then changed to prednisone 20mg/d that was tapered off gradually. The lesions disappeared four weeks postpartum. To date, the patient has not presented cutaneous symptoms again. On the other hand, the newborn did not present lesions of similar characteristics.
DiscussionPemphigoid gestationis shows a worldwide distribution, with an approximate incidence of 1 in 50,000 pregnancies. No ethnic differences are found.1 Although it is more frequent in multiparous women in the second or third trimester, it can happen each time placental tissue is present which implies that it may appear in the context of an ectopic pregnancy, a trophoblastic disease or a miscarriage. Up to 30% of cases, it can occur in the immediate puerperium.2–4
It is an autoimmune disease, produced by the synthesis of IgG type antibodies,2 targeted to the BP180 protein (also known as BPAG1 or collagen XVII). A strong association with the maternal HLA-DRs*0301 (HLA-DR3) and DRB1*0401-040X (HLA-DR4) has been detected. While the combination of these two HLA haplotypes is found in 45% of PG patients, it is in only present in the 3% of control women. MHC class II molecules are abnormally expressed on amniochorionic stromal cells and on the trophoblast. Therefore, there is a loss of the immuneprivilege of the fetoplacental unit. BP180, which is usually expressed on the amniotic epithelium of the placenta and the umbilical cord, is now presented to maternal MHC class II in the presence of paternal MHC II triggering the subsequent production of anti-placental IgG antibodies. In cooperation with the C3 fraction of complement, these antibodies form immunocomplexes that bind to the amniotic membrane causing the immunological insult. Previously reported pathological exam revealed findings such as lymphocyte infiltration, deficit in the development in desmosomes and partial detachment of basement membranes from the trophoblast. To our knowledge, this is the first case reporting a detailed analysis of IgG and C3 deposits in villous basement membrane of the placenta by DIF study. Other studies have reported DIF study of the placenta but less explained.5
Apart from the placenta, BP180 is expressed in the skin and central nervous system. In the skin, it acts as hemidesmosomal transmembrane glycoprotein, which anchors the epidermis to the dermis. When anti-BP180 cross react with collagen XVII in the maternal skin, immunocomplexes are formed, complement cascade is activated and inflammatory cells are recruited leading to degranulation of eosinophils and neutrophils. Degranulation products, among them proteases, are presumably responsible of dermo-epidermal detachment. Clinically, this phenomenon is seen as blisters and erosions.
PG activity usually declines to the end of pregnancy, when progesterone levels are high. By contrast, when progesterone levels decrease postpartum, it may eventually flare. For this reason, the pathogenic cascade is thought to be modulated by the maternal hormonal environment
In relation to prognosis, patients who develop PG during pregnancy are at higher risk for complications for both mother and foetus, contrary to other pregnancy dermatoses. Adverse outcomes5 such as preterm delivery6 and growth restriction3,6 may be justified by placental insufficiency caused by damaged placental tissue. The worsening of the foetal prognosis justifies the end of the pregnancy after week 37. Skin lesions may occur in up to 10% of neonates from mother with this disease due to antibodies vertical transfer, but lesions resolve spontaneously.
To achieve adequate prevention of these potential complications, it is crucial to make an early and good diagnosis. Although alternative strategies such as detection of circulating antibodies had been proposed, currently the PG diagnosis relies in the performance of a biopsy that reveals a linear, dense and regular deposit of the C3 fraction of complement with or without IgG at the dermoepidermal junction.1,3,4,6,7 The immunohistochemistry exam allows us to make a differential diagnosis with other dermatosis of pregnancy more frequent than PG, not necessarily associated with perinatal complications.
In relation to maternal prognosis, as it has been said, many patients experience a remission in late pregnancy, sometimes followed by a flare immediately after delivery, which usually occurs in the first 4 weeks. For this reason, these patients should be closely followed by a dermatologist for the first few months after delivery. In any case, the disease is self-limited.4 Recurrences in subsequent pregnancies are frequent, regardless of partner change, and tend to be more severe and start earlier. However, it does not have to appear in the following one. Recurrence in alternate pregnancies has been described.1,4
In reference to the treatment, the main goals are to stop blistering, decrease itching, and prevent secondary infection. For the latter, the use of cold compresses on the lesions and the drainage of large blisters is recommended.8 Topical corticosteroids associated with oral antihistamines may be sufficient in milder cases, although the use of oral corticosteroids is usually necessary. In moderate-severe cases, in addition to increasing the dose of systemic corticosteroids, intravenous immunoglobulins should be considered. This novel treatment has proven to be safe during pregnancy and highly effective, as this group has shown in previous works.1,9–11 In the case of persistent postpartum symptoms that are refractory to corticosteroid treatment, systemic immunosuppressants such as cyclosporine A, dapsone, azathioprine, or methotrexate may be beneficial.1
Pemphigoid gestationis is an exclusively gestational pathology of autoimmune origin with cutaneous expression that can be associated with adverse foetal events. As described in this case, pathological placental findings have been found that could justify its functional alteration and, therefore, adverse neonatal events, emphasizing the importance of studying the placenta in PG cases. For treatment, although not available in all centres, it is worth highlighting the use of intravenous immunoglobulins in cases refractory to corticosteroids, which have shown great effectiveness with a very good safety profile. As always, the interdisciplinary management of the disease by obstetricians, dermatologists, pathologists, and neonatologists is crucial.
Ethics approvalThe patient gave her informed consent for the publication of the case.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments have been performed on humans or animals for this research.
Data confidentialityThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis research has not received specific aid from agencies from public or commercial sectors or non-profit entities.
Conflict of interestsThe authors declare that no conflicts of interest exist regarding the publication of this paper.
The authors thank all the contributors that have participate in the diagnosis of this case.