The aim of this study is to evaluate the relationship and the accuracy of SCORE (Systematic Coronary Risk Evaluation Project) risk correlated to multiple methods for determining subclinical cardiovascular disease (CVD) in a healthy population.
Material and methodsThis cross-sectional study included 120 completely asymptomatic subjects, with an age range 35–75 years, and randomly selected from the general population. The individuals were evaluated clinically and biochemical, and the SCORE risk was computed. Subclinical atherosclerosis was assessed by various methods: carotid ultrasound for intima-media thickness (cIMT) and plaque detection; aortic pulse wave velocity (aPWV); echocardiography – left ventricular mass index (LVMI) and aortic atheromatosis (AA); ankle-brachial index (ABI).
ResultsSCORE mean value was 2.95±2.71, with 76% of subjects having SCORE <5. Sixty-four percent of all subjects have had increased subclinical CVD changes, and SCORE risk score was correlated positively with all markers, except for ABI. In the multivariate analysis, increased cIMT and aPWV were significantly associated with high value of SCORE risk (OR 4.14, 95% CI: 1.42–12.15, p=0.009; respectively OR 1.41, 95% CI: 1.01–1.96, p=0.039). A positive linear relationship was observed between 3 territories of subclinical CVD (cIMT, LVMI, aPWV) and SCORE risk (p<0.0001). There was evidence of subclinical CVD in 60% of subjects with a SCORE value <5.
ConclusionsAs most subjects with a SCORE value <5 have subclinical CVD abnormalities, a more tailored subclinical CVD primary prevention program should be encouraged.
Nuestro objetivo fue evaluar la relación y la precisión de la Systematic Coronary Risk Evaluation–Evaluación Sistemática del Riesgo Coronario (evaluación SCORE) correlacionada con múltiples métodos para determinar la enfermedad cardiovascular (ECV) subclínica en una población sana.
Material y métodosEste estudio transversal incluyó a 120 personas asignadas al azar de la población general. Los sujetos con edades entre 35 y 75 años y completamente asintomáticos fueron evaluados desde el punto de vista clínico y bioquímico, y se calculó su riesgo SCORE. Se evaluó la aterosclerosis subclínica mediante varios métodos: ecografía carotídea para la determinación del grosor íntima-media y la detección de la placa; velocidad de la onda de pulso aórtico; ecocardiografía-índice de masa ventricular izquierda y ateromatosis aórtica; índice tobillo-brazo.
ResultadosEl valor medio de la puntuación SCORE fue de 2,95±2,71, con un 76% de los sujetos con una puntuación<5. El 64% de todos los sujetos tenía cambios aumentados de ECV subclínica y la puntuación SCORE se correlacionó positivamente con todos los marcadores, excepto el índice tobillo-brazo. El 40% de los sujetos tenía placas carotídeas y el 70% ateromatosis aórtica. En el análisis multivariante, los valores aumentados del grosor íntima-media y de la velocidad de la onda de pulso aórtico se asociaron significativamente con un alto valor de riesgo SCORE (CP 4,14; IC del 95%: 1,42-12,15; p=0,009; respectivamente CP 1,41; IC del 95%: 1,01-1,96, p=0,039). Se observó una relación lineal positiva entre 3 territorios de ECV subclínica (grosor íntima-media, índice de masa ventricular izquierda, velocidad de la onda de pulso aórtico) y el riesgo SCORE (p<0,0001). El 60% de los sujetos con el valor SCORE<5 tenían indicios de ECV subclínica.
ConclusionesLa puntuación SCORE se correlaciona positivamente con la mayoría de los marcadores ateroscleróticos. Como la mayoría de los sujetos con valor SCORE<5 tienen anomalías relacionadas con la ECV subclínica, es necesario promover una prevención primaria mejor adaptada de la ECV subclínica.
Atherosclerotic cardiovascular diseases (CVD) represent the main cause of morbidity and mortality worldwide, requiring intensive medical surveillance and expensive therapies; however the long term prognosis still remains poor.1,2 Primary prevention of CVD costs less than treating its complications and is based on the reduction of cardiovascular risk factors. With a continuous attention toward proper identification of patients, various algorithms of CVD risk stratification have been proposed and tested during time.3,4 Based on the classification in different risk class categories, lifestyle changes or even pharmacological therapy for high risk patients are recommended. However, an acute atherosclerotic cardiovascular event represents the first manifestation in 30–50% of individuals that have been initially included into low to intermediate risk classes.5
It is clear that a simple quantification of risk factors is not sufficient for an accurate CVD primary prevention and the current guidelines admit this limitation.1,6 Since atherosclerosis develops silently before clinical manifestations occur, the evaluation of the diseased arterial wall provides a personalized and early assessment of at-risk subjects. Several parameters of subclinical CVD and atherosclerosis have been proposed for the detection of intermediate and high-risk populations, with reasonable CVD predictive value. Carotid intima-media thickness (cIMT) and identification of atherosclerotic plaques by carotid ultrasonography,7 ankle-brachial index (ABI) for evaluating the peripheral artery disease8 or the detection of aortic atheromatosis and left ventricular (LV) hypertrophy by echocardiography9 proved to be valuable markers for CVD screening. More recently introduced into clinical practice, the aortic pulse wave velocity (aPWV) proved to be an independent predictor of CVD in healthy individuals.10
Recently, the SHAPE (Screening for Heart Attack Prevention and Education) program recommended the screening for subclinical atherosclerosis in asymptomatic subjects aged 45–75 years in men and 55–75 years in women at intermediate risk.5 According to the European and American CVD prevention guidelines, the measurement of ABI, IMT and the screening for carotid atherosclerotic plaques in asymptomatic adults at intermediate risk should be considered.1,6 The role of echocardiography for the general screening in population is not well defined. Moreover, the arterial stiffness measurement is not yet included as recommended screening method despite multiple evidences that supports the PWV predictive role in CVD.10–12 However, the comprehensive evaluation of subclinical CVD using the four up-mentioned screening tools in asymptomatic population has not been previously described. Thus, we aimed (1) to evaluate the subclinical CVD and atherosclerotic burden in a randomly, healthy, adult population by using carotid ultrasound, echocardiography, ABI and arterial stiffness parameters, respectively; (2) to correlate the CVD risk score with determinants of subclinical CVD; and (3) to quantify the proportion of patients who should be reclassified compared with traditional risk factor scoring.
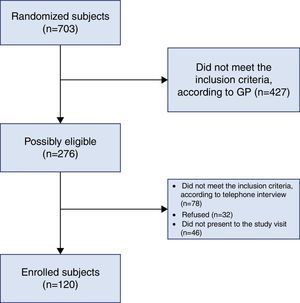
MethodsStudy design and populationA single-center, cross-sectional, observational study was conducted over a 2-year period between January 2014 and November 2015. Inclusion criteria: apparently healthy individuals, aged 35–75 years, recorded on the local general practitioners data lists. Exclusion criteria: pregnant or breastfeeding women recorded on the above mentioned local general practitioners data lists. From the medical subjects’ data lists of the local general practitioners, 703 subjects have been randomized, of whom 276 were apparently healthy individuals, aged 35–75 years and the women not pregnant or breastfeeding. The “asymptomatic” status of the subjects was defined by not having any previous recorded acute or chronic diseases and not being under any chronic treatment. Further eligibility was ascertained by telephone interview directly with the subjects and finally 120 subjects were included in the study (Fig. 1). The study protocol was approved by the local University Ethics Committee and all participants provided written informed consent before enrollment. The methods used in this study have complied with the Helsinki Declaration.
At study visit, an interview was conducted with all participants and data regarding basic cardiovascular risk factors were recorded. By physical examination, height, weight and waist circumference were measured and the body mass index was calculated. The office blood pressure measurement was performed by respecting the 2013 European guidelines.13 A fasting venous blood sample was obtained for biochemical analysis, including lipid profile, plasma glucose and serum creatinine.
SCORE risk scoreFor each subject, the HeartScore® risk was computed from specific risk factors by using age, gender, smoking status, systolic blood pressure and total cholesterol.4 The SCORE (Systematic Coronary Risk Evaluation Project) risk provides a 10-year direct estimation of total cardiovascular mortality risk and the specific chart for high-risk countries has been used in the current study. For a practical approach, the subjects have been classified into two risk categories based on the SCORE result: low to intermediate risk (1 to <5%); and high to very high risk (≥5%).
Subclinical atherosclerosis markerscIMT and carotid plaques were examined using ultrasonography (MyLab™50 XVision model, Esaote Group, Genoa, Italy) by an experienced physician blinded to all patient data and interpreted according to the Mannheim criteria.14 The carotid plaque was defined as cIMT thickness above 1.5mm or as a focal wall protrusion into the arterial lumen of at least 0.5mm or 50% of the surrounding cIMT value. The cIMT was measured on the posterior wall of the common carotid artery 10mm proximal to the carotid bulb. Although the cardiovascular risk is higher with the increasing of cIMT, a value more than 0.9mm is considered abnormal.1
Transthoracic echocardiography was performed by the same operator using the cardiac software of the same ultrasound machine (Mindray DC-T6 Ultrasound Machine). For the current research, the visual detection of aortic atheromatosis in the proximal ascending aorta and evaluation of LV mass as parameter of subclinical organ damage represented the main focuses. The values were indexed by body surface area to obtain the LV mass index (LVMI) with the reference upper limits being 95g/m2 in women and 115g/m2 in men.
ABI measurement was performed after 10min of rest and in supine position, by a single trained person. The systolic blood pressure was initially measured in both arms and the highest brachial systolic value was considered the denominator in the ABI calculation. Afterwards, the systolic blood pressure was measured at the lower limbs in both posterior tibial and dorsally pedis arteries. The highest value obtained for each leg was the numerator in the final equation. A ratio <0.9 was considered the threshold for peripheral artery disease.
The aPWV was assessed using the Arteriograph system (Tensiomed, Budapest, Hungary). It is a relatively new device which uses the oscillometric method. The Arteriograph results have been previously validated, by comparing both with invasive methods and with other devices for PWV determination.15,16 Besides the aPWV, the device also provided other arterial stiffness parameters such as the aortic systolic blood pressure (SBPao) and the augmentation indexes (brachial, AIXbr and aortic, AIXao).
Statistical analysisData analysis was performed using SPSS 20.0 (Statistical Package for the Social Sciences, Chicago, Illinois). Data were presented as mean±standard deviation (SD) and number of cases with percent frequency, for continuous and categorical variable, respectively. The two SCORE risk categories were comparatively analyzed for all variables. Continuous variables were compared using Independent-Samples T Test and One Way ANOVA analysis of variances. Comparisons based on different categories were performed by chi-square test and by Fisher's exact test. Variables with p<0.05 in univariate analysis were selected for multivariate analyses, by logistic regression. This was used to assess the association between selected variables and SCORE, as the dependent variable, and to develop a new predictive model for the risk. Odds ratio (ORs) with 95% confidence interval (CI) was used to report the results. The predictive model was assessed by receiver operating characteristic (ROC) curve (C-statistic) analysis. The degree of agreement between SCORE and the other methods used to assess subclinical atherosclerosis was measured by Cohen's kappa coefficient. Relationship between two variables was determined by Pearson's correlation coefficient. A two-sided p value <0.05 was considered significant for all data analyses.
ResultsBaseline characteristicsThe clinical and biological characteristics of the study group are outlined in Table 1. Two thirds of subjects were females and the mean age of patients was 52 years. Among traditional cardiovascular risk factors, 21% of the subjects were current smokers, 12.5% presented chronic alcohol intake and approximately one third had a positive family history of CVD. Overall, the study participants were overweight and total-, LDL- and non-HDL cholesterol mean values were mildly elevated. However, triglycerides, HDL-cholesterol, plasma glucose, renal function and blood pressure were within normal range. Nonetheless, 34 (28.3%) of individuals were hypertensive. The mean SCORE value was 2.95 (median 2), ranging from 1 to 13.
Characteristics of the study population according to SCORE risk score.
| Characteristic | All subjects (n=120) | SCORE <5 (n=92) | SCORE ≥5 (n=28) | p value |
|---|---|---|---|---|
| Age, years | 52.01±10.73 | 48.42±9.09 | 63.79±6.43 | <0.0001 |
| Male, n (%) | 40 (33.3) | 23 (25) | 17 (60.7) | |
| Current smoker, n (%) | 26 (21.6) | 18 (19.5) | 8 (28.5) | 0.24 |
| Former smoker, n (%) | 22 (18.3) | 15 (16.3) | 7 (25) | |
| Never smoker, n (%) | 72 (60) | 59 (64.1) | 13 (46.4) | |
| Alcohol consumers, n (%) | 15 (12.5) | 6 (6.5) | 9 (32.1) | 0.0011 |
| Family history of CVDa, n (%) | 36 (30) | 31 (33.7) | 5 (17.8) | 0.083 |
| Body mass index, kg/m2 | 28.50±5.34 | 28.28±5.24 | 29.23±5.67 | 0.414 |
| Waist circumference, male, cm | 103.60±10.29 | 102.91±11.52 | 104.58±8.60 | 0.308 |
| Waist circumference, female, cm | 97.2±13.62 | 96.14±13.23 | 103.81±14.84 | 0.041 |
| Systolic blood pressure, mmHg | 127.30±17.22 | 123.16±15.14 | 140.89±16.86 | <0.0001 |
| Diastolic blood pressure, mmHg | 81.27±13.07 | 78.52±12.10 | 90.29±12.22 | <0.0001 |
| Cholesterol total, mg/dl | 209.77±45.56 | 205.38±44.66 | 224.19±46.32 | 0.055 |
| LDL cholesterol, mg/dl | 129.96±40.71 | 128.93±40.67 | 133.45±41.43 | 0.614 |
| HDL cholesterol, mg/dl | 52.49±14.47 | 52.13±13.92 | 53.70±16.35 | 0.616 |
| Non HDL cholesterol, mg/dl | 157.27±44.89 | 153.25±44.58 | 170.48±44.12 | 0.075 |
| Triglycerides, mg/dl | 137.06±81.42 | 121.59±64.07 | 187.90±109.02 | 0.0001 |
| Plasma glucose, mg/dl | 97.21±12.75 | 95.59±11.87 | 102.51±14.28 | 0.011 |
| eGFR, ml/min/1.73m2 | 89.35±16.54 | 92.38±15.98 | 79.62±14.67 | 0.0002 |
| SCORE risk | 2.95±2.71 | 1.65±0.97 | 7.21±2.16 | <0.0001 |
| cIMT, mm | 0.86±0.13 | 0.83±0.12 | 0.97±0.10 | <0.0001 |
| cIMT >0.9mm, n (%) | 44 (36.7) | 23 (25) | 21 (75) | <0.0001 |
| Carotid plaques, n (%) | 48 (40) | 27 (29.3) | 21 (75) | <0.0001 |
| LVMI, g/m2 | 101.54±23.25 | 99.10±21.40 | 109.78±27.50 | 0.035 |
| LVMI increased (>95 in women/>115 in men), n (%) | 54 (45) | 41 (44.5) | 13 (46.4) | 0.473 |
| Aortic atheromatosis, n (%) | 85 (70.8) | 57 (62) | 28 (100) | <0.0001 |
| ABI | 1.08±0.13 | 1.08±0.8 | 1.05±0.24 | 0.210 |
| aPWV, m/s | 8.28±1.79 | 7.87±1.64 | 9.48±1.66 | <0.0001 |
| Central systolic blood pressure, mmHg | 128.14±21.05 | 122.88±18.67 | 143.73±20.24 | <0.0001 |
| AIXbr, % | −0.98±31.03 | −4.75±30.35 | 10.04±30.91 | 0.028 |
| AIXao, % | 37.04±15.60 | 35.06±15.24 | 42.85±15.40 | 0.021 |
ABI: ankle-brachial index; AIXao: aortic augmentation index; AIXbr: brachial augmentation index; aPWV: aortic pulse wave velocity; cIMT: carotid intima-media thickness; CVD: cardiovascular diseases; eGFR: estimated glomerular filtration rate; HDL: high-density lipoprotein; LDL: low-density lipoproteins; LVMI: left ventricular mass index.
As for subclinical atherosclerosis markers, mean cIMT and LVMI were close to the superior limit, 36%, respectively 45% of participants presenting pathological values. Carotid plaques were found in 48 subjects (23 with unilateral and 25 with bilateral plaques) while aortic atheromatosis was a relatively common feature of the population, detected in more than 70% of cases. ABI and arterial stiffness parameters were in normal ranges, with aPWV mean of 8.28±1.79m/s.
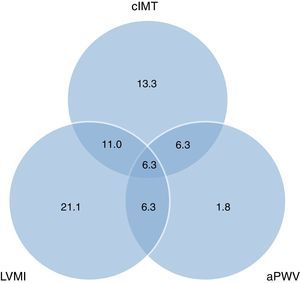
The overlap in the incidence of subclinical CVD and atherosclerosis across 3 different territories (cIMT, LVMI and aPWV) is displayed in the Venn diagram (Fig. 2). Of 120 subjects, 43 (36%) had no evidence of atherosclerosis, 43 (36%) had 1 territory with atherosclerotic involvement, 27 (22%) had 2 territories with atherosclerotic involvement and 7 (6%) had all 3 territories involved.
SCORE determinantsThe study population was further divided into two classes according to the SCORE risk (Table 1). Increased age and blood pressure, male sex, alcohol intake and abdominal obesity only in women were associated with high cardiovascular risk. Smoking habits were better reflected in individuals with increased SCORE risk value (current and former smokers 53.5% vs. 35.8% in the low risk group). Increased plasma glucose and decreased eGFR were associated with high SCORE risk score values. Except for triglycerides, all other lipid parameters were not significantly different between the two groups.
In univariate analysis, high SCORE risk score class individuals presented increased values of cIMT and overall LVMI (p<0.05) but the LVMI significance was lost when divided by gender. In the same subgroup, the carotid and aortic atherosclerotic burden remained high (p<0.0001). There was no difference by groups in regard to ABI. In subjects with high cardiovascular risk, all arterial stiffness markers, especially aPWV had significantly increased values (p<0.0001). A multivariate logistic regression analysis was performed, taking the SCORE categories as the dependent variable and parameters showing significant differences between SCORE categories, in univariate analysis, as independent variables (Table 2). cIMT and aPWV remained independently associated with SCORE risk in the multivariate model. Individuals with cIMT values over 0.9mm have a 4.1 times higher risk for being at high CVD risk according to SCORE chart. Moreover, a 1.4-fold greater risk for having a high SCORE value is present in subjects with an increase of aPWV with 1m/s. The significant relationship between LVMI and aortic atheromatosis was lost in multivariate analysis. The value for the predictive statistical model was 0.713 under receiver operating characteristics (95% CI 0.589–0.838) with specificity of 92.7% and sensitivity of 50%.
Multivariate associates of SCORE risk score.
| Parameter | Odds ratio | 95% CI | p value |
|---|---|---|---|
| cIMTb | 4.140 | 1.422–12.150 | 0.009 |
| aPWVa | 1.412 | 1.017–1.961 | 0.039 |
| LVMIb | 1.268 | 0.442–3.642 | 0.659 |
| Aortic atheromatosisb | 0.000 | 0.000 | 0.998 |
aPWV: aortic pulse wave velocity; cIMT: carotid intima-media thickness; LVMI: left ventricular mass index.
Subclinical CVD was present in 64% of the asymptomatic individuals. However, mean SCORE value was 2.95 and 76% of subjects were classified into the low to intermediate risk class. Except for ABI, SCORE risk positively correlated with cIMT (Pearson's r coefficient=0.57, p<0.0001), the presence of carotid plaques (p<0.0001), aPWV (r=0.41, p<0.0001), LVMI (r=0.29, p=0.001) and aortic atheromatosis (p<0.0001).
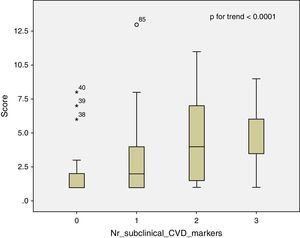
A positive linear relationship was observed between the 3 territories of subclinical CVD (cIMT, LVMI and aPWV) and SCORE risk (p for trend <0.0001). In subjects free of atherosclerotic burden, the 10-year CVD risk was 1.78±1.65. Those who had 1 atherosclerotic marker had a risk of 2.71±2.56, those with 2 markers had a risk of 4.50±3.26, and those with all 3 markers increased had a risk of 5.00±2.58 (Fig. 3). 89% of the subjects with high to very high CVD risk presented markers of atherosclerosis. However, in individuals considered into low to intermediate risk class, 60% had evidence of subclinical CVD (39% in 1, 18% in 2, and 3% in all 3 sites). Moreover, in subjects with low SCORE risk, 23% had increased cIMT, 29.3% had carotid plaques, 14.1% had high aPWV, 46.7% had pathological LVMI, while 62% had aortic atheromatosis.
Validity of subclinical atherosclerosis assessment methods in predicting CVD risk was evaluated by measuring the degree of agreement between subclinical CVD parameters and SCORE risk (low-intermediate and high-very high risk classes). For each of the determined parameters, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and Cohen's kappa coefficient are shown in Table 3. Individually, aortic atherosclerosis presented 100% in sensitivity but 32.9% for PPV. Conversely, ABI had the best PPV (100%) but only 10.7% in sensitivity. aPWV and carotid plaques had good results on specificity and NPV (more than 70%). Overall, cIMT presented the best results in the prediction of SCORE risk with the highest kappa coefficient (0.42).
Characteristics of subclinical CVD in predicting SCORE risk score.
| Parameter | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Kappa coefficient | p value |
|---|---|---|---|---|---|---|
| cIMT | 75 | 75 | 47.7 | 90.8 | 0.42 | <0.0001 |
| Carotid plaques | 75 | 70.7 | 43.8 | 90.3 | 0.37 | 0.0001 |
| aPWV | 35.7 | 85.9 | 43.5 | 81.4 | 0.23 | 0.011 |
| LVMI | 50 | 53.3 | 24.6 | 77.8 | 0.02 | 0.76 |
| Aortic atheromatosis | 100 | 38 | 32.9 | 38 | 0.23 | 0.001 |
| ABI | 10.7 | 100 | 100 | 78.6 | 0.15 | 0.001 |
ABI: ankle-brachial index; aPWV: aortic pulse wave velocity; cIMT: carotid intima-media thickness; CVD: cardiovascular diseases; LVMI: left ventricular mass index; PPV: positive predictive value; NPV: negative predictive value.
By adding cIMT, PWV, SBPao, ABI and LVMI in the PCA comparative to SCORE, the best correlations for SCORE were obtained with cIMT (r=0.57), SBPao (r=0.47) and PWV (r=0.40). The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.74, p<0.0001. Only 2 components were retained for further analysis which accounted for 61.92% of the total variance. The best overall values were obtained for cIMT, PWV and SBPao.
Study limitationsOur study should be interpreted within its limitations. Firstly, the measurements have been performed in a relatively small group of 120 adult participants. Though the subjects have been previously randomized, the results should be mindfully regarded when being extrapolated to the overall population. Secondly, the study design was cross-sectional and the results reflect the CVD abnormalities measured at a specific moment. The absence of independent validation limits the impact of this study. A long-term follow-up of these individuals will show us if the current results remain valid and which non-coronary markers better predict the cardiovascular events.
DiscussionsIn the current study, we have shown that in healthy individuals the SCORE risk score was positively associated with most of the traditional clinical and biochemical risk factors, as well as with different markers of subclinical CVD and atherosclerosis. However, 60% of subjects considered as having low to intermediate SCORE risk presented increased markers of subclinical CVD evaluated by carotid and cardiac ultrasound or arterial stiffness parameters. In contrast, low ABI values were detected only in a minority of the study sample. To our present knowledge, this is the first study that compared the SCORE risk score with multiple methods of determining non-coronary CVD changes by measuring cIMT, aPWV, LVMI, ABI and respectively, carotid and aortic atherosclerosis in a healthy adult population.
In the current CVD prevention guidelines, the strongest recommendations are for performing carotid ultrasound and ABI (class IIa).1,6 Echocardiography is not considered a first line investigation in CVD prevention, but in our study 28% of apparently healthy individuals were newly diagnosed with arterial hypertension and 45% had increased LVMI. Likewise, 20% of subjects had increased arterial stiffness though aPWV has not been yet recommended as method for cardiovascular risk assessment. Measurement of coronary artery calcium (CAC) score by computer tomography is included in the current guidelines1,6 and has been shown to predict mortality and modify the CVD risk prediction.17 However, individuals with low CAC score can still suffer from acute coronary events and it is debatable whether to perform CT imaging for primary prevention in asymptomatic low and intermediate CVD risk individuals due to radiation exposure risk and the considerable impact on the public health costs.18 Based on such considerations and combined with our study results, we consider that carotid and cardiac ultrasound, ABI and arterial stiffness markers represent accessible, reliable and easy to perform methods for a proper cardiovascular risk assessment in asymptomatic population.
cIMT measurement leads to better cardiovascular risk prediction and reclassification in non-high risk subjects.19 In our study, cIMT represented the marker best correlated with SCORE risk and with the powerful risk estimation even after multivariate analysis. In a study by Karim et al., elevated cIMT correlated independently with 10-year CVD risk (p=0.0003) (20) and 69% of individuals classified in the low risk category presented evidence of subclinical atherosclerosis in three different vascular beds (carotid, coronary and aortic) with 8% presenting calcifications in all three. Our results are similar only that we have assessed the carotid, aortic and LV subclinical changes. However, Karim et al. included subjects with increased homocysteine levels which otherwise resembled the baseline population according to the authors and excluded the persons that presented cardiovascular risk factors e.g. hypertriglyceridemia, high blood pressure or chronic alcohol intake. In our study, individuals with risk factors have not been excluded since we consider they are generally met in the population and influence the CVD risk. Bjerrum et al. showed on 277 healthy middle-aged individuals that 56% had signs of coronary or carotid atherosclerosis and the prevalence of subclinical atherosclerosis was 57.5% and above 80% in participants classified as having intermediate and high to very high risk profile according to SCORE risk score.21 Nonetheless, in the same Danish study 12% of subjects were treated for hypercholesterolemia and 18% for hypertension. However, though our results are relatively similar to the presented data, those studies used CAC for the evaluation of coronary atherosclerosis so that the results should be regarded separately.
The occurrence of carotid plaques seems to be variable in the general population. We have reported an overall incidence of 40% with 25% prevalence in individuals with low to intermediate SCORE risk. In subjects aged 50–60 years, 31% had carotid plaques according to Bjerrum et al.21 In a low to intermediate cardiovascular risk sample (SCORE=1.47; cIMT=0.74mm), 25.1% of individuals had carotid atherosclerosis and the prevalence was increasing with higher SCORE values.22 The ultrasound screening for carotid and femoral plaques in low and intermediate risk adults, aged 50–64 years, revealed a prevalence of 32% in women and 40% in men.23 In the CARMELA (Cardiovascular Risk Factor Multiple Evaluation in Latin America) study including more than 11,000 participants, the prevalence of carotid plaques was 8% in different Latin American countries, with an average IMT of 0.65mm.24 Thus, the cIMT values and the presence of plaques are different across regions and might be explained by geographical influence, age and the presence of cardiovascular risk factors.
Arterial stiffness markers predict adverse cardiovascular events in various populations. A recent meta-analysis including more than 17,000 participants concluded stated that aPWV improves the cardiovascular risk prediction with 13% in individuals at intermediate risk.11 Mendonça et al. showed on 800 subjects that aPWV was increased both in individuals with and without coronary artery disease but presenting several cardiovascular risk factors.25 Moreover, in an asymptomatic population with normal cIMT and without carotid plaques, aPWV progressively increased related to the number of risk factors even when adjusted for gender and age.26 One study that included community-based samples of adults with no history of myocardial infarction or stroke has shown that higher aPWV was related to higher CAC (p=0.0003) and lower ABI (p=0.02).27 Thus, increased aPWV was directly and independently associated with greater burden of subclinical CVD in other vascular beds. Our results confirm the significant positive linear correlation between aPWV and SCORE risk and increased aPWV levels are associated with atherosclerotic burden in other territories.
LV hypertrophy is a marker especially used for evaluating the target organ damage in arterial hypertension. In our asymptomatic population, one fourth had high blood pressure and 45% had increased LVMI. Though in univariate analysis, LVMI correlated with SCORE risk, in multivariate logistic regression the significance was lost. Abe et al. showed that 23% of a community-based, multiethnic population had LV hypertrophy.9 The LVMI was increasing as the Framingham score was higher: 23% in the intermediate risk class, respectively 35% in the high risk class. Currently, it is not well defined the approach for normotensive subjects with increased LVMI, 17% in our study, this result being higher than values reported by other authors (under 10%).28 This high prevalence of LV hypertrophy might have different explanations: undiagnosed hypertensive subjects that had normal blood pressure values at the study visit or other non-evaluated factors that might influence the LV mass (increased physical activity levels, presence of obstructive sleep apnea). Aortic atherosclerosis is a relative, visual parameter, not included in the current prevention guidelines. As LVMI, in multivariate logistic regression no positive correlation was obtained with SCORE risk score. However, the presence of aorta calcium determined by computer tomography was independently associated with the 10-year CVD risk score.20
The very low prevalence of pathological ABI (2.5%) in the present study might be explained by the low risk profile of our population as persons with known CVD and diabetes had been excluded. Similar result has been obtained by Bjerrum et al. on a healthy middle-aged sample where only 1% of individuals had an ABI below 0.9.21 Probably, a higher prevalence of asymptomatic lower limb atherosclerosis would have been obtained in our research if imaging or morphological rather than functional methods would have been applied23 as low ABI reflects only hemodynamically significant atherosclerotic lesions.
The findings of the current study present good evidence in favor of a more practical approach in the CVD primary prevention by using different methods for the assessment of subclinical CVD changes. In our asymptomatic population, the SCORE risk score underestimated the cardiovascular risk especially in low to intermediate risk persons where more than a half presented subclinical CVD and atherosclerosis. By determining the CVD changes, the subjects’ risk would be reassessed and early risk reduction therapies could be applied. There might be other risk factors that determine subclinical CVD changes and may be included in the CVD risk algorithms such as family history of CVD, race obesity or inflammatory diseases.20 Nonetheless, the balance cost-benefit for performing investigations in asymptomatic low and intermediate risk subjects should be carefully assessed.29 However, in this risk category, we consider convenient to assess the subclinical CVD abnormalities by at least one method. The criteria for choosing subclinical atherosclerosis tests should take into consideration the predictive value, simplicity, reproducibility, safety and low cost.30 Besides the excellent predictive value of CAC but the modest value for all other criteria, the carotid artery ultrasound and arterial stiffness parameters seem to be the most accurate investigations. As future perspective, ideal risk chart estimation would probably include both general risk factors and easy-determined parameters of subclinical CVD changes.
In conclusion, in an apparently healthy population, SCORE risk score was directly associated with increased markers of subclinical CVD abnormalities. 60% of individuals considered as having low to intermediate SCORE risk presented asymptomatic atherosclerosis and should have been reclassified into higher CVD risk classes. According to our results, cIMT and aPWV represent the parameters that best assess the increased cardiovascular risk and may serve as useful markers to improve cardiovascular risk prediction. Thus, further studies are needed for creating more accurate algorithms in the primary CVD prevention.
Ethical disclosuresProtection of human and animal subjectsThe authors state that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in agreement with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors state that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the correspondence author.
Authors’ contributionsOvidiu Mitu: contributions to the idea and design, collection of data or their analysis and interpretation, writing of the draft of the article, approval of the final version.
Mihai Roca: collection of data or their analysis and interpretation, writing of the draft of the article, approval of the final version.
Mariana Floria: collection of data or their analysis and interpretation, critical review of article contents, approval of the final version.
Antoniu Octavian Petris: collection of data or their analysis and interpretation, critical review of article contents, approval of the final version.
Mariana Graur: contributions to the idea and design, critical review of article contents, approval of the final version.
Florin Mitu: contributions to the idea and design, critical review of article contents, approval of the final version.
Conflict of interestNone declared.
This paper was published under the frame of European Social Found, Human Resources Development Operational Program 2007–2013, project no. POSDRU/159/1.5/136893.
The authors are grateful to Roxana Iacob for carefully reading the article and making valuable suggestions.