The number of splenectomies performed by General Surgery Departments has decreased considerably.1 This is mainly due to 2 reasons: conservative management of patients with blunt abdominal trauma who are hemodynamically stable, and a notable drop in the number of splenectomies performed for hematological diseases (immune thrombocytopenic purpura [ITP], thalassemia, etc.), which are no longer performed because of current medical treatments that are usually effective.1 Therefore, the number of scheduled splenectomies performed is very low, and these are indicated for a varied group of diseases (pseudocysts, neoplasms, splenic artery aneurysms [SAA], failed therapies for hematological disorders, parasitic diseases, etc.) and usually performed using the laparoscopic approach.2–5
The use of the robotic approach has increased exponentially in the field of general surgery.3 However, the number of robotic splenectomies (RS) performed is very small, making it difficult to compare with the laparoscopic approach, which is considered the gold standard.1–4 We present a bi-centric RS experience with a discussion about indications and the results obtained.
We carried out a retrospective, observational, descriptive study of consecutive patients operated on at 2 medical centers. The study was conducted from January 2021-May 2024, following the ethical principles of the Declaration of Helsinki and Good Clinical Practices. The inclusion criteria were patients >18 years of age with any ASA who had undergone RS.
The RS technique was performed using 4 robotic ports (8 mm2 and 12 mm2), placed in a line, as well as an auxiliary infraumbilical trocar when necessary. The table position was: 10 ° anti-Trendelenburg and 3°–5° right lateral decubitus. The robot was positioned at the left of the patient. We collected data for preoperative variables (age, gender, medical history, clinical features, radiological characteristics, size), intraoperative variables (operating time, bleeding, incidents), and postoperative variables (complications measured after 90 days according to the Clavien-Dindo classification, hospital stay, histological study). Major complications were defined as >grade II. Quantitative data were expressed as median and interquartile range, and qualitative data as frequencies or percentages.
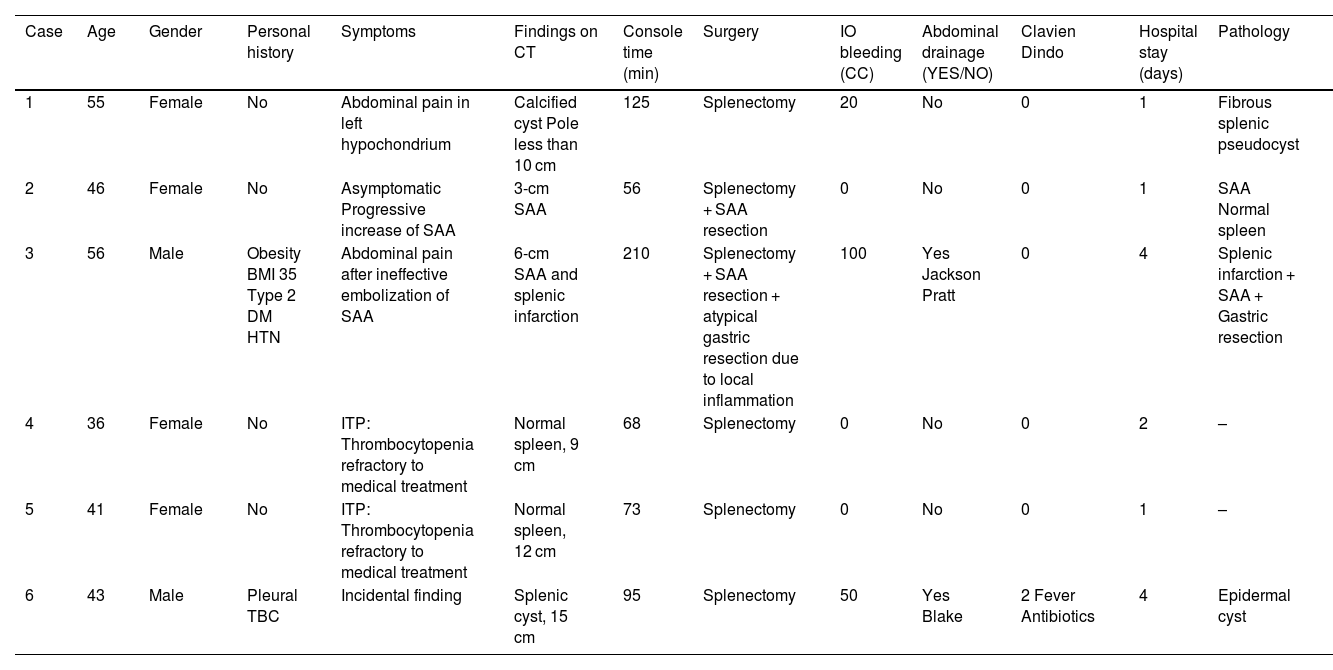
Six robotic procedures were performed. Median age was 44.5 years (IQR: 40–55). The gender distribution was 4 women and 2 men. Two patients presented symptomatic cystic lesions measuring 10 and 14 cm in the hilar region, 2 patients had SAA not resolved by interventional radiology, and 2 had ITP refractory to medical treatment. The median console time was 84 min (IQR: 65–146). Six total splenectomies were performed, associated with atypical gastric resection in one patient with SAA. Surgical blood loss was 10 cc (IQR: 0–63). An abdominal drain was placed on 2 occasions. There were no major complications. One patient had postoperative fever, for which antibiotics were prescribed (Clavien-Dindo II). The hospital stay was 1.5 days (IQR: 1–4). The patients have been asymptomatic at all follow-up appointments (Table 1).
Summary of robotic splenectomies.
| Case | Age | Gender | Personal history | Symptoms | Findings on CT | Console time (min) | Surgery | IO bleeding (CC) | Abdominal drainage (YES/NO) | Clavien Dindo | Hospital stay (days) | Pathology |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 55 | Female | No | Abdominal pain in left hypochondrium | Calcified cyst Pole less than 10 cm | 125 | Splenectomy | 20 | No | 0 | 1 | Fibrous splenic pseudocyst |
| 2 | 46 | Female | No | Asymptomatic Progressive increase of SAA | 3-cm SAA | 56 | Splenectomy + SAA resection | 0 | No | 0 | 1 | SAA Normal spleen |
| 3 | 56 | Male | Obesity BMI 35 Type 2 DM HTN | Abdominal pain after ineffective embolization of SAA | 6-cm SAA and splenic infarction | 210 | Splenectomy + SAA resection + atypical gastric resection due to local inflammation | 100 | Yes Jackson Pratt | 0 | 4 | Splenic infarction + SAA + Gastric resection |
| 4 | 36 | Female | No | ITP: Thrombocytopenia refractory to medical treatment | Normal spleen, 9 cm | 68 | Splenectomy | 0 | No | 0 | 2 | – |
| 5 | 41 | Female | No | ITP: Thrombocytopenia refractory to medical treatment | Normal spleen, 12 cm | 73 | Splenectomy | 0 | No | 0 | 1 | – |
| 6 | 43 | Male | Pleural TBC | Incidental finding | Splenic cyst, 15 cm | 95 | Splenectomy | 50 | Yes Blake | 2 Fever Antibiotics | 4 | Epidermal cyst |
We have presented a series of 6 RS performed at 2 medical centers for different pathologies: splenic cysts, SAA and ITP. The results obtained are optimal, with a shorter surgical time, minimal operative bleeding, no major complications, short hospital stay and complete clinical resolution.
We will briefly summarize the splenic diseases for which we indicate RS. There is a very small number of published cases of RS for these diseases.
- •
Splenic cysts are an extremely rare pathology (0.07% of the population).6 The most common symptom is abdominal pain in the left hypochondrium, as in our 2 patients.7 Cysts >5 cm should be treated due to the risk of infection, bleeding or rupture.7 Total splenectomy is indicated in giant cysts (>10 cm) or if they are located in the hilar region, as in the cases presented. The remaining patients can be treated by fenestration or partial splenectomy.8
- •
SAA is the most frequent visceral aneurysm and should be treated if >2 cm and in pregnant women or symptomatic patients.9 The endovascular approach is the most commonly used, but if symptoms do not persist or the size increases, it should be treated surgically.9
- •
ITP is a hematological disease that causes thrombocytopenia. Historically, symptomatic patients who did not respond to corticosteroids were treated by splenectomy.1 The emergence of multiple drugs in the last decade has reduced the surgical indication to only refractory cases, like the 2 we have presented.
In recent years, advances in robotic surgery have contributed to its indication in an increasing number of abdominal pathologies.3 The robotic approach allows for better visualization, less tremor, and increased maneuverability during dissection, and perhaps the only drawback is higher costs.2.3,5,6,10 Few articles have been published about RS (6 manuscripts including 140 patients), but they have described how RS is associated with fewer postoperative complications, lower conversion rate, shorter hospital stay and less blood loss versus the laparoscopic approach.3,4,10 RS seems especially recommended in more difficult splenectomies (partial splenectomy, patients with cirrhosis, splenic tumors, malignant blood disease).2 Critics of the robotic approach cite that it is not cost-effective (a fact that will gradually improve) and it involves a longer operating time; however, as our cases demonstrate, the surgical times are similar to those of laparoscopic surgery.3,5,10
In conclusion, and despite the limitation of presenting a small case series, we believe that RS is a safe and reliable technique that will probably replace the laparoscopic approach in coming years due to the technical benefits it provides.
Conflict of interestThe authors declare that they have no conflicts of interest.