Pulmonary sequestration (PS) is a rare congenital malformation characterized by nonfunctional lung parenchyma isolated from the normal tracheobronchial tree that receives aberrant blood supply from the systemic arteries.1 Intralobar sequestrations (ILS) are the more common type,2 in which the abnormal tissue is embedded within the visceral pleura of the normal lung. Superimposed aspergillus fungal infections have rarely been reported in ILS, consisting of 39 isolated case reports.3 Surgical resection of the sequestrated lung and shutting off aberrant arteries is the standard treatment.4 Resection typically consisted of lobectomy. However, sublobar resection may be preferable since parenchymal preservation is desirable. Here, we report the first case described in the literature of an ILS complicated with aspergilloma, which was successfully resected by robot-assisted segmentectomy using fluorescence image guided by indocyanine green (ICG).
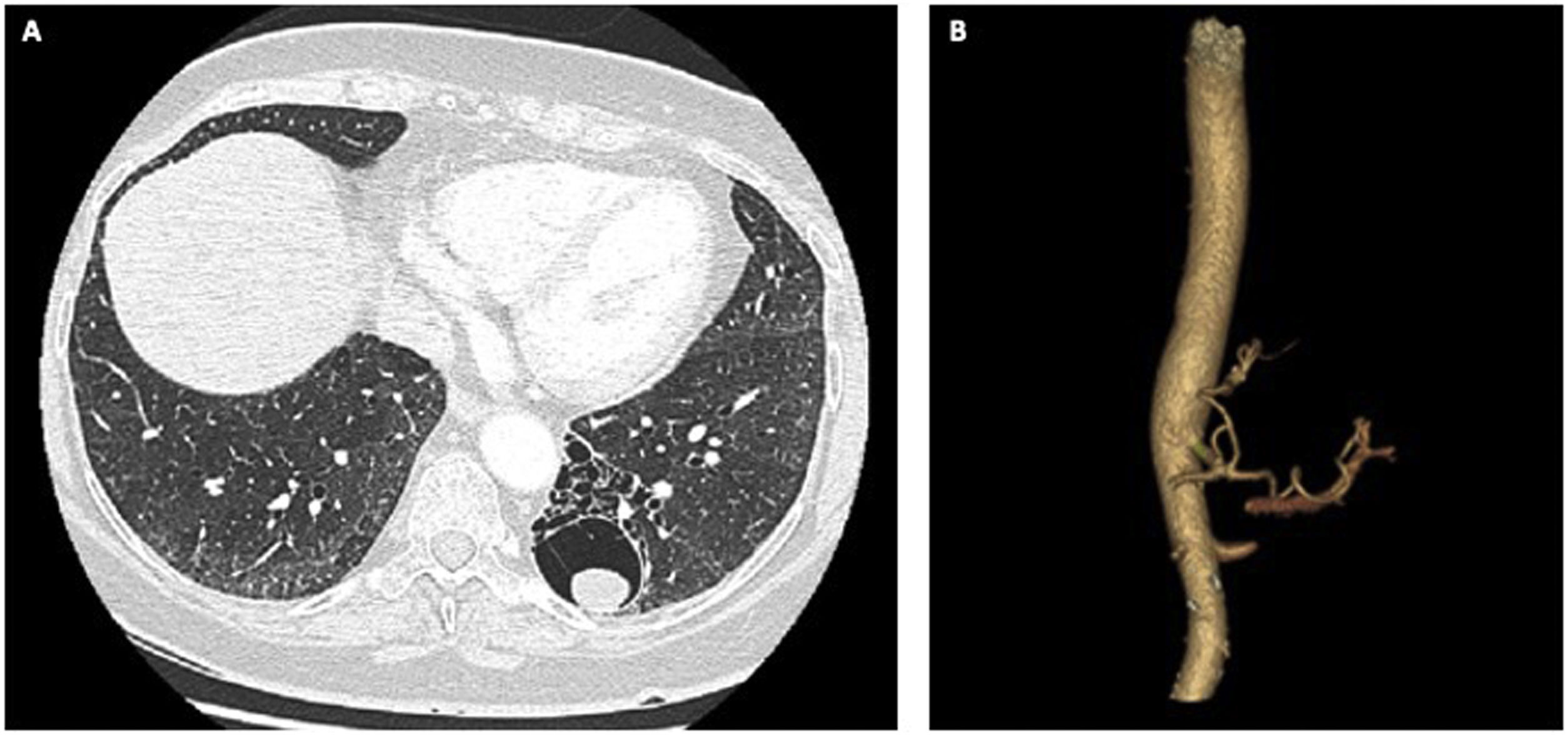
A 63-year-old woman with no relevant medical history had been incidentally diagnosed with left lower lobe ILS 10 years earlier, which was managed conservatively since she was asymptomatic. In recent years, symptoms had begun to manifest, and she had several episodes of pneumonia and expectoration with haemoptysis. Chest computed tomography demonstrated a cystic lesion with a 2.2-cm mobile, nodular content at the base of the left lower lobe, compatible with ILS complicated with mycetoma (Fig. 1A). Systemic blood supply was provided by the splenic artery (Fig. 1B). Bronchoscopy was performed, and microbiological cultures of the bronchial suction sample showed evidence of Aspergillus fumigatus. Pulmonary function tests were within normal ranges (FEV1%: 105%, and DLCO%: 96%). Therefore, the patient was diagnosed with ILS complicated with aspergilloma, treated with voriconazole and scheduled for robotic resection of the pulmonary sequestration.
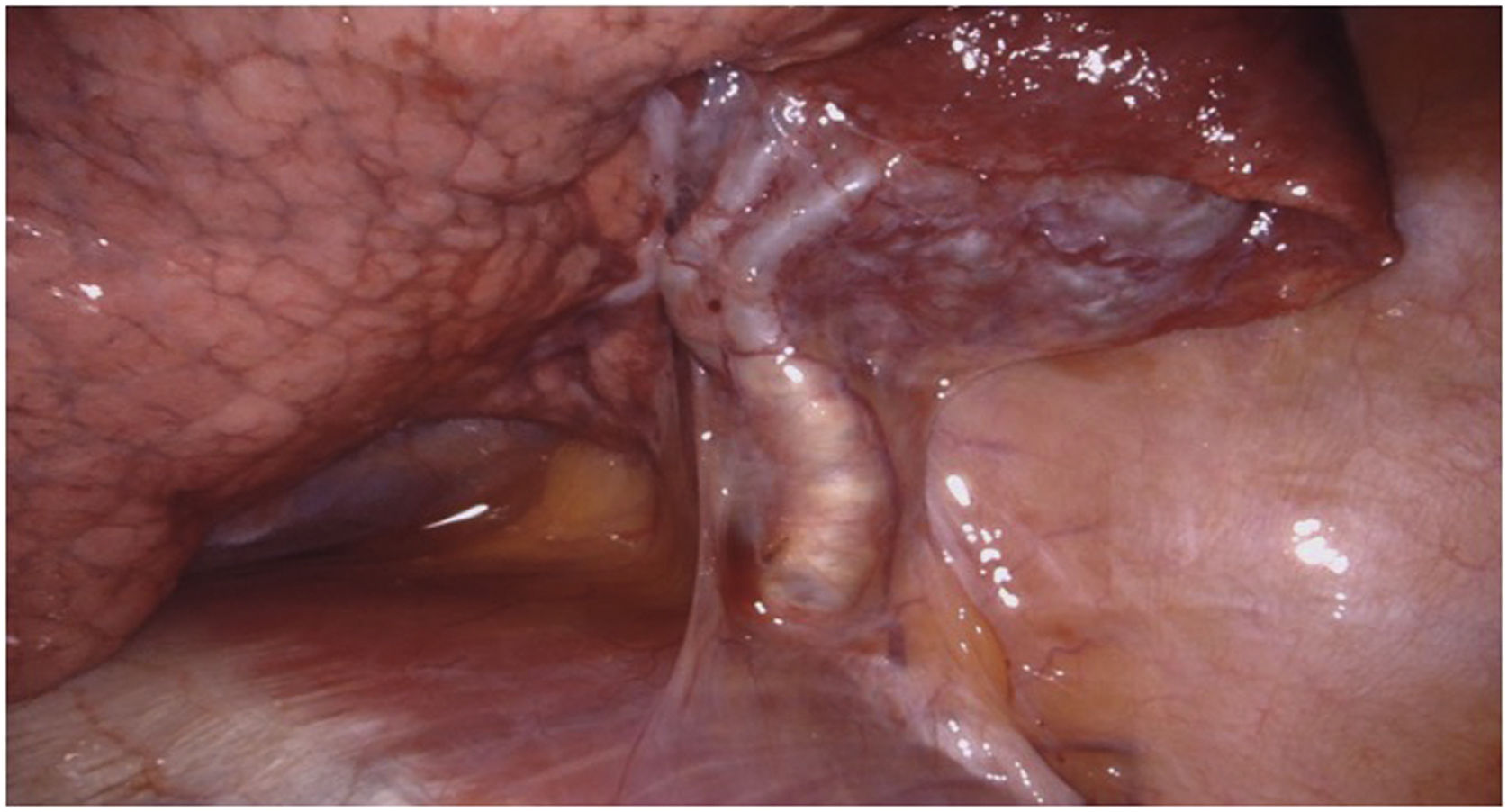
A 4-arm technique with one additional assistant port was used with the da Vinci X surgical system (Intuitive, Sunnyvale, CA, USA). The camera port was situated in the eighth intercostal space. No significant pleural adhesions were found. A systemic arterial branch to the sequestration originating below the diaphragm was first isolated (Fig. 2) and divided with a robotic stapler (white cartridge, 2.5-mm staple height). Venous drainage of the sequestration was diminutive, and therefore Maryland bipolar coagulation forceps were used. There was no other vascular or bronchial abnormality. Thirteen milligrams of ICG (0.15 mg/kg) were injected intravenously after ligation of the arterial blood supply, permitting demarcation of the sequestration from the normal lung. The boundary around the sequestration was marked with electrocautery. However, the sequestrated parenchyma was quite extensive and central, and left lower lobe basilar segmentectomy was therefore performed to ensure complete resection of the abnormal tissue. ICG was administered again to define the borderline between the segment 6 and basilar segments. Parenchymal transection was then performed with robotic staples (blue and green cartridges, 3.5-mm and 4.3-mm staple heights, respectively). The specimen was removed with a polytetrafluoroethylene bag.
Pathology confirmed the diagnosis of aspergilloma within ILS. The postoperative period was uneventful, and the patient was discharged home on postoperative day 2 after chest tube removal.
PS is a relatively unusual condition comprising 0.15–6.4% of congenital lung malformations.5 Superinfections of PS by fungal pathogens are extremely rare. Some authors support the hypothesis that some ILS may be acquired lesions associated with chronic infection, such as aspergillosis, instead of congenital abnormalities related to anomalous lung development.6 In the current case, the patient was diagnosed with ILS several years before developing the fungal infection. We hypothesize that pulmonary aspergilloma developed in preexisting cavities formed by underlying pulmonary lesions. The occurrence of a fungal mycetoma within ILS indicates that the ILS must have communications with the tracheobronchial tree.
Surgical resection is considered the optimal treatment for both PS and aspergilloma in order to prevent life-threatening symptoms.4,7 Although ILS have been classically treated with lobectomy,2 successful cases of sublobar resections, including wedge resection and segmentectomy, have been reported for localized ILS.3,8 We believe that sublobar resection should be preferred when the sequestration is limited to a segment, since it allows for complete removal of the benign lesion and limits the loss of normal-functioning lung. Whether patients with pulmonary aspergillomas should receive lobectomy or sublobectomy is also debatable. A retrospective research study revealed that sublobar resections were recommended for small, peripheral, and simple pulmonary aspergillomas (<3 cm) to preserve lung function and enhance recovery.9 These procedures are usually technically demanding, mainly due to difficult operating conditions, including massive pleural adhesions or damaged lung parenchyma.
Robotic-assisted resection of ILS has been recently reported,8,10 while minimally invasive surgery has been described in selected cases of pulmonary aspergilloma.7 The robotic approach offers the advantages of minimally invasive surgery, superior visualization in the 3-dimensional view setting, higher instrument precision with 7 degrees of motion resulting in improved dexterity and fluorescence imaging vision. These advantages are particularly useful during anatomical pulmonary segmentectomy, which requires meticulous intraparenchymal dissection and precise delimitation of the intersegmental plane, and also in ILS, where identification of aberrant arteries and demarcation of the sequestration margin is crucial for resection.
This case demonstrates that the robotic approach with fluorescence image guidance can be helpful for sublobar resection of ILS complicated with aspergilloma.
Funding statementThe authors declare that no financial support was received regarding the content of this manuscript.
Conflict of interestThe authors declare that there is no conflict of interest regarding the content of this manuscript.