Endometriosis is one of the most frequent gynecological pathologies in women of reproductive age. It is characterized by the presence of epithelium and stromal cells in extrauterine locations.1,2 Its prevalence is 10%–15%, and the average age is 30 years. Symptoms include chronic pain and infertility. The most frequent pelvic locations are the ovaries and the pelvic peritoneum.1–4 A rare form is endometriosis of the abdominal wall, which is most frequently found in patients with previous gynecological surgeries. The risk of malignant disease is very rare, and the most frequent variant is clear-cell adenocarcinoma.5,6
We present 2 cases derived from foci of endometriosis.Case 1 The patient is a 54-year-old woman with a history of lymphoma in remission. She had undergone 2 cesarean sections, the last one 21 years earlier. Presently, she consulted for a mass in the abdominal wall. On examination, an immobile mass was palpable in the region of the cesarean section scar.
CT scan revealed a 46-mm mass with heterogeneous uptake (Fig. 1), with no plane of separation from the abdominal wall.
Core-needle biopsy was performed, and the results identified adenocarcinoma of possible Müllerian origin (ovarian serous).
The surgical procedure included en bloc excision of the tumor preserving the peritoneum and including skin, fascia, and muscles. Free margins were confirmed intraoperatively. Subsequently, the gynecology team performed a hysterectomy with double adnexectomy. The peritoneum was closed with 2/0 poly(4-hydroxybutyrate) suture. Bilateral TAR was performed, placing a 20 × 20 cm double-layered polypropylene and PVDF mesh in the preperitoneal position. A 15 × 15 cm PLP inlay mesh was placed and affixed with continuous absorbable 2/0 suture to the anterior sheath of the rectus and the greater oblique muscles.
During the postoperative period, the patient presented no complications and was discharged after 4 days.
The pathology study of the surgical piece reported grade III clear-cell carcinoma. Adjuvant chemotherapy with carboplatin and paclitaxel was administered for 6 cycles.
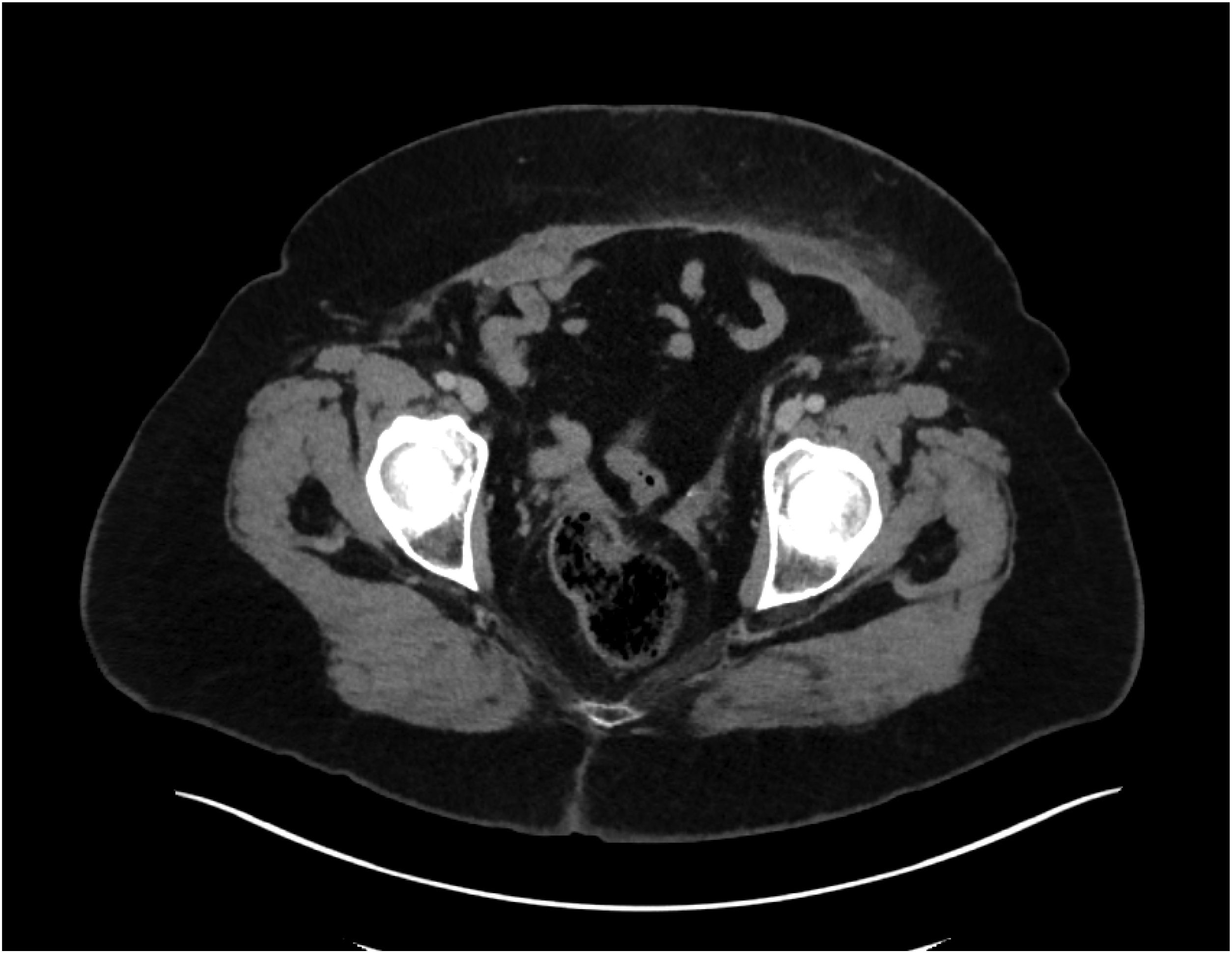
The 6-month follow-up CT scan described post-surgical changes in the hypogastrium and RIF (Fig. 2). At the one-year follow-up, the patient remains in remission.Case 2 The patient is a 51-year-old woman who underwent a cesarean section 25 years earlier, with no other history of interest. Presently, she consulted for a painful mass in the abdominal wall. On examination, an indurated nodule was palpated in the hypogastrium, which could not be reduced and was painful.
CT scan demonstrated a tumor with a solid appearance and heterogeneous density located in the left anterior rectus muscle measuring 4.8 × 2.9 × 4.6 cm. The findings were compatible with desmoid tumor, fibromatosis, endometrioma, sarcoma, etc.
We performed surgery for the abdominal wall mass, using a surgical technique similar to the aforementioned case. The pathology study reported immunohistochemical findings of Müllerian origin of the neoplasm and a histology of clear-cell carcinoma. Given these results, the case was presented to the multidisciplinary team, who decided that the surgery should be completed with total hysterectomy and bilateral adnexectomy. This was followed by chemotherapy with carboplatin and paclitaxel for 6 cycles.
The patient remains under follow-up in the outpatient oncology consultations, and 2 years after the intervention she remains in remission.
Endometriosis is a benign disease with an unpredictable evolution that can infiltrate and spread to other structures.
Surgical scars are a good substrate for the implantation of endometriosis foci. As indicated by Mara et al, less than 1% of these foci will develop cancer. Yoahua et al indicate that hyperestrogenism is one of the main risk factors. The CD10 and P53 markers are important, having high sensitivity and specificity for extragonadal endometriosis and endometriosis-associated cancer, respectively.3 The most frequent variant in wall tumors secondary to endometriosis is clear-cell tumors, as observed in the 2 cases described.
The interval between the first surgery and the diagnosis of carcinoma is about 20 years. Diagnoses are usually made when the patient consults for a palpable lesion in the abdomen as well as abdominal pain associated with menstruation. It is essential to use imaging studies for diagnosis (ultrasound, MRI, or CT) to define not only its size but also its relationship with neighboring structures and its resectability. Core-needle biopsy is the most cost-effective means for the initial diagnosis.3,5
The most widespread therapeutic strategy is resection of the tumor with hysterectomy and double adnexectomy.
Prognostic factors have not yet been determined due to the small number of cases, but it seems that a size greater than 5 cm, affected lymph nodes, or positive resection margins are associated with lower survival.4 The article by Taburaix et al has reported a median survival of 30 months. The behavior of recurrences and/or metastases is also unknown, although the most frequent site is the inguinal lymph nodes.7
Abdominal wall endometriosis is a frequently benign pathology that can sometimes become malignant, and the histological type is usually an endometrial carcinoma. In these cases, as in our patients, the histological variant is clear-cell carcinoma, which is extremely rare. Complete excision with negative margins is the objective for treatment, although this may require complex reconstructions of the abdominal wall associated with hysterectomy and adjuvant treatment.