Liver resection is the only potentially curative treatment for most malignant liver tumors.1,2 Traditionally, tumors that compromised portal or hepatocaval confluence vessels were considered unresectable. The objective of our study is to evaluate the surgical results and applicability of the techniques used in hepatic resection of tumors with compromised venous vasculature.
We present a retrospective, descriptive study of patients who had undergone liver resection for malignant tumors with venous vascular compromise during the period between January 2015 and December 2022. Perioperative variables were analyzed.
We define venous vascular invasion as tumor infiltration of the vena cava, main trunks of the portal vein and/or hepatic veins, which requires resection and vascular reconstruction techniques to achieve a complete resection of the lesion.
Triphasic computed tomography and/or magnetic resonance imaging were used to determine tumor involvement, resectability and the presence of extrahepatic disease.
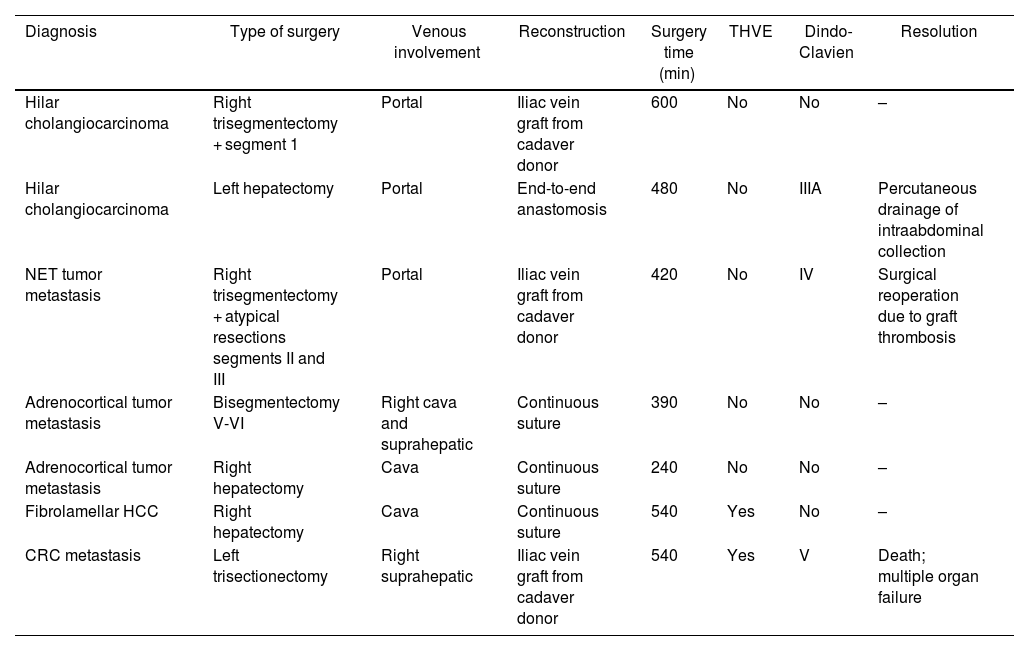
In this period, 270 liver resections were performed, 7 of which (2.6%) were associated with vein resections. Median age was 46 years (range, 27–66). The data on etiology, types of surgery, vascular compromise, vascular reconstruction, surgical times and complications are found in Table 1. Intraoperative ultrasound was used to map the lesions and their relationship with the vascular structures. Transection of the liver parenchyma was performed with a harmonic scalpel, ultrasonic aspirator or a combination of both. Total vascular exclusion times were ≤40 min. The patients were routinely evaluated using doppler ultrasound in the immediate postoperative period and then daily during the first 72 h. The average consumption of blood products was 3 units (range, 1–8). The median length of stay in the intensive care unit was 8 days (range, 3–18) and mean hospitalization stay was 20 days (range, 5–48). Morbidity was 42.8% (all major complications, Dindo-Clavien >3) and mortality 14.3%. The median follow-up was 186 days (range, 10–336).
Surgical results.
| Diagnosis | Type of surgery | Venous involvement | Reconstruction | Surgery time (min) | THVE | Dindo-Clavien | Resolution |
|---|---|---|---|---|---|---|---|
| Hilar cholangiocarcinoma | Right trisegmentectomy + segment 1 | Portal | Iliac vein graft from cadaver donor | 600 | No | No | – |
| Hilar cholangiocarcinoma | Left hepatectomy | Portal | End-to-end anastomosis | 480 | No | IIIA | Percutaneous drainage of intraabdominal collection |
| NET tumor metastasis | Right trisegmentectomy + atypical resections segments II and III | Portal | Iliac vein graft from cadaver donor | 420 | No | IV | Surgical reoperation due to graft thrombosis |
| Adrenocortical tumor metastasis | Bisegmentectomy V-VI | Right cava and suprahepatic | Continuous suture | 390 | No | No | – |
| Adrenocortical tumor metastasis | Right hepatectomy | Cava | Continuous suture | 240 | No | No | – |
| Fibrolamellar HCC | Right hepatectomy | Cava | Continuous suture | 540 | Yes | No | – |
| CRC metastasis | Left trisectionectomy | Right suprahepatic | Iliac vein graft from cadaver donor | 540 | Yes | V | Death; multiple organ failure |
NET: neuroendocrine tumor; CRC: colorectal cancer; THVE: total hepatic vascular exclusion; HCC: hepatocellular carcinoma.
Liver tumors involving the hepatocaval confluence were considered an absolute contraindication for liver resection.3,4 Reconstruction of the hepatic veins depends on the size and location of the defect. In some cases, tangential resection and reconstruction can done with autologous vein grafts (Fig. 1A), bovine pericardium or polytetrafluoroethylene (PTFE) stents. If the resection is short and close to the opening in the vena cava, it can be reinserted directly. However, if the distance is greater, interposition may be necessary, such as in portal vein resection techniques.
A) Reconstruction of the right hepatic vein using a cadaver donor iliac vein graft (white arrow: yellow vessel loop surrounding common trunk of the MHC and the LHV, occluded by a Satinsky clamp; white pentagon: Pringle maneuver); B) Reconstruction of the right portal vein (white arrow) with iliac vein graft from a deceased donor. A previously placed percutaneous biliary drain tube is also observed entering the right posterior sectoral duct (white pentagon).
The technical difficulty of resecting the inferior vena cava depends on the location of the compromise. If the invasion is found below the confluence of the hepatic veins, direct clamping can be performed without significant circulatory instability. Small defects can be sutured tangentially.
The resection of tumors close to the opening of the hepatic veins represents a major technical challenge that requires adequate vascular control. Total vascular exclusion implies the complete occlusion of the flow to and from the liver, isolating it completely from the systemic circulation. Most studies report a total vascular exclusion time of 45−60 min without significant deterioration in liver function.5 In cases requiring longer times, hypothermic portal perfusion is recommended.
Portal vein resection is a standard procedure, especially in Klatskin tumors. Radical surgical resection with negative margins is a treatment option that has demonstrated a 5-year survival rate of 41%.6 Portal vein reconstructions can be performed via end-to-end anastomosis. When this is not possible because the gap requiring reconstruction is larger, autologous or heterologous vein grafts or PTFE stents can be used. In our cases, iliac vein grafts from cadaver donors were preferred due to their availability (Fig. 1B). Their advantages over stents include lower rates of infection and thrombosis, greater durability and permeability.7
The anastomosis between the main trunk of the portal vein and its left branch can be technically difficult due to the difference in calibers. It is important to ensure the correct position and length of both ends to avoid rotation and posterior thrombosis. In our case, a two-stage hepatectomy was performed in a patient with a Klatskin tumor (Bismuth IIIa). In the first stage, right portal embolization was performed; 25 days later, and after having certified adequate hypertrophy through volumetry, a right trisectionectomy including segment I was performed. Reconstruction between the main trunk and the left branch of the portal vein was carried out using an end-to-end anastomosis with monofilament surget suture.
In cases of tangential resections, the defect is usually closed with direct suture transverse to the axis of the vessel to avoid stenosis or using vein patches.
In conclusion, hepatectomy associated with venous vascular resection in patients with malignant liver tumors is a feasible procedure, although it entails high morbidity and mortality.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ruiz NS, Mollard L, Chahdi Beltrame M, Lenz Virreira ME, Quiñonez EG. Resección de tumores hepáticos con infiltracion vascular venosa: técnicas y resultados. Cir Esp. 2024;102:122–124.