Extended thromboprophylaxis with low-molecular-weight heparin (LMWH) for 28 days is recommended in patients undergoing major abdominal or pelvic cancer surgery, but the evidence for thoracic cancer surgery is weak. We aimed to evaluate the use of pharmacological thromboprophylaxis and incidence of venous thromboembolism (VTE) in adult patients undergoing lung cancer surgery in daily clinical practice.
MethodsRetrospective evaluation of a cohort of consecutive adult patients who had undergone lung cancer surgery. Patients were followed for 90 days after surgery.
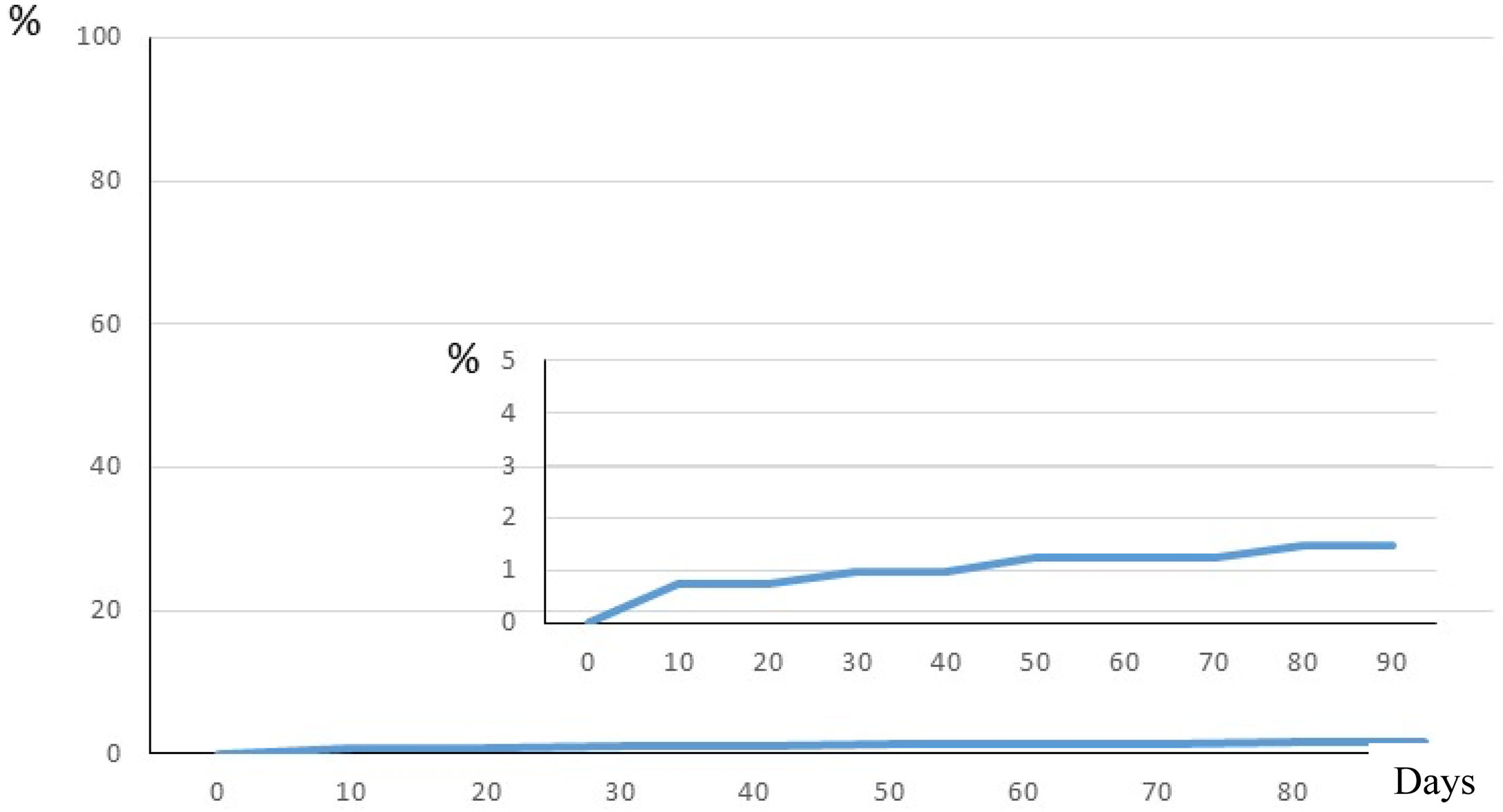
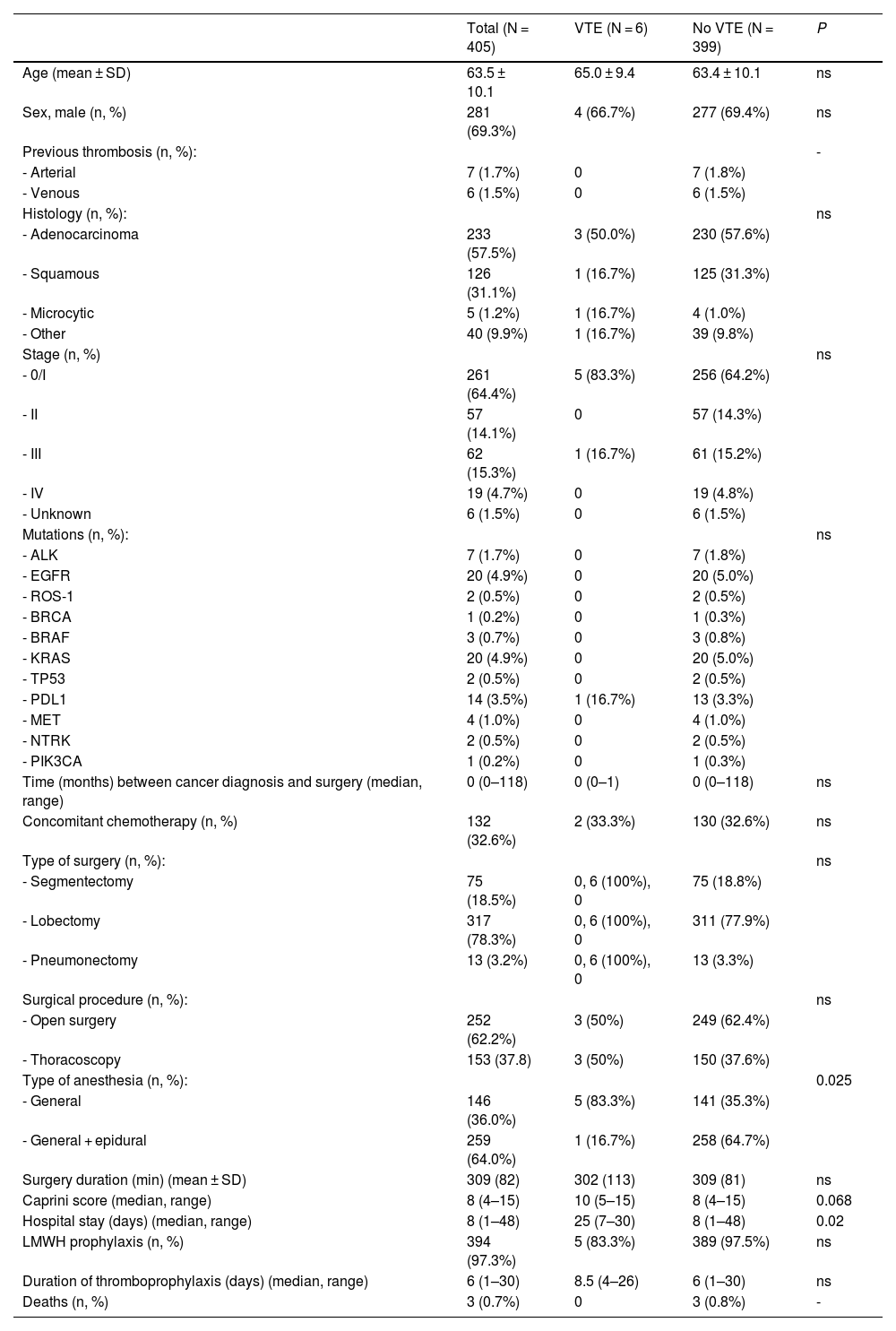
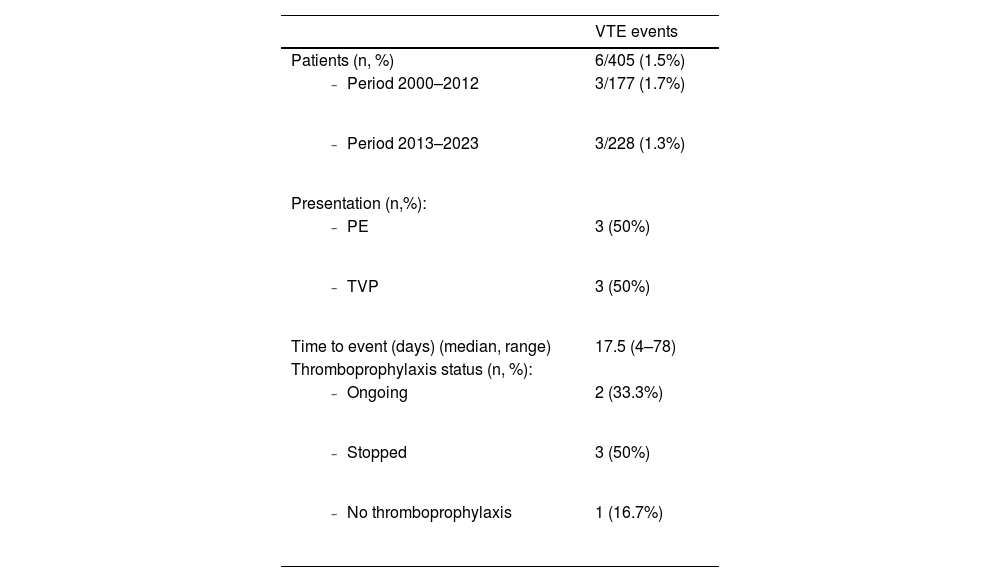
ResultsFrom 2000 to 2023, 405 patients were included (69% males; mean age 63.5 ± 10.1 years). Overall, 97.3% of the patients received LMWH thromboprophylaxis, with a median duration of 6 days (range, 1–30 days). Thromboprophylaxis use increased over time (from 94.9% in the period 2000–2012 to 99.1% in the period 2013–2023). During follow-up, 6 patients (1.5%) developed a VTE event: 3 isolated lower-limb deep vein thrombosis, and 3 non-fatal pulmonary embolism. Median time between surgery and the thrombotic event was 17.5 days (range, 4–78 days). Concomitant epidural analgesia and shorter hospital stay were associated with a lower risk of VTE. Three patients (0.7%) died during follow-up, none of them due to a VTE event.
ConclusionsWhile extended thromboprophylaxis could be considered for certain high-risk thoracic surgery cancer patients, our results do not support its widespread use due to the low rate of VTE after lung cancer surgery. More studies are needed to identify subgroups of patients that could benefit from tailored thromboprophylaxis strategies.
La trombropofilaxis extendida con heparina de bajo peso molecular (HBPM) durante 28 días está recomendada en cirugía oncológica mayor abdominal o pélvica. La evidencia en cirugía oncológica torácica es débil. Hemos evaluado el uso de tromboprofilaxis farmacológica y la incidencia de tromboembolismo venoso (TEV) en condiciones de práctica clínica habitual en pacientes intervenidos por cáncer de pulmón.
MétodosEstudio retrospectivo unicéntrico de pacientes adultos consecutivos intervenidos por cáncer de pulmón, seguidos durante 90 días tras la cirugía.
ResultadosEntre 2000 y 2023 se incluyeron 405 pacientes (69% varones; edad media 63,5 ± 10,1 años). Globalmente, el 97,3% de los pacientes recibieron tromboprofilaxis con HBPM, con una mediana de duración de 6 días (rango, 1-30 días). El uso de la tromboprofilaxis aumentó a lo largo del tiempo (de 94,9% en el periodo 2000-2012 a 99,1% en el periodo 2013-2023). Durante el seguimiento 6 pacientes (1,5%) desarrollaron un episodio de TEV, 3 trombosis venosas profundas aisladas de extremidades inferiores y 3 embolias de pulmón no fatales. La mediana de tiempo entre la cirugía y el evento trombótico fue 17,5 días (rango, 4-78 días). El empleo de anestesia epidural y la menor estancia hospitalaria se asociaron con un menor riesgo de TEV. Durante el seguimiento fallecieron 3 pacientes (0,7%), ninguno de ellos como consecuencia de una complicación trombótica.
ConclusionesNuestros resultados no apoyan el empleo sistemático de la tromboprofilaxis farmacológica extendida tras cirugía por cáncer de pulmón. Se precisan estudios adicionales para identificar subgrupos de pacientes que se beneficiarían de estrategias de tromboprofilaxis individualizadas.