The Spanish Association of Surgeons (AEC) deems it essential to define and regulate the acquisition of high-specialization competencies within General Surgery and Gastrointestinal Surgery and proposes the Regulation for the accreditation of specialized surgical units. The AEC aims to define specialized surgical units as those functional elements of the health system that meet the defined requirements regarding their provision, solvency, and specialization in care, teaching, and research. In this paper we present the proposed accreditation model for Abdominal Wall Surgery Units, as well as the results of a survey conducted to assess the status of such units in our country. The model presented represents one of the pioneering initiatives worldwide concerning the accreditation of Abdominal Wall Surgery Units.
La Asociación Española de Cirujanos (AEC) considera imprescindible definir y regular la adquisición de competencias de alta especialización dentro de la Cirugía General y del Aparato Digestivo y propone la Normativa de acreditación de unidades quirúrgicas especializadas. El objetivo de la AEC es definir las unidades quirúrgicas especializadas como aquellos elementos del sistema sanitario, de carácter funcional, que cumplan los requisitos definidos sobre su prestación, solvencia, especialización asistencial, docente e investigadora. En el presente trabajo se presenta el modelo de acreditación propuesto para las Unidades de Cirugía de la Pared Abdominal, así como los resultados de una encuesta realizada para conocer la situación de dichas unidades en nuestro país. El modelo presentado representa una de las iniciativas pioneras a nivel mundial en referencia a la acreditación de Unidades de Cirugía de la Pared Abdominal.
In recent years Abdominal Wall Surgery (AWS) has seen exponential growth in terms of understanding the risk factors associated with the occurrence of a hernia,1–3 preoperative care (i.e., prehabilitation),4,5 intraoperative care (enhanced description and comprehension of surgical anatomy, incorporation of new surgical techniques, improvements in prosthetic materials, addition of robotic surgery)6–9 and postoperative care.10,11 In the previous context, there has been a parallel increase in surgeons' interest in understanding the practice and complexity of AWS.12 Recently, the European Union of Medical Specialists (UEMS) has recognized AWS as a specific working group by creating the "European Board of Abdominal Wall Surgery" (EBAWS)13. Moreover, the claim for the need to identify “AWS Units” is not new.14 In fact, the European Hernia Society (EHS) has formulated some accreditation and certification requirements for such "Units"15 which have contributed to specific pioneering proposals in some countries in our environment.16,17 Given the above and considering the wide spectrum of difficulty in AWS (from less complex to the most complex cases), the knowledge required to perform it (surgical anatomy, risk factors, surgical techniques, prosthetic materials, postoperative care) and the minimum facilities necessary for its practice, regulation from scientific societies first and from health policies second, is necessary regarding the "capabilities" of different centers to carry out this specific type of surgery, both in terms of human resources and infrastructure. A first step in this "regulation" is the establishment of criteria by scientific societies for the "accreditation" of these Abdominal Wall Surgery Units. From the Spanish Association of Surgeons (AEC), concern for meeting quality standards within a clinical, educational, and research framework has driven the development of the necessary criteria for the accreditation of units in different training areas of General and Digestive Surgery, including Abdominal Wall Surgery.18,19
The primary objective of this work is to present the accreditation model for Abdominal Wall Units in our country approved by the AEC. The secondary objective is to gather information through an online survey among members of the AEC's abdominal wall section on their potential involvement and healthcare activity in Abdominal Wall Units in Spain.
Material and methodAccreditationIn Spain, the Cohesion and Quality Law of the National Health System (16/2003, of May 28), provides for the existence of reference services for the care of pathologies that require high professional specialization or complex technology. Also, when the number of cases to be treated is not high and the concentration of diagnostic and therapeutic resources may be advisable.
In accordance with current legislation and through its Executive Board and Scientific Committee, the AEC has decided to launch (in several phases) the accreditation process for Units in different training areas, creating a general regulation with minimum criteria and specific regulation with concrete criteria that will vary depending on the training area of the unit to be accredited.19
The organizational structure of the AEC is divided into sections, based on specific training areas. Each section has its board composed of a coordinator, a secretary, and members. The AEC's scientific committee, in collaborative work with the members of each board section, designed the minimum and specific criteria for the accreditation of units.19 For the accreditation of Abdominal Wall Surgery Units, the following criteria were established:
Minimum criteria:
Recognition of the Unit by the Health Care Center, specifying its service portfolio.
Accreditation of the availability of a specific operating room.
Accreditation of a minimum composition of specialist doctors with exclusive dedication to the corresponding area.
4. Commitment to include cases in a specific database or registry for a period not less than 1 year from the application.
Specific criteria:
- 1
Criteria in the care area:
- 2)
Human and material resources (minimum composition of surgeons with specific dedication to the abdominal wall and specific and regular operating rooms for abdominal wall surgery).
- 3)
b) Quality (commitment to include cases in a registry, specific treatment protocols according to available evidence).
- 4)
Care activity and outcomes.
- 5)
Service portfolio.
- 6)
Activity report.
- 7
Criteria in the research area.
- 8
Criteria in the teaching area.
The accreditation committee that evaluates the minimum and specific requirements is designated by prior agreement of the board of the section interested in developing the accredited unit and the AEC's Scientific Committee.
QuestionnaireBefore designing the specific accreditation criteria for the Abdominal Wall Units, the abdominal wall section of the AEC conducted an online survey using "Google Forms" (https://docs.google.com/forms). Google Forms is a survey management software that is included as part of the free web-based "Google Docs Editors" suite offered by Google.
The survey was designed and evaluated by 2 surgeons with exclusive dedication to abdominal wall surgery (MLC and JAPR).
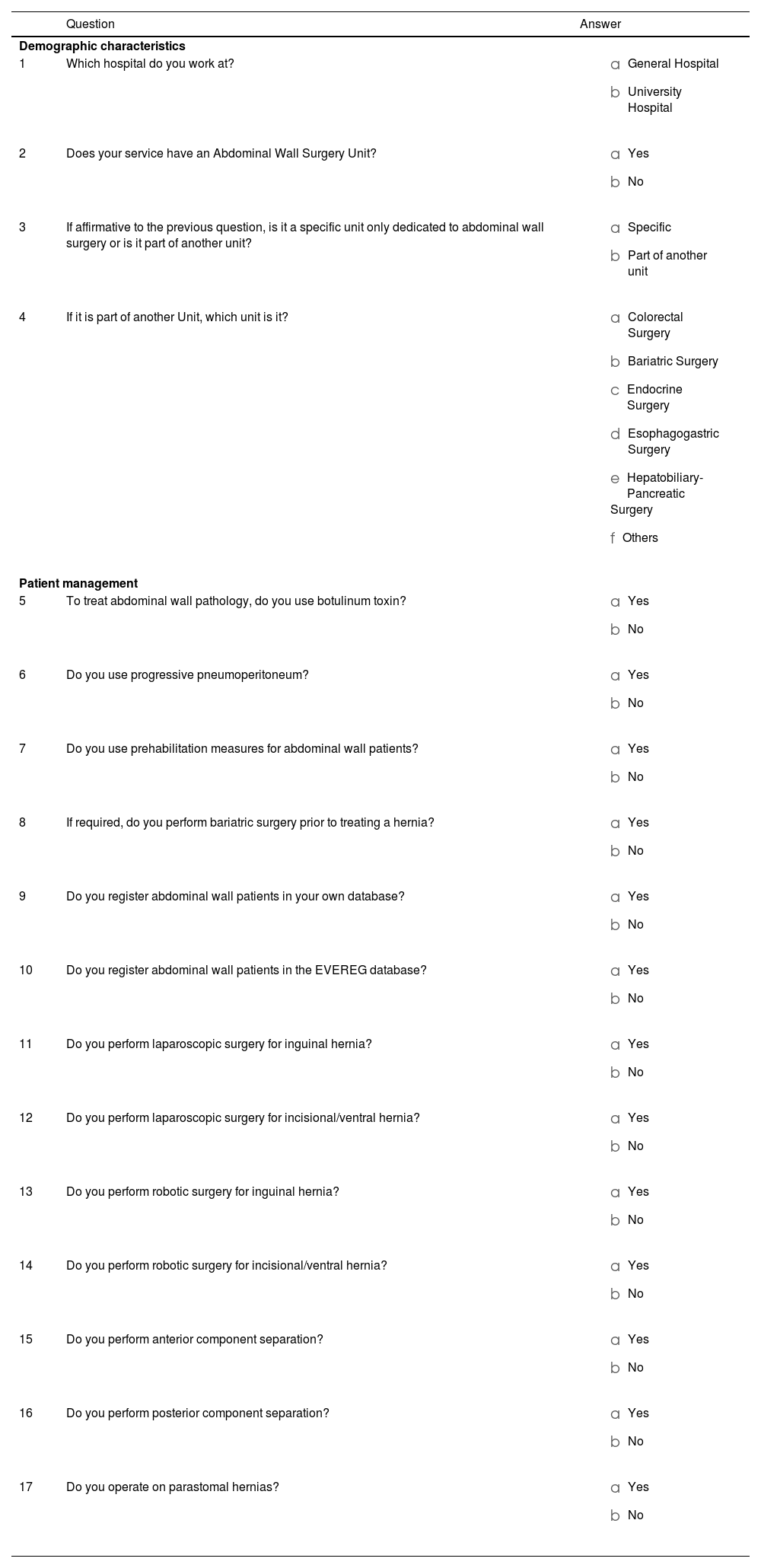
The questionnaire consisted of 17 questions (Table 1). It included 4 initial questions to understand the demographic characteristics of the respondents and potential abdominal wall units (type of hospital, presence of a specific wall unit or integrated into another training area and if so, in which one). The remaining 13 questions explored whether the management of patients with abdominal wall pathology followed a "pattern" of specialized management. Thus, 4 questions were about preoperative management (i.e., prehabilitation), 2 questions about activity control through own databases or specific to the abdominal wall, 4 questions about the use of minimally invasive surgical approaches to the abdominal wall, 2 questions about the use of advanced abdominal wall repair techniques, and finally 1 question about whether a specific type of hernia is operated on that could be considered as complex abdominal wall (i.e., parastomal hernia).
Questionnaire.
| Question | Answer | |
|---|---|---|
| Demographic characteristics | ||
| 1 | Which hospital do you work at? |
|
| 2 | Does your service have an Abdominal Wall Surgery Unit? |
|
| 3 | If affirmative to the previous question, is it a specific unit only dedicated to abdominal wall surgery or is it part of another unit? |
|
| 4 | If it is part of another Unit, which unit is it? |
|
| Patient management | ||
| 5 | To treat abdominal wall pathology, do you use botulinum toxin? |
|
| 6 | Do you use progressive pneumoperitoneum? |
|
| 7 | Do you use prehabilitation measures for abdominal wall patients? |
|
| 8 | If required, do you perform bariatric surgery prior to treating a hernia? |
|
| 9 | Do you register abdominal wall patients in your own database? |
|
| 10 | Do you register abdominal wall patients in the EVEREG database? |
|
| 11 | Do you perform laparoscopic surgery for inguinal hernia? |
|
| 12 | Do you perform laparoscopic surgery for incisional/ventral hernia? |
|
| 13 | Do you perform robotic surgery for inguinal hernia? |
|
| 14 | Do you perform robotic surgery for incisional/ventral hernia? |
|
| 15 | Do you perform anterior component separation? |
|
| 16 | Do you perform posterior component separation? |
|
| 17 | Do you operate on parastomal hernias? |
|
Access to the form (questionnaire) and the invitation to complete it was sent via email to all members registered in the AEC's abdominal wall section, this email included a hyperlink to access the questionnaire. The email was resent on two occasions. All responses were anonymous. Descriptive statistics are presented.
ResultsAccreditation of abdominal Wall surgery unitsMinimum criteriaFor criteria 1, 2, and 3 (Recognition of the Unit by the Health Center, specifying its service portfolio, accreditation of the availability of a specific operating room, and accreditation of a minimum composition of specialist doctors with exclusive dedication), the required proof is a certificate issued by the Medical Direction of the Hospital or the Head of Service, attaching the service portfolio, specifying the specific operating room, its availability, and the composition of the unit with the identification of the professionals involved.
Regarding criterion 4 (Commitment to include cases in a specific database or registry for a period not less than 1 year from the application) and since in Spain we have had a specific database for abdominal wall surgery named EVEREG since 2012,20 it was decided that the required proof of compliance with this criterion would be a document of commitment and truthfulness in the inclusion of data in the EVEREG register, signed by the coordinators of the register.
Specific criteria- 1
Criteria in the care area:
- 2)
Human and material resources: two people in a specialized wall unit and one person in a hybrid unit (wall surgery encompassed in another unit). A minimum of one surgical session per week for complex pathology and one weekly session for simple surgery.
- 3)
Quality: Certificate of membership to the EVEREG register. Protocols and/or clinical action guidelines.
- 4)
Care activity and results: performance of prehabilitation (e.g., botulinum toxin and/or progressive pneumoperitoneum), performance of a minimum of 30 minimally invasive surgery procedures per year, performance of anterior and posterior component separation and repair of paraestomal hernia, at least 15 cases per year. Presence of an outpatient inguinal hernia repair circuit, at least 150 cases per year.
Optimal results according to established standards,21–23 are recurrence rates for primary inguinal and ventral hernia of 2–5% with surgical site infection (SSI) rates of 0.5–2% and chronic pain rates lower than 10%. For incisional hernia, optimal results are considered to be recurrence rates of 10–15%, SSI rates of 2–5%, and chronic pain rates lower than 5%.
- a)
Service portfolio: Outpatient and inpatient inguinal hernias and treatment of their short, medium, and long-term complications (mesh infection, chronic pain, recurrence). Primary ventral hernias and their short, medium, and long-term complications. Rectus diastasis associated with primary ventral hernias. Simple and complex incisional hernias.24 Paraestomal hernias. Other pathologies (Synchronous abdominal wall surgery with intra-abdominal tumors (colon, small intestine, hepatobiliary-pancreatic surgery, Urology, Gynecology)
Synchronous abdominal wall surgery with intestinal transit reconstruction (previous stomas). Abdominal wall tumors.
- e)
Activity report: Document proving the activity report of the accreditation year and certification by the Head of Service of its completion in the two previous years (including the accreditation year).
- f
Criteria in the research area
The following are considered mandatory criteria for accreditation:
- a)
Participation in clinical and/or basic research projects, requiring a certificate of participation and the approvals of the hospital's ethics committee.
- b)
Presentation at congresses of at least three communications on abdominal wall surgery in the accreditation year or five in the last two or eight in the last three. Presentation certificates are required as proof.
- c)
Participation in the EVEREG register, with its corresponding certificate.
Optional (non-mandatory) criteria in the research area include possession of a doctorate by at least one member of the unit or having directed doctoral theses and the publication of at least one article in an indexed journal or a book chapter on abdominal wall topics in the last 5 years.
- 3
Criteria in the teaching area
The following are considered mandatory criteria in this area, accompanied by their corresponding supporting documents: attendance at a training activity related to the abdominal wall. Some member of the unit being a university professor or a figure at the university (this criterion is only mandatory for university hospitals). Accreditation of membership to the AEC Abdominal Wall Section and the European Hernia Society (at least one member of the unit in the two years prior to accreditation). In hospitals with residents, scheduled rotation of residents through the unit.
Optional criteria for the teaching area include invitations to lectures at congresses or courses for at least one member of the unit; training stays of at least 1 month (national or international), for at least one member of the unit in the last 5 years prior to accreditation; accreditation of the European abdominal wall board for at least one member of the unit; organization of training stays in the unit for residents or specialists; organization of educational activities related to abdominal wall surgery (Webinars, Courses, Congresses, Symposiums, Seminars).
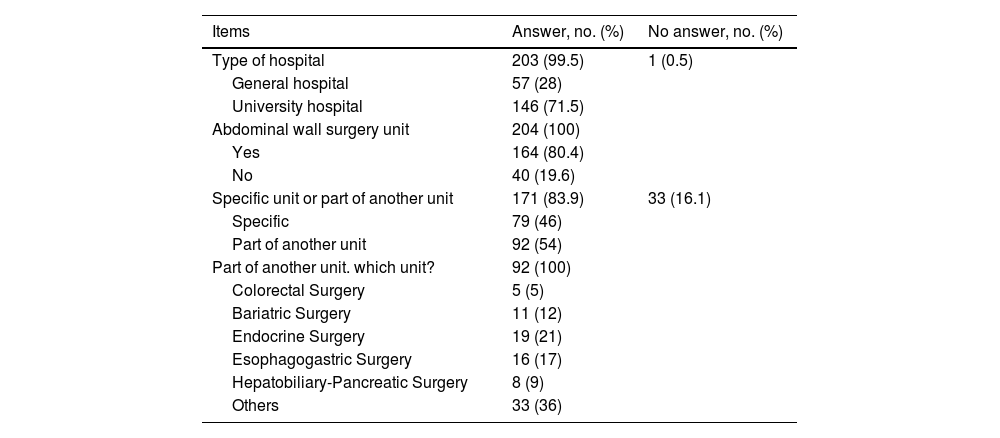
QuestionnaireDemographic characteristicsOut of the 1181 surgeons registered in the AEC abdominal wall section and after sending 2362 emails, responses to the questionnaire were counted in 204 (17%). Of these, the majority (146 [71.5%]) belonged to a university hospital and 164 (80.4%) claimed to have an abdominal wall surgery unit in their service. 171 (83.9%) surgeons responded to the question of whether they had a specific wall unit or integrated into another unit and of these 92 (54%) claimed that their unit was integrated into another unit Table 2.
Demographic characteristics.
| Items | Answer, no. (%) | No answer, no. (%) |
|---|---|---|
| Type of hospital | 203 (99.5) | 1 (0.5) |
| General hospital | 57 (28) | |
| University hospital | 146 (71.5) | |
| Abdominal wall surgery unit | 204 (100) | |
| Yes | 164 (80.4) | |
| No | 40 (19.6) | |
| Specific unit or part of another unit | 171 (83.9) | 33 (16.1) |
| Specific | 79 (46) | |
| Part of another unit | 92 (54) | |
| Part of another unit. which unit? | 92 (100) | |
| Colorectal Surgery | 5 (5) | |
| Bariatric Surgery | 11 (12) | |
| Endocrine Surgery | 19 (21) | |
| Esophagogastric Surgery | 16 (17) | |
| Hepatobiliary-Pancreatic Surgery | 8 (9) | |
| Others | 33 (36) |
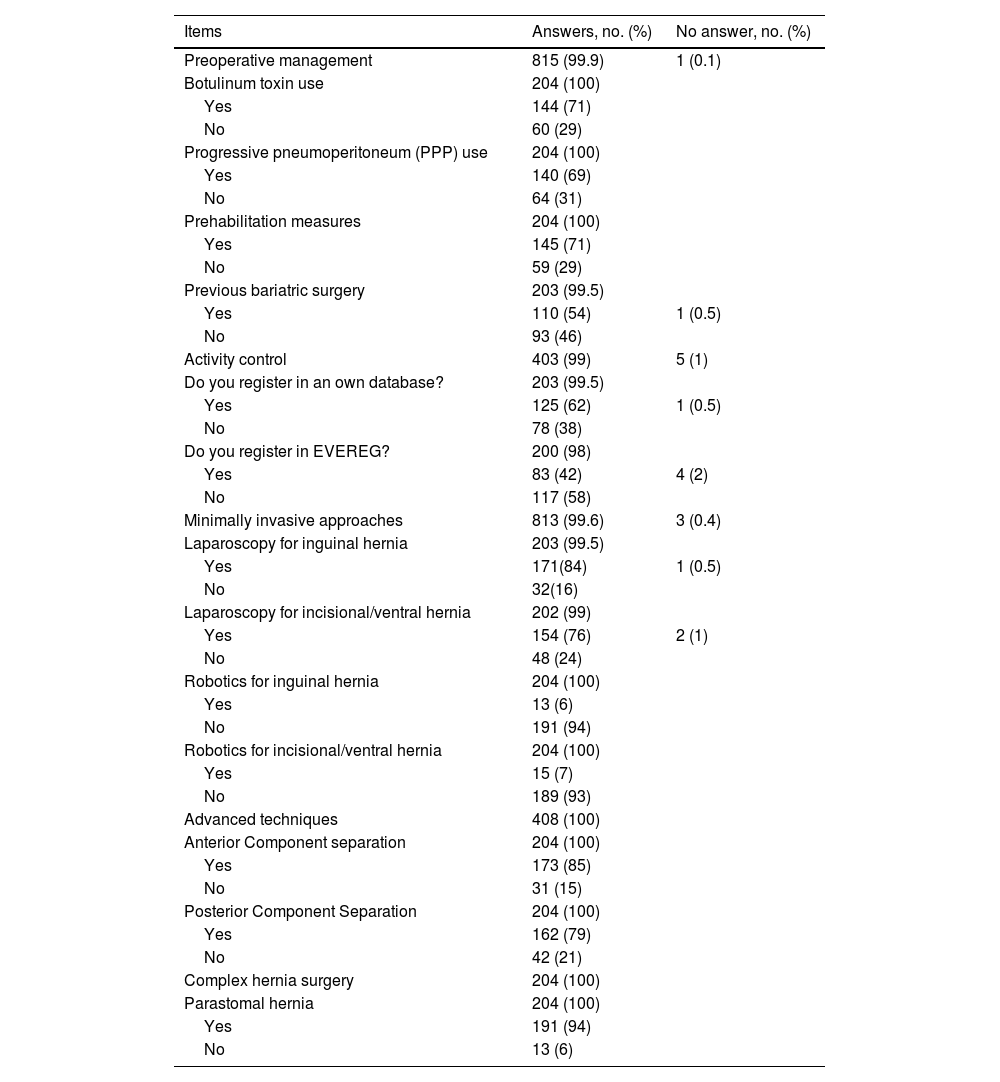
59 (29%) surgeons answered that they did not prehabilitate their patients and only 110 (54%) answered affirmatively to the question of whether they performed bariatric surgery prior to the treatment of a hernia Table 3.
Patients management.
| Items | Answers, no. (%) | No answer, no. (%) |
|---|---|---|
| Preoperative management | 815 (99.9) | 1 (0.1) |
| Botulinum toxin use | 204 (100) | |
| Yes | 144 (71) | |
| No | 60 (29) | |
| Progressive pneumoperitoneum (PPP) use | 204 (100) | |
| Yes | 140 (69) | |
| No | 64 (31) | |
| Prehabilitation measures | 204 (100) | |
| Yes | 145 (71) | |
| No | 59 (29) | |
| Previous bariatric surgery | 203 (99.5) | |
| Yes | 110 (54) | 1 (0.5) |
| No | 93 (46) | |
| Activity control | 403 (99) | 5 (1) |
| Do you register in an own database? | 203 (99.5) | |
| Yes | 125 (62) | 1 (0.5) |
| No | 78 (38) | |
| Do you register in EVEREG? | 200 (98) | |
| Yes | 83 (42) | 4 (2) |
| No | 117 (58) | |
| Minimally invasive approaches | 813 (99.6) | 3 (0.4) |
| Laparoscopy for inguinal hernia | 203 (99.5) | |
| Yes | 171(84) | 1 (0.5) |
| No | 32(16) | |
| Laparoscopy for incisional/ventral hernia | 202 (99) | |
| Yes | 154 (76) | 2 (1) |
| No | 48 (24) | |
| Robotics for inguinal hernia | 204 (100) | |
| Yes | 13 (6) | |
| No | 191 (94) | |
| Robotics for incisional/ventral hernia | 204 (100) | |
| Yes | 15 (7) | |
| No | 189 (93) | |
| Advanced techniques | 408 (100) | |
| Anterior Component separation | 204 (100) | |
| Yes | 173 (85) | |
| No | 31 (15) | |
| Posterior Component Separation | 204 (100) | |
| Yes | 162 (79) | |
| No | 42 (21) | |
| Complex hernia surgery | 204 (100) | |
| Parastomal hernia | 204 (100) | |
| Yes | 191 (94) | |
| No | 13 (6) |
78 (38%) answered that they did not register in their own database and 117 (58%) that they did not register in EVEREG Table 3.
Minimally invasive approachesThe majority answered that they perform laparoscopic surgery for inguinal and incisional hernias and very little robotic surgery for both types of hernias Table 3.
Advanced techniquesThe majority of the surgeons who responded to the survey answered affirmatively to the question of whether they performed anterior or posterior component separation Table 3.
Intervention of complex hernia(94%) of the surveyed surgeons answered that they do operate on paraestomal hernias.
DiscussionIn the last 20 years, and probably more markedly in the last decade, general surgery has increasingly fragmented into subspecialties.25 Processes within the specialty of General and Digestive Surgery (GDS) that were previously treated indistinctly by "general surgeons" are now treated by "subspecialists" (i.e., highly specialized) and it is unlikely that this paradigm shift towards "subspecialization" within general surgery is reversible.25 Aware of this situation, the AEC considers it "essential to define and regulate the acquisition of high specialization competences within GDS, and proposes the Regulation for the accreditation of specialized surgical units".18,19 The objectives of the AEC are clear: to favor the consolidation and organization of the current reality of the GDS specialty in most hospitals in our country, to collaborate so that legislation on specific training areas within the specialty is well defined, and to lay the foundations for the training of specialists in the different areas of subspecialization.18 Ultimately, as previously published: "the objective of accreditation by the AEC is, therefore, to define specialized surgical units as those functional elements of the health system that meet the defined requirements regarding their provision, solvency, care specialization, teaching, and research".18
Abdominal wall surgery is also incorporated into the accreditation regulations for specialized units proposed by the AEC.19 From our point of view, this incorporation is not serendipitous and comes from a general surgical perspective related to our environment and from a local surgical perspective related to the analysis of a survey on abdominal wall units in our country.
Regarding our environment and to the best of our knowledge, it is the European continent that is the leading promoter of the recognition (globally) of abdominal wall surgery as its own entity. Principally driven by the EHS and the UEMS. The EHS promotes projects recognizing the growing need for specialized centers/units in abdominal wall surgery26 and to train specialists in abdominal wall surgery12; promoting the publication of clinical guidelines referring to different aspects of the treatment of abdominal wall pathology27–33 or participating in educational platforms about the abdominal wall,34 among other multiple activities. The UEMS has also played a definitive role in the specialization of abdominal wall surgery by forming a specific working group and creating the "European Board of Abdominal Wall Surgery" (EBAWS).13 Probably based on the previous framework, specific pioneering proposals have been made in some countries in our environment16,17 that attempt to define (each in its context) the requirements that different centers must have for a specialized practice of abdominal wall surgery. The AEC's proposal presented in this work adds to these few pioneering initiatives in Europe and defines the AEC as one of the first surgical societies worldwide to propose criteria for what can be considered a specialized unit in abdominal wall surgery. On the other hand, recently other parts of the world such as the USA (with clear influence on global surgical evolution) are beginning to become aware of the differences between centers in treatments for complex abdominal wall reconstructions35 and the need to redefine the knowledge of an emerging specialty such as specialization in abdominal wall surgery.36
Regarding the local surgical perspective derived from the analysis of a survey on abdominal wall surgery units in our country, it is interesting to observe how the majority (71%) of respondents belonged to university hospitals and the majority (80.4%) responded that they had an AWS unit in their service. However, more than half (54%) responded that it was not a unit with exclusive dedication to abdominal wall surgery but integrated into another unit, which was not clearly defined as the highest percentage of responses (36%) was that the abdominal wall unit was integrated into the option "other units". On the other hand, very important aspects in the proper management of patients with abdominal wall pathology that should align with current clinical practice guidelines offered contradictory responses, thus, 29% of respondents did not use prehabilitation measures or 46% did not perform bariatric surgery (if necessary) before abdominal wall surgery, which seems not to align with the current recommendations of the ASMBS (American Society for Metabolic and Bariatric Surgery) and the IFSO (International Federation for the Surgery of Obesity and Metabolic Disorders) recommending bariatric surgery in case of elective abdominal wall hernia surgery and severe obesity.37 Furthermore, 38% did not register their operated patients in their own database and 58% did not do so in EVEREG. Nevertheless, the majority responded that they perform minimally invasive surgery for inguinal and incisional hernias, advanced abdominal wall repair techniques such as component separation (anterior or posterior), or complex abdominal wall pathology such as paraestomal hernia. It is paradoxical to observe an environment of majority practice of advanced and complex repair techniques, in relation to a variable structural organization, with high percentages of potential poor management of patient prehabilitation measures and defective activity control/registration. It seems logical, therefore, that the AEC proposes an accreditation model for abdominal wall units to favor the consolidation and organization of the current reality of this part of the GDS, in the face of a national survey where an insufficient definition of abdominal wall units in terms of structural quality (i.e., specific or integrated units, organizational definition), process quality (i.e., prehabilitation, collaboration with other units, guidelines follow-up), or outcome quality (i.e., data registration, complications, morbidity and mortality) seems to be guessed.
Limitations in the present work can be considered the potential discrepancy in the definition of the accreditation structure where perhaps other characteristics could be considered. However, the joint work of the AEC scientific committee and the abdominal wall section has covered from minimum to specific criteria that encompass the care, teaching, and research areas, laying the foundations for the optimal care of patients and the training of specialists in the specific area of the abdominal wall.
The results of the survey should also be interpreted with some limitations. Firstly, the survey was self-administered and was not subjected to internal or external validation before its distribution. Although the survey instrument had not been validated, 2 experienced abdominal wall surgeons reviewed its content. Secondly, the response rate was 17% (204/1181). However, some studies have shown that bias induced by the response rate does not seem to pose a great threat to the validity of the questionnaires.38 Even so, it is possible that the responses do not accurately represent the practice patterns and attitudes of the surveyed surgeons.38 On the other hand, this is the largest and only survey to date among surgeons regarding AWS units in our country. Thirdly, the survey was distributed among members of the AEC's abdominal wall section, but surgeons who do not belong to this were not asked. There is likely to be a selection bias, as the section members have a declared interest in abdominal wall surgery. However, precisely the fact that the survey is made to surgeons with a special interest in the abdominal wall reinforces the veracity of the results and the need for an accreditation proposal.
In summary, the evolution of GDS leads to subspecialization in a process that does not seem reversible. The process of accreditation of abdominal wall surgery units in our country will contribute to an improvement in structural quality, process quality, and outcome quality of abdominal wall surgery.
FundingThis work has not been funded by any public or private funds.
Artificial intelligenceThe authors declare that artificial intelligence has not been used in the preparation of this work.
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to this work.