One of the recent advances in bariatric surgery is the use of magnetic devices. This research paper describes magnetic liver retraction in morbidly obese patients during bariatric surgery. A descriptive, prospective and observational study was carried out, analyzing 100 patients in whom magnetic retraction was used. Mean and SD body mass index was 46.1 ± 5.09 kg/m2. The magnetic system was successfully used for liver retraction in 95% of cases; in only 5% of cases was its use not possible due to hepatomegaly and severe hepatic steatosis. According to the results, magnetic liver retraction can be safe and used in bariatric surgery, regardless of body mass index and with a low percentage of complications.
Uno de los avances recientes en cirugía bariátrica es el uso de dispositivos magnéticos. Esta investigación reporta la retracción magnética del hígado en pacientes con obesidad mórbida durante la cirugía bariátrica. Se realizó un estudio descriptivo, prospectivo y observacional, seleccionando 100 pacientes donde se utilizó la retracción hepática magnética. Entre los 100 pacientes seleccionados, la media/DE del índice de masa corporal fue de 46,1 ± 5,09 kg/m2. El sistema magnético se utilizó con éxito para la retracción hepática en el 95% de los casos, sólo en el 5% de los casos no fue posible utilizarlo debido a hepatomegalia y esteatosis hepática severa. Según los resultados, la retracción hepática magnética puede ser segura y utilizada en cirugía bariátrica independientemente del índice de masa corporal con un bajo porcentaje de complicaciones.
Bariatric surgery is the gold standard treatment for morbid obesity. The approach to these procedures has been undergoing changes, including minimally invasive techniques. One involves the introduction of innovative magnetic devices in laparoscopic surgery, which can be used to perform incisionless approaches, while magnetic assistance can also perform essential steps of the surgery, such as liver retraction.1
During bariatric surgical procedures, adequate hepatic retraction is vitally important to achieve good visualization of the surgical field, exposing the hiatus and the gastroesophageal junction. These devices help us achieve better visualization of the surgical field in minimally invasive surgeries or incisionless approaches.2
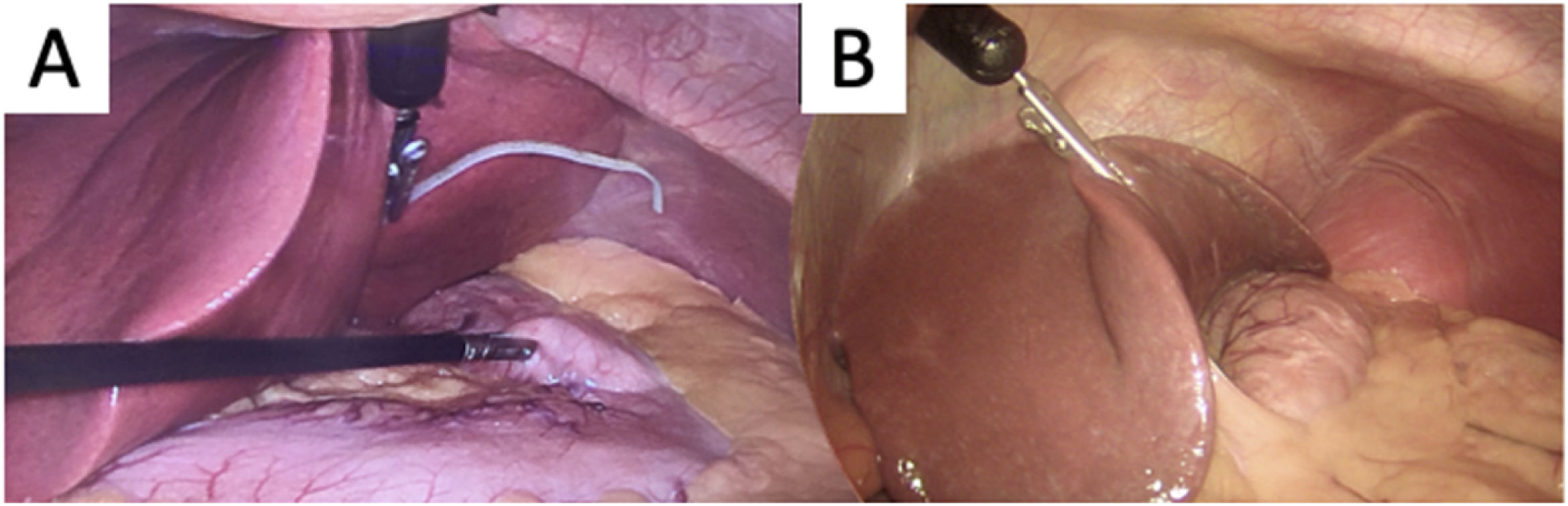
Surgical techniqueThe magnetic device consists of an internal magnet, an external magnet, an enhancer and silastic tubing (Fig. 1). The internal magnet can be introduced through a 12-mm laparoscopic trocar or through the umbilicus in the reduced-port approach.
To achieve adequate liver retraction, we use the device in 2 ways. First of all, in cases of severe hepatic steatosis and hepatomegaly, we use the device by attaching silastic tubing to the right pillar of the diaphragm, and on this silastic tubing we also attach the internal magnetic grasper to obtain the exposure of the surgical field. In addition, we can attach the enhancer to the internal magnet to give it more strength (Fig. 2A).
In cases with a smaller liver and non-severe steatosis, we can attach the magnetic grasper directly to the left liver lobe (Fig. 2B). With the external magnet, we can control the internal magnetic grasper. The use of the external magnet is shown in Fig. 3.
The magnetic system used was the IMANLAP® Project. This study was approved by the Institutional Review Board at the institution where the study was performed, and informed consent was obtained from all the participants included in the study.
Based on this cohort, mean BMI was 46.1 kg/m2. We found that magnetic liver retraction was able to be performed in 95% of the cases, while the 5% of failed attempts were associated with a severe degree of fatty infiltration and hepatomegaly. The use of silastic tubing was necessary in 66% of cases. The time of use of the magnetic device was the entire surgical time; for instance, RYGB was the main procedure with a duration of 93.55 ± 25.64 min.
We observed a 3% rate of minor complications, such as minor liver laceration when using the magnetic device directly on the hepatic lobe. These lacerations were resolved with compression and conservative treatment. No cases of device malfunction were observed.
In the higher BMI grades, such as a BMI > 50 (representing 26% of our study population), liver retraction was successful in 24%, which is an interesting result. However, regardless of BMI, this result was not directly related to the degree of hepatic fatty infiltration, as severe fatty liver infiltration was also present among patients with lower BMI. Specifically, 3% of the failed attempts had a mean BMI of 43 kg/m2, with severe fatty infiltration and hepatomegaly as determining factors.
DiscussionIn bariatric surgery and upper gastrointestinal surgery, it is important to achieve appropriate exposure of the surgical field, mainly of the gastroesophageal junction and crura.3 Some authors conclude that magnetic liver retraction can be a well-tolerated and effective option in bariatric surgery.4
In the literature, certain studies have reported applying the magnetic devices directly to the left liver lobe.2 We propose an alternative method using silastic tubing attached to the right pillar of the diaphragm. In 66% of patients in whom this method was applied, no complications were detected.
In contrast, the usual method reported in the literature and applied in 29% of the cases is the magnetic grasper positioned directly to the left liver lobe. However, the results with this method are associated with complications, such as minor hepatic lacerations, which in our experience was reported in 3%. We avoid these types of complications with the alternative method using silastic tubing.
This trocar-free method or incisionless approach is associated with fewer infections of the surgical port and incisional hernias. It is an effective option in minimally invasive surgery that can be performed while maintaining the safety of the procedure.5 Several important factors can influence the selection of the surgical approach in minimally invasive surgeries, and better aesthetic results can be obtained with these devices. Regardless of BMI, some patients present severe hepatopathy, so it is better to avoid the magnetic device in these special cases, thereby avoiding any increase in the percentage of complications. This study suggests new lines of research in hepatopathy and magnetic devices in magnetic-laparoscopic surgery in order to obtain better applications.
ConclusionsMagnetic liver retraction can be a safe and feasible technique to use in bariatric surgery, regardless of the body mass index. The alternative methods presented, such as using silastic tubing and enhancer, can avoid complications.
Funding informationThis study was self-funded. No funding was received for this article.
Human and Animal RightsAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committees approved this study.
ConsentWritten informed consent was obtained from the patients for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interestThe authors have no conflict of interest to declare.
We thank each person in my team for putting all their efforts into taking this intuition to the top level and all my patients without their trust we could never reach this greatness.