An anomalous origin of the coronary artery is an uncommon congenital disorder. Even though the pathology is generally asymptomatic, it can present with life-threatening symptoms. Two cases with an anomalous origin of the right coronary artery are assessed. Though both patients’ arterial anomalies were alike, the surgical procedure was different in each case. The unroofing technique and coronary artery bypass grafting are compared to evaluate different surgical approaches for a personalize treatment of the pathology.
El origen anómalo de la arteria coronaria es una enfermedad congénita poco común. Aunque la afección es generalmente asintomática puede presentarse con síntomas potencialmente mortales. Se valoran 2 casos con origen anómalo de la arteria coronaria derecha. Aunque las anomalías arteriales de ambos pacientes eran similares, el procedimiento quirúrgico fue diferente en cada caso. Se comparan la técnica de unroofing y la cirugía de revascularización miocárdica para evaluar diferentes abordajes quirúrgicos para un tratamiento personalizado de la enfermedad.
An anomalous origin of the coronary artery (AOCA) is an uncommon congenital disorder, presenting with an incidence of 0.3-1%.1 Most AOCA are asymptomatic and found incidentally, however, about 20% of these anomalies can present with life-threatening symptoms such as arrhythmias, myocardial infarction, or sudden cardiac death (SCD).2,3 The latter being of particular concern when the right vessel originates from the left sinus and follows an interarterial course between the aorta and the pulmonary artery.
Although SCD in young athletes is rare, AOCA is responsible for up to 15% of these lethal outcomes.4 Elderly patients are less likely to experience SCD, however they suffer from more persistent anginal symptoms.1
Herewith, two cases presenting an anomalous origin of the right coronary artery (AORCA) will be assessed. Though both patients’ arterial anomalies are alike, the clinical manifestations and comorbidities are distinct. We aim to highlight the importance of evaluating different surgical treatment options for AORCA in an attempt to adjust the surgical management to each patient.
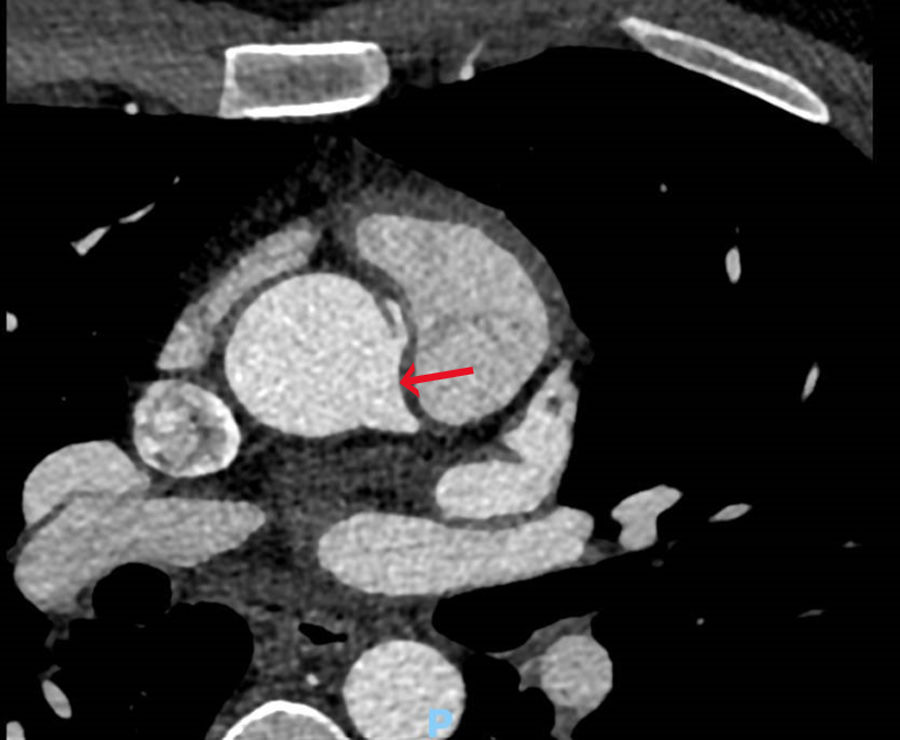
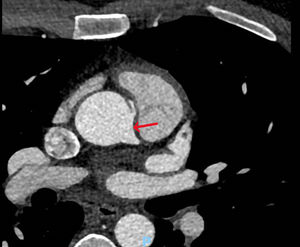
Case presentationsCase 1A 37-year-old male athlete, presented to the hospital for a sport's physical examination. Despite having no clinical symptoms, an ST segment depression was found in the inferior and precordial leads during a cardiopulmonary stress test (maximum descent of 0.26mV at aVF). Physical examination, ECG and Doppler ultrasound presented no significant findings. A coronary computed tomography angiography was performed to further define his underlying condition. The images revealed an AORCA, which stemmed anterosuperiorly from the left coronary sinus and approximately 23mm from the aortic valve, at the level of the sinotubular junction (Fig. 1). No pathological findings were reported regarding coronary caliber or the remaining coronary branches.
The patient was admitted for open heart surgery. Undergoing a median sternotomy approach, the right coronary artery was meticulously dissected. It appeared to originate from the anterolateral surface of the aorta, displaced approximately 1–1.5cm anteriorly. Cardiopulmonary bypass was initiated, and a 2.5mm dilator was introduced into the right coronary artery which originated from the left coronary sinus, a 2–2.5cm aortic intramural course was appreciated. A subsequent unroofing technique was performed. Postoperatively, the patient's course was satisfactory. Three months after surgery, the patient is in functional grade I (NYHA scale).
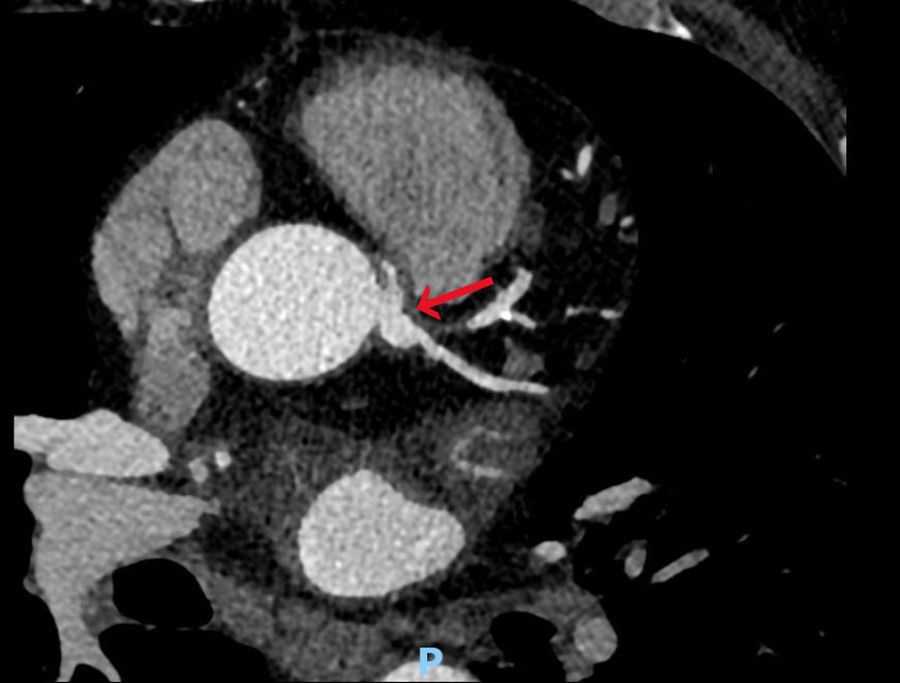
Case 2We present the case of an 80-year-old male with a history of hypercholesterolemia, arterial hypertension, and diagnosed in 2014 with mitral insufficiency which required implantation of a biological valve prosthesis. While undergoing a cardiac catheterization, an AORCA was found.
In April 2020, the patient presented with dizziness, instability, dyspnea and worsening angina, rising suspicion for acute coronary syndrome. Sinus rhythm and left ventricular hypertrophy were observed on ECG. Two stress tests, both of which had to be halted due to angina and dyspnea, were electrically negative for ischemia. A coronary computed tomography angiography presented similar findings (Fig. 2), yet a PET scan showed possible inferior ischemia.
After undergoing several tests all possible causes of the symptoms were discarded, leaving the AORCA as the last possible option. A coronary artery bypass grafting (CABG) with reversed-flow saphenous vein graft (SVG) was scheduled for the treatment of the condition.
During the CABG procedure, a saphenous vein graft was obtained, and cardio-pulmonary bypass was started. The distal anastomosis was performed at the distal right coronary artery, then approximately 14cm of VEST 1B (Vascular Graft Solutions, Tel Aviv, Israel) was threaded on the graft to avoid vein graft failure. The proximal anastomosis was performed to the trunk of the aorta and bypass exit protocol was carried out.
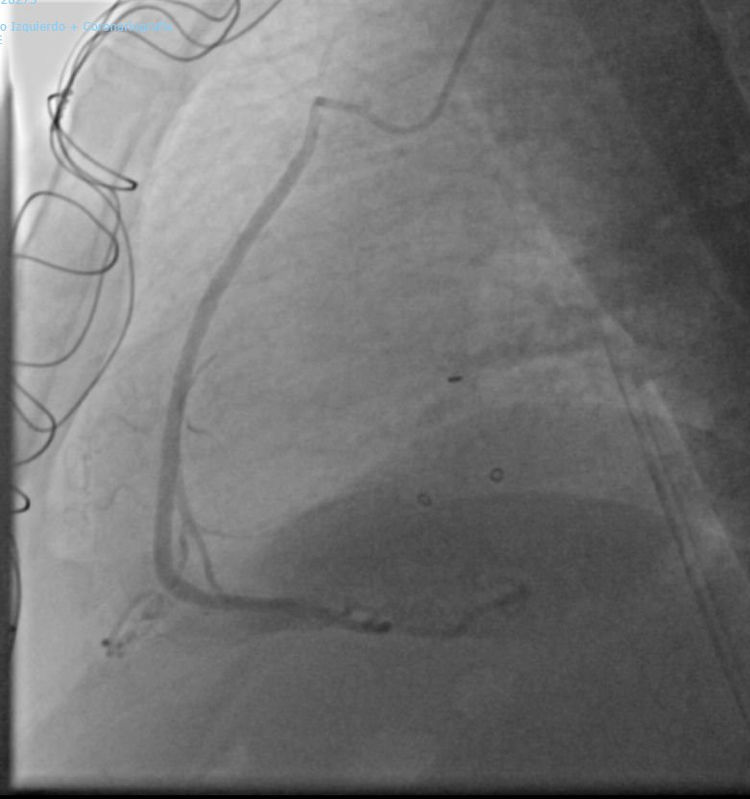
Post-surgery recovery was favorable. Since discharge the patient is in functional grade I (NYHA scale). A year after the surgery a coronary angiogram showed that the SVG was patent (Fig. 3).
DiscussionAn AOCA is a congenital heart defect in which a coronary artery follows an aberrant course, most typically arising from the opposite sinus of Valsalva.1 Among the different subtypes, the most clinically concerning AOCA are those that follow an interarterial course between the pulmonary artery and aorta.
The most life-threatening cardiac complication associated with this condition is SCD.4 The mechanism believed to cause SCD in young athletes is the mechanical compression of the intra-arterial section of the AOCA, result of the great vessel dilation during physical exercise.1 Another way in which ischemia can happen is acute angle take off from the opposite sinus of Valsalva.1 This usually courses with a slit-like ostium at the aortic trunk that can collapse during exercise. Moreover, recent studies have shown that AOCA predisposes patients to suffer vasospasms.1 While this could be due to the mechanical irritation, there are indications that these aberrant vessels might be associated with endothelial dysfunction since, many patients continue having vasospasms even 2 years after surgery.1
Several surgical techniques have been proposed for the repair of an AOCA. It is difficult to compare the quality of the outcome achieved between the different surgical options, since the anatomy and clinical presentation of the AOCA vary from patient to patient.
Generally, all patients with an anomalous origin of the left coronary artery (AOLCA) should undergo surgery, whereas the treatment options for the patients with an AORCA are still unclear.5 According to the American College of Cardiology/American Heart Association guidelines, patients with an AORCA following an interarterial course are recommended to undergo surgical revascularization if ischemic symptoms are present.4 The surgical strategies that have been proposed vary between CABG, unroofing and coronary ostioplasty.5,6
As with the first case, patients are typically asymptomatic making it difficult to diagnose an AOCA in advance. The prevention of SCD is challenging, since young patients do not usually undergo cardiac screening tests in which the anomaly can be incidentally found. Fortunately, this patient underwent a cardiopulmonary stress test and the AORCA was diagnosed in time.
The patient was considered eligible for an unroofing procedure since the cardiopulmonary stress test showed inferior NSTEMI and by, considering the patient's predisposition to suffer from SCD.
The coronary unroofing technique is the most common surgical procedure used for AOCA repair.6 It is useful when there is a long proximal segment of the aberrant coronary artery following an intramural course.6 It is highly recommended that the unroofing procedure is only performed when the intra-arterial portion of the AOCA is long enough, in such a manner that the surgery will be able to move the new ostia past the inter-arterial section towards the correct sinus of Valsalva.5 In the patient from the first case, the intra-arterial course was 2–2.5cm long and posed no contraindication for this surgery.
Furthermore, the exact location of the intramural course must be carefully considered since it sometimes descends towards the aortic valve and crosses the valvular commissure. In these situations, the typical unroofing procedure is contraindicated.6 Therefore, it is relevant to know that in the first patient the intramural course is found 23mm above the aortic valve, and thus the surgery is unlikely to cause aortic valve damage.
In the second case, we presented an 80-year-old patient, casually diagnosed with AORCA while undergoing a cardiac catheterization for a mitral valve replacement. At that moment, surgical revascularization was not indicated since there was no evidence of ischemia and the patient was asymptomatic.4 However, 5 years later, the procedure was indicated due to the patient's symptoms attributed to the AORCA.
In contrast to the first patient, this one had signs of ischemia possibly attributed to his AORCA. The fact that the vessel followed an interarterial course made it more likely to be subject to compression causing flow restriction. A CABG was elected as the optimal surgical treatment for the patient. This procedure carries a low level of difficulty, so it is particularly indicated when treating older patients.6,7
In this case, an unroofing technique was considered non-optimal since it carries a significant risk of causing aortic valve damage and by considering the age of the patient.1 In addition, due to prior mitral valve replacement, adhesions were formed around the aorta, which could have posed a challenge in the process of dissecting the aorta for an unroofing surgery. We considered a CABG procedure to be the most suitable for the patient since it has shown favorable early and midterm results and there is no need for manipulation of the aortic valve.6
Two possible complications that must be taken into consideration when choosing this type of procedure are SVG failure and long-term loss of patency.5 Early SVG failure occurs generally during the first year after the surgical procedure.8 It arises as an adaptation of the vein graft to the high arterial pressures, resulting in an intimal hyperplasia, which decreases the internal diameter of the graft. The implantation of an external stent around the vein graft has been demonstrated to reduce the incidence of this complication by improving the flow patterns and preventing disruption of the endothelium.9 In the case presented above, the VEST was used to prevent the early failure of the graft.
Furthermore, the utilization of the SVG carries other problems associated with its decreased durability, as its patency declines over time, however, it is still considered the vessel of choice for CABG in situations such as right coronary artery grafting and the treatment of elderly patients, which have an average life expectancy shorter than is necessary for the graft to degenerate.8 The longevity of the graft is not a determinant factor for the prognostic value of patients in this age group.
Using a right internal thoracic artery as an alternative was discarded in this specific case since the use of this conduit carries other associated disadvantages such as competitive flow. Unlike veins, arteries have a broader muscular layer allowing the conduit to regulate their luminal surface in response to variations in blood flow, making the arterial conduit more prone to competitive flow, leading to occlusion, hypoperfusion and ischemia.
Due to the low prevalence of AORCA in the population, there are few studies that evaluate the long-term outcomes of patients undergoing its surgical correction. In a prospective cohort study conducted by Mery et al.,10 the postoperative recovery of 44 patients undergoing an AORCA repair was evaluated. On 35 of these subjects an unroofing technique was performed, 1 patient received a CABG and the remaining 8 underwent other procedures such as ostioplasty or coronary artery translocation. In postoperatory follow-up visits it was found that 40 patients were now asymptomatic, and 4 patients had remaining nonspecific chest pain. The most common complication reported by the authors was pericardial effusion which occurred in 4 patients. Regardless, the study concludes by reassuring that surgical treatment for these patients has great outcomes and low risks of postoperative complications.
The rare nature of the pathology makes it hard to conduct significant randomized controlled trials. Further prospective observational studies could be proposed as an alternative to assess long-term outcomes for each of the surgical procedures.
ConclusionAn AOCA is an uncommon congenital disorder that can present with life-threatening consequences such as SCD. Both cases presented, were diagnosed with an AORCA originating from the left sinus of Valsalva. The first patient underwent an unroofing procedure, useful when the AOCA has a long intramural trajectory and when the hypoperfusion symptoms originate from the compression of the intra-arterial segment. The second patient underwent a CABG procedure, particularly indicated when treating older patients. Early SVG failure can be prevented by implanting an external stent around the graft. Adjusting the surgical management to each patient is critical to achieve excellent results.
Informed consentWritten informed consent were obtained from the patients for the publication of this case report.
FundingThere has been no significant financial support for this work that could have influenced its outcome.
Conflict of interestThe authors declare that they have no conflict of interest.