To determine the distribution of consultation times, the factors that determine their length, and their relationship with a more participative, patient-centred consulting style.
DesignCross-sectional multicentre study.
LocationPrimary Healthcare Centres in Andalusia, Spain.
ParticipantsA total of 119 tutors and family medicine physician residents.
Principal measurementsConsultation length and communication with the patient were analysed using the CICCAA scale (Connect, Identify, Understand, Consent, Help) during 436 interviews in Primary Care.
ResultsThe mean duration of consultations was 8.8min (sd: 3.6). The consultation tended to be longer when the physician had a patient-centred approach (10.37±4.19min vs 7.54±2.98min; p=0.001), and when there was joint decision-making (9.79±3.96min vs 7.73±3.42min: p=0.001). In the multivariable model, longer consultations were associated with obtaining higher scores on the CICAA scale, a wider range of reasons for consultation, whether they came accompanied, in urban centres, and a smaller number of daily visits (r2=0.32). There was no correlation between physician or patient gender, or problem type.
ConclusionA more patient centred medical profile, increased shared decision-making, a wider range of reasons for consultation, whether they came accompanied, in urban centres, and less professional pressure all seem to be associated with a longer consultation.
Conocer la distribución del tiempo de consulta, los factores que determinan su duración y su relación con un estilo de consulta participativo y más centrado en el paciente.
DiseñoEstudio descriptivo multicéntrico.
EmplazamientoCentros de salud de Atención Primaria en Andalucía (España).
ParticipantesEn total, 119 tutores y residentes de medicina de familia.
Mediciones principalesSe analizó el tiempo de consulta y la comunicación con el paciente mediante la escala Conectar, Identificar y Comprender, Acordar y Ayudar (CICAA) en 436 entrevistas en Atención Primaria.
ResultadosLa duración media de las consultas fue de 8,8 min (DE: 3,86). La consulta fue más larga cuando el profesional tenía un perfil centrado en el paciente (10,37±4,19 vs. 7,54±2,98 min; p=0,001) y existía toma de decisiones compartida (9,79±3,96 vs. 7,73±3,42 min; p=0,001). En el modelo multivariable, una mayor duración de la consulta se relacionó con obtener mejores puntuaciones en la escala CICAA, un mayor número de motivos de consulta, presencia de acompañante, centros urbanos y un menor número de visitas diarias (r2=0,32). No hubo relación con el sexo del profesional, del paciente ni con el tipo de problema consultado.
ConclusionesUn perfil médico más centrado en el paciente, mayor toma de decisiones compartida, un mayor número de motivos de consulta, la presencia de acompañante, el ser centros de salud urbanos y una menor presión asistencial se muestran asociados a un mayor tiempo de consulta.
There are many different factors that influence interaction between patient and physician in medical practice, including the duration of the consultation.1,2 The appropriate length of a consultation is a controversial issue.1 In Spain there are precise limits (10min minimum on average), that under no circumstances should be exceeded.3
The Spanish Public Health System allocates 6min on average to consultations, much less than the 10–15min allocated in other European countries and the 20min in North America and Canada.1,4 A longer duration would allow a more comprehensive approach, exploring risk factors, prevention, and improving lifestyle.1,2 By contrast, a consultation lasting less than 10min, in addition to increasing dissatisfaction, could cause malpractice and higher costs.1
Several factors have been associated with longer consultations; older professionals, female patients, increased patient participation, a greater number of reasons for consultations or type of problem (psychological or social).5–8
Other factors such as if the patient is accompanied, are not so clear. For some authors this does not increase consultation length,9,10 while for others it does.11
The gender of the professional also seems to have an influence; women generally carry out longer consultations, which seems related to a more patient-centred experience, encouraging them to express themselves more.5,12–14Lastly, some authors find to communicate better with patients, a longer consultation is required.6,7 The importance of this finding would lie in the proven link between adequate communication and improvement of health.15,16
In Spain, a country where the increase in consultation time is a continuous demand, the relationship between consultation time and communication with patient has hardly been addressed.
In this study, we plan to discover how consultation length is distributed, as well as the factors associated with longer or shorter medical consultations in primary care. In particular we aim to understand whether better communication and a more patient-centred, participatory style consultation requires more time.
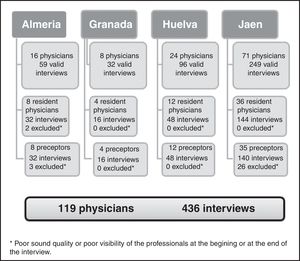
MethodologyDesign and study populationThis study is part of a larger project funded by the Andalusian Council and analyses the communicational profile of medical tutors and senior resident physicians of family and community medicine in four Andalusian cities.17
This is a cross-sectional, multicentre study carried out in health centres in four Spanish provinces. Andalusian physicians of family medicine participated, accredited as tutors and residents in their last year of training.
They were videotaped during regular working hours. The main researcher then selected 4 video recordings of each professional (excluding their first consultation and bureaucratic or internal consultations) at random, which were subsequently analysed by two people alien to the research and trained in the use and management of video recordings using the CICAA survey.
The intraobserver agreement by the intraclass correlation coefficient was 0.89 (95% CI 0.79–0.94) for the first observer and 0.91 (95% CI 0.84–0.95) for the second. The interobserver agreement of both was 0.94 (95% CI 0.89–0.96).
Variables in the studyThe main dependent variable was the total consultation time, measured in minutes, from the moment the patient entered the consultation until he left.
It was divided into three parts:
- a)
exploratory phase, from the beginning of the interview to the physical examination.
- b)
physical examination length.
- c)
resolution phase, from the end of the physical examination until the end of the interview.
The main independent variable was the score obtained on the CICAA17 questionnaire with three possible values for each item: 0 points (did not accomplish the set tasks), 1 point (acceptably accomplished the set tasks) and 2 points (achieved the set tasks completely or almost completely). The score can range from 0 to 58 points. In addition, two new variables were established: patient-centred communication and patient participation in decision making.
- -
Patient-centred communication: If a professional obtained a score of 7 points or more in the sum of the items 5, 10, 11, 12, 13, 14, 15, 16, 18 and 26 of the questionnaire, the communication was considered patient-centred (corresponding to the mean and median of the variable in this sample). Numbers relating to exploring the psychosocial sphere and patient-centred consultations in validating the questionnaire.19
- -
Patient involvement in decision making: The patient was considered to have been involved in decision making when the score in number 25 was 1 or 2, according to the work published by Moral et al.7
Other independent variables were the personal and professional characteristics of physicians that emerged during the interviews.17
Ethical aspectsThe research project was approved by the Ethics Committee of Health Research in Referral Hospitals. The informed consent of healthcare professionals and patients was obtained in writing or verbally during the video recordings.
Statistical analysisStatistical analysis was performed using the program SPSS (15.0), considering a level of less than or equal to 0.05 as significant.
The analysis of consultation length according to the characteristics of the physician, the patient and the interview, was conducted by using Student t tests, ANOVA, correlation and/or simple linear regression. Finally, a multiple linear regression model was constructed with length as the dependent variable, having previously checked the conditions.
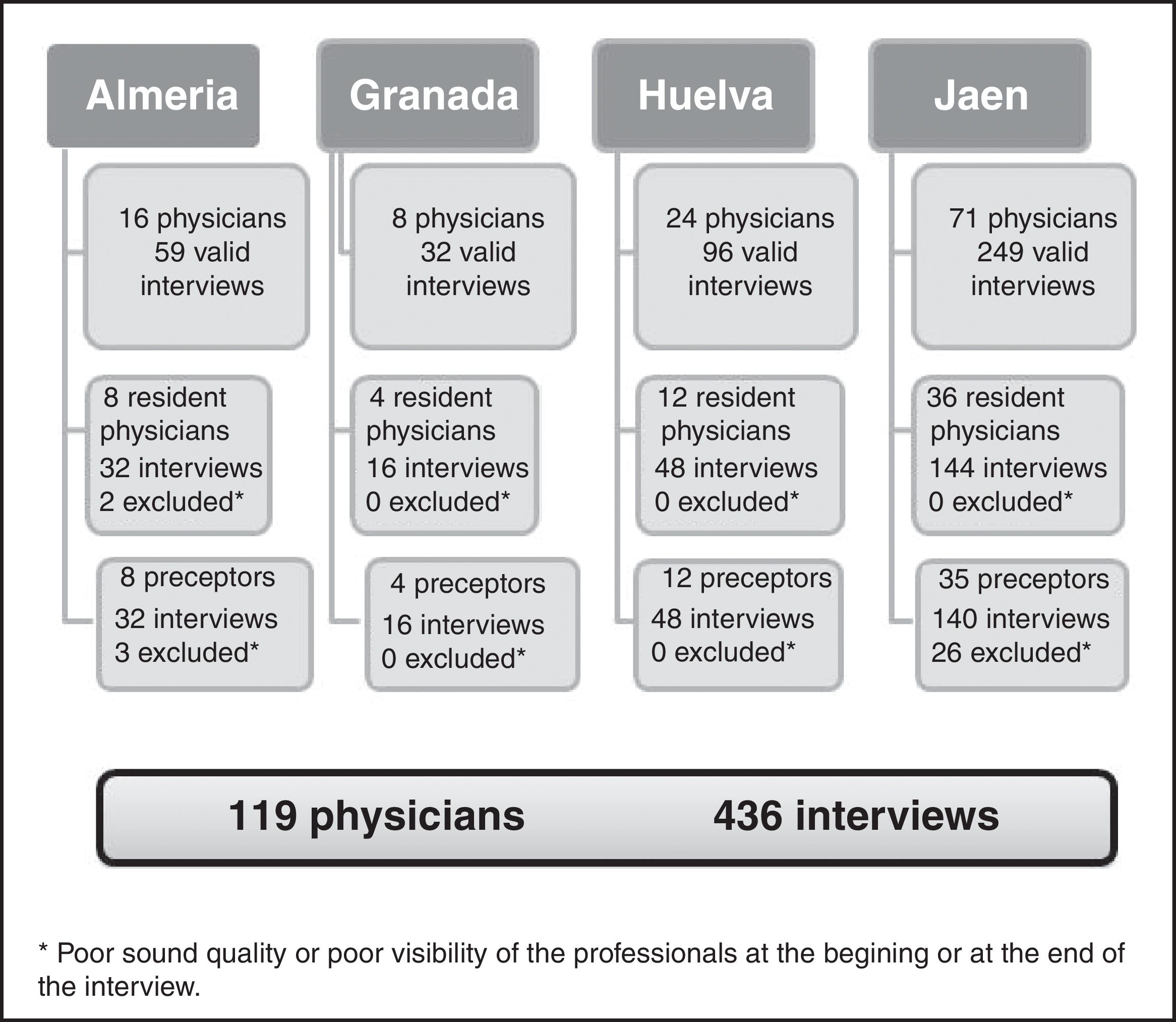
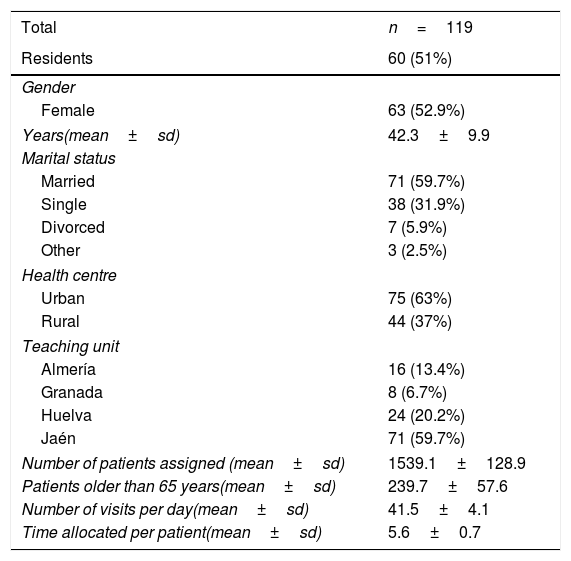
ResultsGeneral characteristics of the interviews and professionals analysedThere were 476 video recordings in total, excluding 40 due to technical difficulties. Of the 119 participants, 60 were residents (50.4%) with 229 interviews (52.5%) and 59 tutors with 207 interviews. The characteristics of physicians and interviews can be seen in Tables 1 and 2.
Characteristics of professionals.
| Total | n=119 |
|---|---|
| Residents | 60 (51%) |
| Gender | |
| Female | 63 (52.9%) |
| Years(mean±sd) | 42.3±9.9 |
| Marital status | |
| Married | 71 (59.7%) |
| Single | 38 (31.9%) |
| Divorced | 7 (5.9%) |
| Other | 3 (2.5%) |
| Health centre | |
| Urban | 75 (63%) |
| Rural | 44 (37%) |
| Teaching unit | |
| Almería | 16 (13.4%) |
| Granada | 8 (6.7%) |
| Huelva | 24 (20.2%) |
| Jaén | 71 (59.7%) |
| Number of patients assigned (mean±sd) | 1539.1±128.9 |
| Patients older than 65 years(mean±sd) | 239.7±57.6 |
| Number of visits per day(mean±sd) | 41.5±4.1 |
| Time allocated per patient(mean±sd) | 5.6±0.7 |
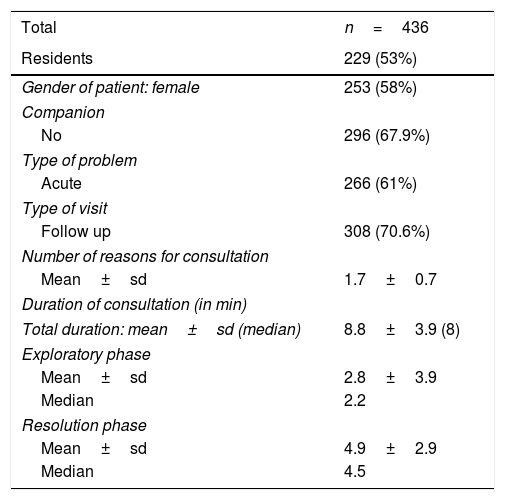
Characteristics of video recorded interviews.
| Total | n=436 |
|---|---|
| Residents | 229 (53%) |
| Gender of patient: female | 253 (58%) |
| Companion | |
| No | 296 (67.9%) |
| Type of problem | |
| Acute | 266 (61%) |
| Type of visit | |
| Follow up | 308 (70.6%) |
| Number of reasons for consultation | |
| Mean±sd | 1.7±0.7 |
| Duration of consultation (in min) | |
| Total duration: mean±sd (median) | 8.8±3.9 (8) |
| Exploratory phase | |
| Mean±sd | 2.8±3.9 |
| Median | 2.2 |
| Resolution phase | |
| Mean±sd | 4.9±2.9 |
| Median | 4.5 |
The average duration of consultations was 8.8min (sd: 3.86), with a median of 8min. Almost double the time was taken for the resolution phase than in the operative phase (Table 2).
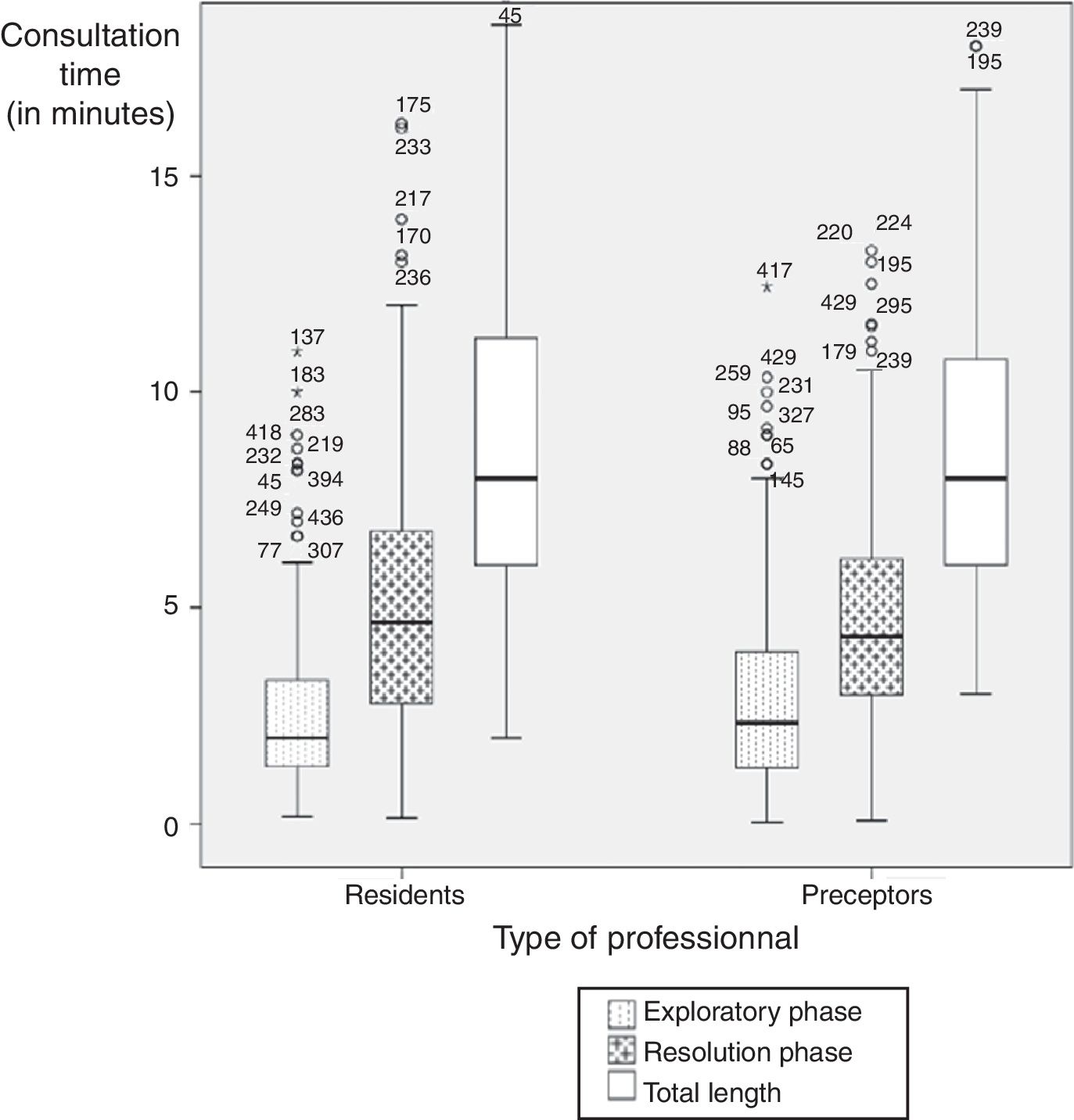
There are slight differences in consultation length between tutors and residents; however, tutors took longer in the exploratory phase of the interview, and residents took longer in the operative phase (Fig. 1).
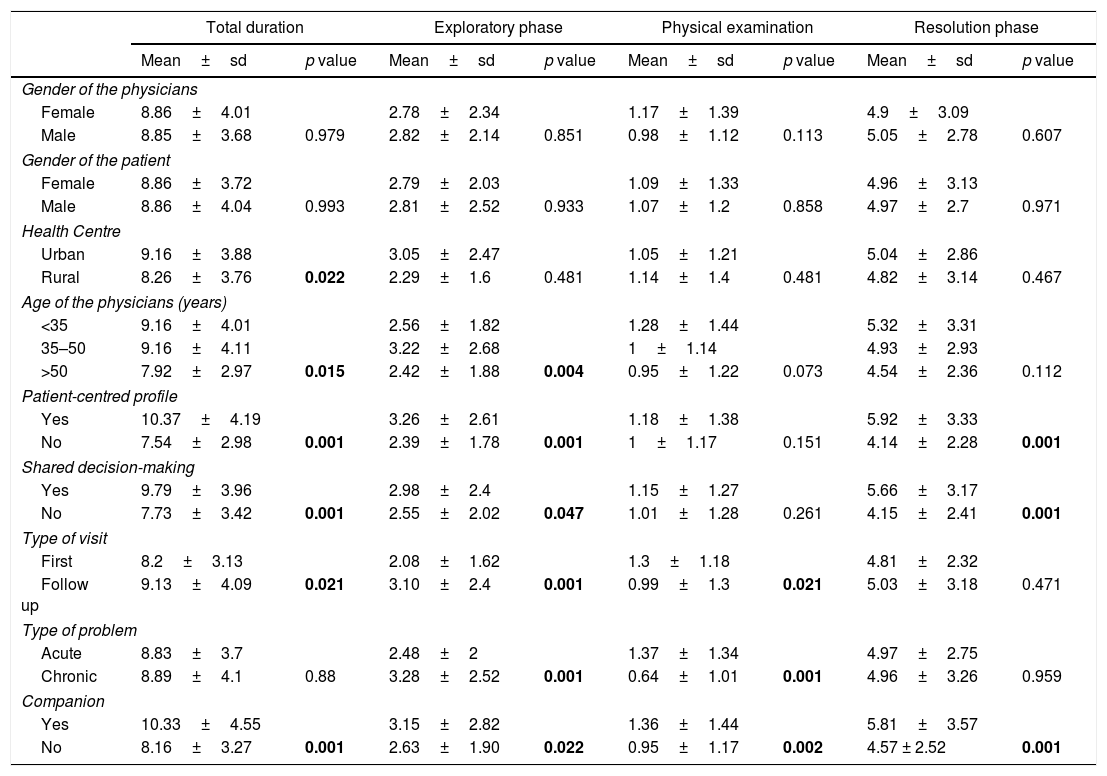
Variables relating to a longer consultationIn the bivariate analysis, a longer consultation length took place in urban centres, with younger professionals, those who had a patient-centred profile, when there was shared decision-making, in consultation reviews and when the patient was accompanied (Table 3).
Variables associated to a longer consultation.
| Total duration | Exploratory phase | Physical examination | Resolution phase | |||||
|---|---|---|---|---|---|---|---|---|
| Mean±sd | p value | Mean±sd | p value | Mean±sd | p value | Mean±sd | p value | |
| Gender of the physicians | ||||||||
| Female | 8.86±4.01 | 2.78±2.34 | 1.17±1.39 | 4.9±3.09 | ||||
| Male | 8.85±3.68 | 0.979 | 2.82±2.14 | 0.851 | 0.98±1.12 | 0.113 | 5.05±2.78 | 0.607 |
| Gender of the patient | ||||||||
| Female | 8.86±3.72 | 2.79±2.03 | 1.09±1.33 | 4.96±3.13 | ||||
| Male | 8.86±4.04 | 0.993 | 2.81±2.52 | 0.933 | 1.07±1.2 | 0.858 | 4.97±2.7 | 0.971 |
| Health Centre | ||||||||
| Urban | 9.16±3.88 | 3.05±2.47 | 1.05±1.21 | 5.04±2.86 | ||||
| Rural | 8.26±3.76 | 0.022 | 2.29±1.6 | 0.481 | 1.14±1.4 | 0.481 | 4.82±3.14 | 0.467 |
| Age of the physicians (years) | ||||||||
| <35 | 9.16±4.01 | 2.56±1.82 | 1.28±1.44 | 5.32±3.31 | ||||
| 35–50 | 9.16±4.11 | 3.22±2.68 | 1±1.14 | 4.93±2.93 | ||||
| >50 | 7.92±2.97 | 0.015 | 2.42±1.88 | 0.004 | 0.95±1.22 | 0.073 | 4.54±2.36 | 0.112 |
| Patient-centred profile | ||||||||
| Yes | 10.37±4.19 | 3.26±2.61 | 1.18±1.38 | 5.92±3.33 | ||||
| No | 7.54±2.98 | 0.001 | 2.39±1.78 | 0.001 | 1±1.17 | 0.151 | 4.14±2.28 | 0.001 |
| Shared decision-making | ||||||||
| Yes | 9.79±3.96 | 2.98±2.4 | 1.15±1.27 | 5.66±3.17 | ||||
| No | 7.73±3.42 | 0.001 | 2.55±2.02 | 0.047 | 1.01±1.28 | 0.261 | 4.15±2.41 | 0.001 |
| Type of visit | ||||||||
| First | 8.2±3.13 | 2.08±1.62 | 1.3±1.18 | 4.81±2.32 | ||||
| Follow up | 9.13±4.09 | 0.021 | 3.10±2.4 | 0.001 | 0.99±1.3 | 0.021 | 5.03±3.18 | 0.471 |
| Type of problem | ||||||||
| Acute | 8.83±3.7 | 2.48±2 | 1.37±1.34 | 4.97±2.75 | ||||
| Chronic | 8.89±4.1 | 0.88 | 3.28±2.52 | 0.001 | 0.64±1.01 | 0.001 | 4.96±3.26 | 0.959 |
| Companion | ||||||||
| Yes | 10.33±4.55 | 3.15±2.82 | 1.36±1.44 | 5.81±3.57 | ||||
| No | 8.16±3.27 | 0.001 | 2.63±1.90 | 0.022 | 0.95±1.17 | 0.002 | 4.57 ± 2.52 | 0.001 |
Values in bold are statistically significant.
A correlation between duration of the consultation and the number of reasons for the consultation was also found (r=0.353; p<0.001), with the professional's score obtained from the CICAA scale (r=0.420; p<0.01).
By contrast, consultation time was not related neither to the type of problem, neither with the gender of the doctor, the patient, nor with the doctor–patient gender interaction.
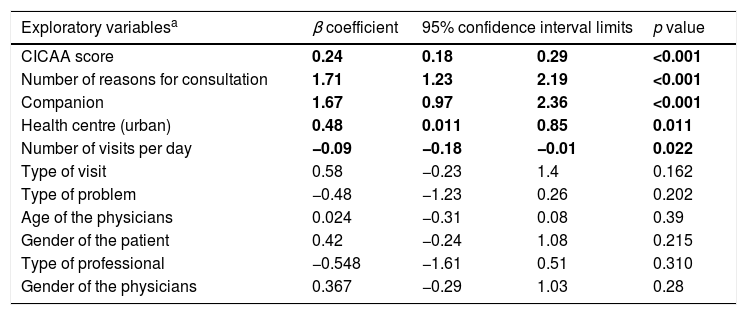
In the multivariate model, longer consultations were associated with better CICAA scores, a greater number of reasons for the consultation, if the patient was accompanied, the health centre type (urban), and less daily consultations (Table 4). The coefficient of determination (r2) was 0.32.
Final multiple linear regression model for consultation time.
| Exploratory variablesa | β coefficient | 95% confidence interval limits | p value | |
|---|---|---|---|---|
| CICAA score | 0.24 | 0.18 | 0.29 | <0.001 |
| Number of reasons for consultation | 1.71 | 1.23 | 2.19 | <0.001 |
| Companion | 1.67 | 0.97 | 2.36 | <0.001 |
| Health centre (urban) | 0.48 | 0.011 | 0.85 | 0.011 |
| Number of visits per day | −0.09 | −0.18 | −0.01 | 0.022 |
| Type of visit | 0.58 | −0.23 | 1.4 | 0.162 |
| Type of problem | −0.48 | −1.23 | 0.26 | 0.202 |
| Age of the physicians | 0.024 | −0.31 | 0.08 | 0.39 |
| Gender of the patient | 0.42 | −0.24 | 1.08 | 0.215 |
| Type of professional | −0.548 | −1.61 | 0.51 | 0.310 |
| Gender of the physicians | 0.367 | −0.29 | 1.03 | 0.28 |
Values in bold are statistically significant.
Before analysing the results, we must discuss possible limitations including voluntary sample selection. Although this is the method most frequently used in video-recorded studies20 is not exempt from possible selection bias, and may represent a subpopulation of more motivated professionals with a better communication profile.
Another difficulty would be behaviour change whilst being recorded; however it has been shown that this did not occur.20 In our work, recording a minimum of 1h is recommended, selecting multiple consultations of each professional and eliminating the first.
Regarding scale of measurement, there are many questionnaires to measure patient-physician communication, but only two that have been validated in Spain, one is the CICAA scale, which has certainly demonstrated its validity for this purpose.18,19
It has also been possible to produce a residual confounding bias as not having measured other variables probably related, among them, the reason for consultation.
Finally, this type of design of research studies does not allow establishing causal relationships between variables.
Time distribution during the consultationThe average consultation length in this study is around 9min, similar to that obtained by other authors in Spain.10,21 At European level, the average length is between 10 and 15min; according to Deveugele,4 shorter consultations occur in Germany and Spain with 7.6 and 7.8min respectively; in England and Holland duration is around 10min and in Belgium and Switzerland around 15min.
For some authors, consultation length should be around 20min to achieve an approach that includes encouraging a healthy lifestyle, detecting risk factors (hypertension, alcoholism, smoking), improving patient and professional satisfaction.1,2
There is no difference in the total consultation time between tutors and residents, although they distribute time differently, tutors spend more time on the exploratory phase, and residents are quicker in the anamnesis.
The bivariate analysis shows how older doctors perform shorter consultations, which was observed in resident physician training.22 However, after performing a multiple regression analysis, like other authors we have not found a relationship between consultation length and age of the physician.4
No differences in consultation length in relation to the gender of the professional were detected, unlike in other areas, where female medical staff took 2min longer than men, involving the patient in the consultation more.5,12–14 Although there are publications that describe an increase in quality of care and communication skills without increasing the consultation time,23,24 in this study, as in other studies,6,7,25,26 better communication (a higher CICAA score), patient involvement in decision-making or developing a patient-centred approach are factors that lengthen the consultation. It is inevitable, as several authors claim, that listening to the patient, and involving them in the process, would require more time.6,7,25,26
In urban centres, consultation length is increased, possibly because patients had more reasons for the consultation.4 It has been found that the more reasons the patient has for the consultation, the longer the duration due to the type of diagnosis the physician must give.4,5,8,27 The consultations due to psychological,4 gynaecological,5 social and psychosocial problems are usually longer than strictly biomedical consultations.8,28
As Hutton and Gunn8 noted, follow up consultations related to the elderly or patients with chronic conditions, were also associated in our study with a longer consultation. Although, the gender of the physician was not determinative, and neither was the gender of patient. However, other authors have found that consultations with female patients tended to be longer, especially if the physician was also female.4,5
Whether the patient was accompanied also affected consultation length. Although not included in our study, other authors also point out how increased query time is associated with age and type of ailment, possibly because of the greater complexity in ailments of the elderly.11
Pressure is an external factor to the professional (although sometimes the result of inappropriate clinical management21,28,29) which in our study was associated with a shorter consultation. It seems logical that more patients per day would mean a shorter duration. However, when communication is analysed, often such external factors are not considered, including other factors related to the patient, such as prior knowledge of them or their family.30
Lastly, all features and factors included in the multiple regression model explain 32% of the time variability in the consultation, thus leaving two-thirds unexplained. Deveugele et al.4 investigated the average consultation time in 6 European cities and the influencing factors. Factors relating to the physician and the country accounted for 22% and 23% of the variance of consultation length, whereas patient characteristics accounted for 55%.
ConclusionBetter communication (a higher CICAA score), a patient-centred physician and shared decision-making is associated with increased consultation length. There is also a proven correlation between multivariate analysis and the number of reasons for the consultation, whether the patient is accompanied, the urban health centre and a smaller workload.
Practical applicationAn average consultation length should be established, with recommended standards figures as it has been found allowing more time improves relationships between physicians and patients, and consequently the health of citizens.
Consultation length in primary care is affected by variables that are not always controllable by the professional, such as a heavy workload, often caused by a lack of resources.
To better define the relationship between patient communication and consultation time, in future research it would be interesting to incorporate the perceptions of professionals and the point of view of patients, as well as the results of the consultation, in terms of patient satisfaction and health.
FundingThis study was subsidised by a research grant from the Junta de Andalusia (Regional Government of Andalusia) File 0726-2010.
The appropriate length of a consultation is a controversial issue.
There are wide differences in duration of consultations between countries
A shorter consultation may be associated with professional malpractice.
What has this study contributedA consultation focused on the patient and a patient involvement in decision-making, is associated with a longer consultation time.
Patients who come with a companion and have a greater number of demands, are associated with a longer duration of the consultation.
Greater care pressure is associated with shorter consultations.
The authors declare there is no conflict of interest.
The work was presented as a research project to the XVI Wonca Europe Conference that took place in Malaga, Spain, from the 6th to the 9th of October 2010. The preliminary results were presented in the Thematic Conference World Psychiatric Association (WPA) that took place in Granada, Spain from the 8th to the 12th of February 2012. The first part of the study was published in: Valverde Bolívar FJ, et al. Communication skills of tutors and family medicine physician residents in Primary Care clinics. Aten Primaria. 2016;48(10):632–41 (http://dx.doi.org/10.1016/j.aprim.2015.12.002).