Abstracts Asociación Mexicana de Hepatología (AMH) 2024
More infoTwenty-five years after the discovery of the hepatitis C virus (HCV), it is the chronic infection with the greatest impact on diagnosis and treatment. The objective of this study is to describe the simplification of HCV management for a cohort of 270 patients evaluated from 2018 to 2023.
Materials and PatientsA prospective cohort study was carried out to evaluate patients with HCV (Ac vs HCV +). In 2018 we had direct-acting antivirals (DAA) to treat HCV genotype 1; in addition to the HCV viral load (HCV RT-PCR), we required the viral genotype and liver elastography, 2019 we already had pan-fibrotic pangenotypic schemes, so genotype and liver elastography were excluded; however, due to the capacity of HCV to infect lymphocytes, screening prior to treatment with DAAs for diabetes, kidney disease, thyroid disease, rheumatic musculoskeletal disease, and associated proliferative disorders continues to be necessary. To B lymphocytes and in patients with cirrhosis determination of alpha fetoprotein (AFP) and liver ultrasound. In the clinical presence of cutaneous purpura, determination of cryoglobulins, rheumatoid factor and complement fractions, in addition to excluding coinfections with the Hepatitis B Virus and the human immunodeficiency virus. In the initial assessment, the risk factors for HCV were obtained by questioning. Patients who received treatment were evaluated every month during the months of treatment and the sustained viral response 12 weeks after completing treatment (SVR12) and every 6 months thereafter.
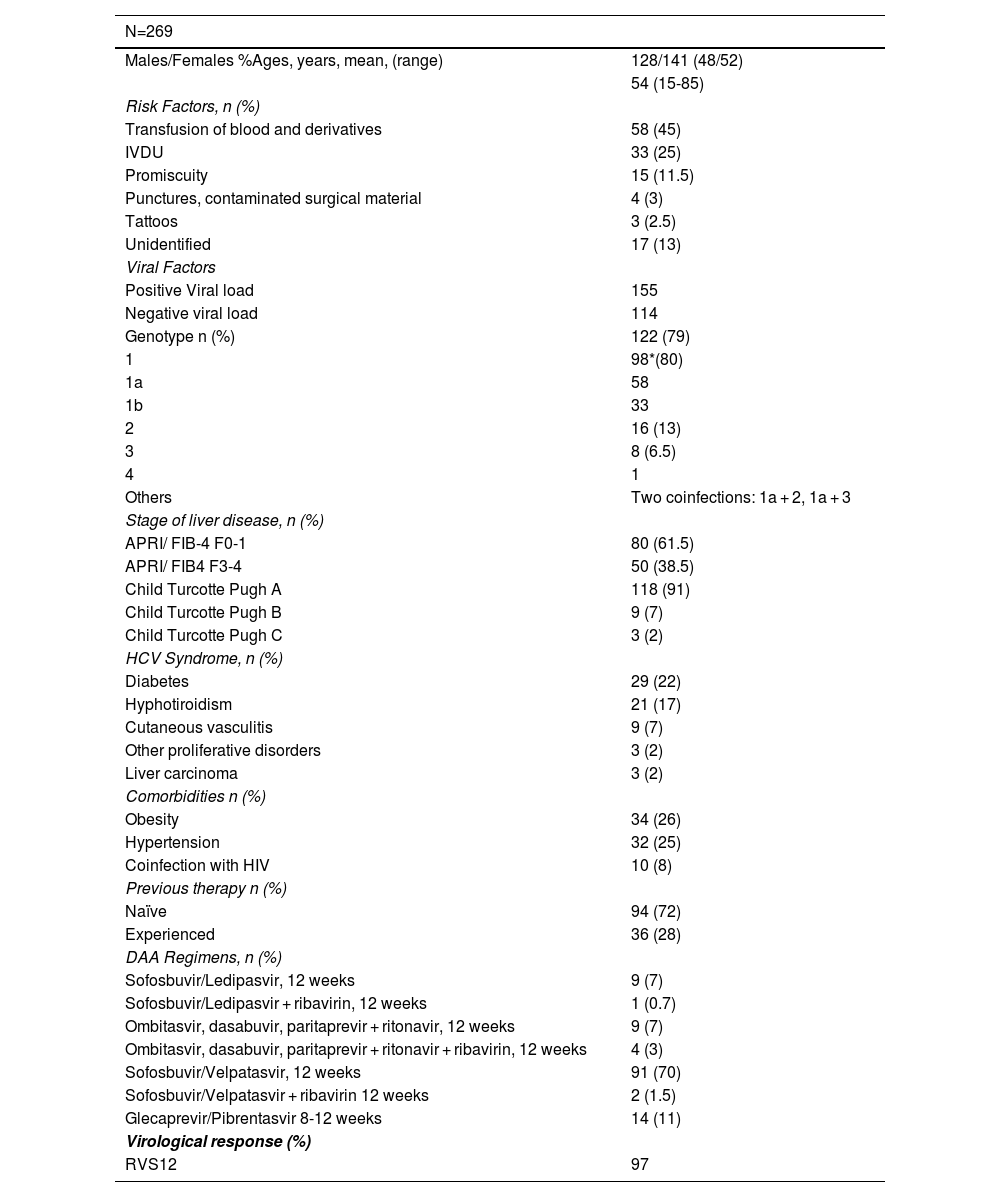
Results269 patients with chronic HCV infection were included, sent from 11 first-level medical units and 3 second-level hospitals in Northeast Mexico. 53% were women with an average age of 54 years. The main risk factor identified was blood transfusion followed by intravenous drug use (IVDU). 28% had previous treatment with pegylated interferon and ribavirin. 30% had compensated cirrhosis. Fibrosis was calculated using the APRI algorithm, finding 53/130 with >1.5 and 60/130 with >3.25, which predicted F3-4. Liver elastography was performed in 55/130 patients, with 37 at F3-4. Among the diseases possibly related to chronic HCV infection we found 29 diabetes, 21 hypothyroidism, 9 cutaneous vasculitis with cryoglobulins, 1 diffuse large cell non-Hodgkin lymphoma, 1 monoclonal gammopathy of uncertain origin, 1 chronic lymphocytic leukemia and 3 cases of hepatocellular carcinoma., a patient with HCV relapse in a transplanted liver. Of these, 155 (58%) presented positive HCV RT-PCR with genotype 1 in 80% of the patients. 130 (84%) received treatment, the most used regimens were those based on sofosbuvir with SVR12 in 97% (Table 1).
ConclusionsThe diagnostic approach and treatment of chronic HCV infection has been simplified with the rapid test for detection and mainly due to the safety of the new treatments, DAAs, since these have proven to be safe and highly effective in the heterogeneous population that suffers from this infection.
Ethical statement: Approval was obtained from the ethics and research committee of our hospital.
Declaration of interests: None.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Baseline characteristics of patients included
APRI: Aspartate Aminotransferase to Platelet Ratio Index, FIB-4: Fibrosis-4 Index, HCV: Hepatitis C Virus, DAA: Direct-Acting Antiviral, RVS12: Sustained Virological Response at 12 weeks, IVDU: Intravenous Drug Use.