Abstracts of the 2025 Annual Meeting of the ALEH
More infoThe MELD 3.0 score has demonstrated superior discriminatory performance for predicting 90-day waitlist mortality among liver transplant (LT) candidates in the US. This study aimed to validate the MELD 3.0 in a Latin American cohort.
Materials and MethodsRetrospective cohort study including adults LT candidates listed between 2016-2023 across five Latin American countries. Baseline data were registered at listing. Cox regression model was performed, with 90-day mortality as the primary outcome and LT as censored observation. Discriminative performance was assessed using Harrell´s c-index for MELD, MELD-Na and MELD 3.0. Net Reclassification Index (NRI) was also calculated.
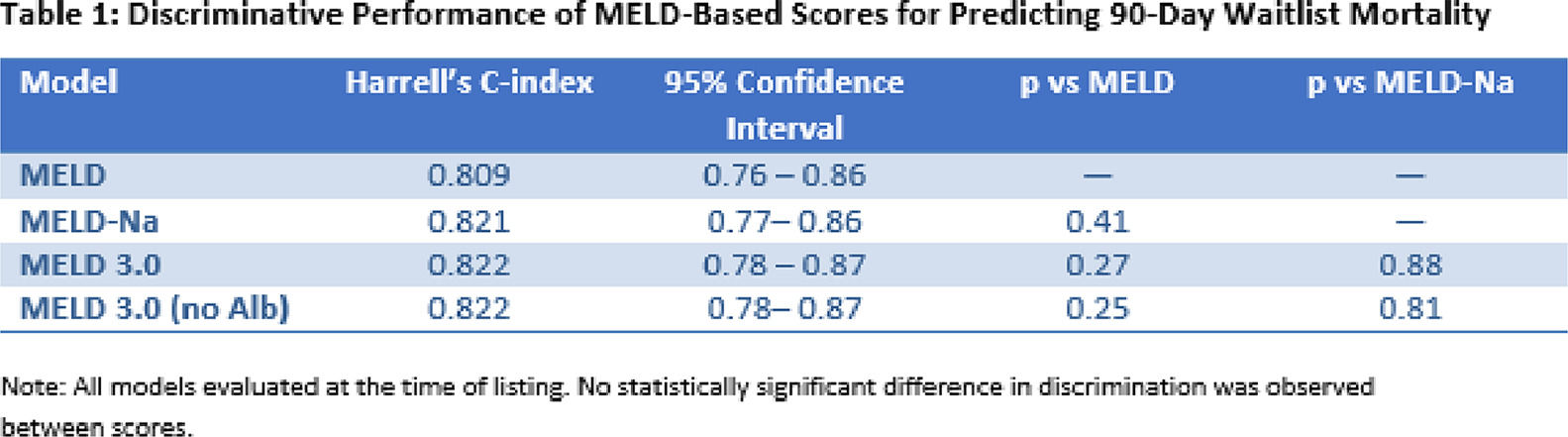
ResultsWe included 1,013 patients: mean age 51 years (±11.8); 41.4% females, 25.8% obese, 58.1% ascites and 38.3% had encephalopathy were present in 58.1% and 38.3% of cases, respectively. Median MELD score was 16.9 (IQR 13.3–21.1), MELD-Na 18.3 (IQR 14.6–24), and MELD 3.0 19.5 (IQR 15.1–24.8). At 90 days, 26.3% underwent LT and 66.8% remained on the waitlist. The mortality incidence was 29.4 deaths per 1,000 patient-months, with a cumulative mortality of 8.3% (95% CI 6.6–10.4%) at 3 months. Hazard ratios for 90-day mortality were: MELD 1.15 (95% CI 1.12-1.19), MELD-Na 1.16 (95% CI 1.13-1.20), and MELD 3.0 1.15 (95% CI 1.12-1.19). Harrell’s c-index showed no significant differences (Table 1).NRI showed no significant improvement in risk reclassification using MELD 3.0.
ConclusionsIn a region showing high waitlist mortality, MELD 3.0 did not demonstrate superior predictive performance over MELD or MELD-Na. These findings highlight the need for regional validation of predictive models before implementation in transplant priorization policies.