Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related deaths worldwide, following lung and colorectal cancers [1]. Recent estimates indicate that it is the sixth most diagnosed cancer and the second most leading cause of premature cancer-related deaths globally [2].
Over the past two decades, the epidemiology of HCC has shifted significantly, with incidence and mortality trends varying substantially across different countries [3,4]. The causes of HCC have also evolved over time. Historically, chronic viral hepatitis (hepatitis B and C) was the predominant contributor to HCC, but this is gradually changing. This shift is partly attributable to the availability of highly effective antiviral therapies for chronic hepatitis and the widespread implementation of HBV vaccination in routine childhood immunization programs [5]. At the same time, rising sedentary lifestyles and the adoption of Western diets have contributed to an increase in metabolic syndrome and obesity [6]. As a result, metabolic dysfunction–associated fatty liver disease (MAFLD) has emerged as a leading cause of chronic liver disease and cirrhosis worldwide, including in the Arab region, and its impact on HCC is likely to grow given the paucity of specific treatments [7,8].
In the Arab region, which comprises 22 countries with approximately 500 million people, there has been an alarming rise in obesity and metabolic disorders, with dramatic increases in MAFLD prevalence in recent years [9–11]. However, high-quality epidemiological studies on HCC in Arab populations remain limited, impeding the development of effective region-specific health policies and cancer control strategies [12]. Analyzing the burden and trends of HCC in these countries is crucial for guiding targeted prevention and early detection efforts where they are needed most. Therefore, this study aims to examine the epidemiology and changing profile of HCC in the Arab region by analyzing incidence, mortality, and etiological trends from 1990 to 2021 using the Global Burden of Disease (GBD) 2021 dataset.
2Materials and Methods2.1Data sourceThis analysis assesses the burden of HCC in Arab countries using data from GBD 2021, a comprehensive global initiative covering 371 diseases across 204 territories and nations [13]. The GBD study gathers cancer data from multiple sources, with vital registration systems contributing the majority, alongside cancer registries and, in certain instances, verbal autopsy reports. This comprehensive data collection aims to capture cancer incidence, mortality, and associated burden across various regions and countries. The information is then utilized to calculate metrics that evaluate the overall impact of cancer on populations. Data regarding HCC burden, including prevalence, incidence, mortality, and disability-adjusted life years (DALYs), have been compiled for 22 countries in the Arab region. This information was obtained from the Data Input Sources Tool (http://ghdx.healthdata.org/gbd-results-tool), an online resource managed by the Institute for Health Metrics and Evaluation, which is part of a global partnership providing extensive health-related data [14]. The main goal of this analysis is to quantify the disease burden of HCC in the Arab region.
2.2Definitions and measuresIn the GBD dataset, HCC is defined using the International Classification of Disease (ICD) Version 10 codes for primary HCC (ICD-10 C22). For each disease burden indicator- incidence, prevalence, mortality, and DALYs data were collected as both crude and age-adjusted rates per 100,000 population. The incidence rate represents the number of newly diagnosed HCC cases in a year per 100,000 individuals. The prevalence rate refers to the total count of patients with HCC, including both new and existing cases, in a year per 100,000 individuals. The mortality rate refers to the number of deaths caused by HCC in a year per 100,000 individuals. DALYs, which quantify total health loss, are calculated by summing the years of life lost to premature mortality (YLL) and the years of life lived with disability (YLD). Age adjustment involves multiplying age-specific disease rates by age-specific weights, representing the population proportion within each age group. These weighted rates are totaled across age groups to produce the age-adjusted rate. We also conducted a subgroup analysis based on etiology, age, and gender.
2.3Ethics statementThis study utilized publicly available, aggregated, and de-identified data from the GBD 2021 study. As such, ethical approval was not required because the analysis was based on pre-existing, de-identified data available in the public domain.
3Results3.1Prevalence of HCCIn 2021, HCC affected approximately 0.74 million individuals globally, including 23,340.63 in the Arab region, representing about 3.2 % of the global burden. Egypt reported the largest absolute burden, with 13,567.26 cases in 2021, followed by Iraq with 1352.15 cases. The lowest prevalence was in Djibouti (40.39) and Comoros (29.49).
In 2021, Mauritania exhibited the highest age-standardized prevalence rate (ASPR) (20.9; 11.13–30.3), closely followed by Egypt (19.28; 15.04–24.02) and Qatar (15.77; 11.7–21.47), which was more than twice the global average (8.68; 7.9–9.67). While the lowest ASPR was reported in Kuwait (1.36; 1.1–1.63) and Morocco (0.59; 0.43–0.77) (Table 1).
Age-standardized rates for 1990, 2021 and the annual rate of change (1990–2021) for various parameters in Arab countries.
Abbreviation: DALYs, disability-adjusted life years.
Examining the estimated annual percentage change (EAPC), Libya recorded the most rapid increase in prevalence at 1.17 %, the highest in the region, followed by Qatar at 1.09 %. Conversely, Kuwait at −4.11 %, Mauritania at −2.28 %, and Bahrain at −1.44 % experienced the steepest declines (Table 1).
3.2Incidence of HCCIn 2021, over 0.5 million new cases of HCC were reported worldwide, with approximately 19,000 cases from the Arab countries, which accounted for about 3.6 % of the global burden. Egypt reported the highest incidence, with 11,520.87 new cases in 2021, followed by Iraq with 1091.72 cases. The lowest incidence was in Djibouti (29.78) and Comoros (23.20).
Incidence trends of HCC in Arab countries exhibited significant regional variability. In 2021, Mauritania reported the highest age-standardized incidence rate (ASIR) at 19.13 per 100,000 (10.18–27.93), followed closely by Egypt (18.37; 14.37–22.85) and Qatar (14.42; 10.59–19.5), which was more than twice the global level (6.15; 5.58–6.9). Similar to prevalence, Kuwait (1.14; 0.92–1.37) and Morocco (0.51; 0.36–0.65) reported the lowest ASIR among Arab countries (Fig. 1).
The fastest-growing EAPC of incidence rates was observed in Libya (1.03 %) and Algeria (0.92 %). Conversely, Kuwait (−4.02 %) and Mauritania (−2.22 %) exhibited the steepest declines (Table 1).
3.3Mortality of HCCIn 2021, there were nearly 0.5 million HCC-related deaths globally, 19,261.89 occurred in Arab countries, comprising 4.0 % of the global HCC-related deaths. Egypt reported the highest mortality, with 11,778.37 deaths in 2021, followed by Iraq with 1110.96 deaths. The lowest mortality was in Kuwait (30.15) and Comoros (24.27).
At the country level, the age-standardized mortality rate (ASMR) for HCC was disproportionately high in Mauritania (20.59; 10.96–29.93), followed by Egypt (19.73; 15.42–24.47), which was >4 times higher than the global level (5.65; 5.13–6.30). The lowest ASMR were reported in Morocco (0.54; 0.38–0.68), followed by Kuwait (1.18; 0.94–1.42) (Table 1).
The fastest-growing EAPC of mortality rates were observed in Libya (0.99 %) and Algeria (0.91 %). Conversely, Kuwait (−4.01 %) and Mauritania (−2.17 %) exhibited the steepest declines (Table 1). Sex-specific differences exist, as EAPC of mortality rates was generally higher in males than in females across all Arab countries in this period, with the highest rate observed in Libya (1.43) and Egypt (1.17). Notably, the UAE was the only country in the region that showed an opposite trend with higher EAPC of mortality rates in females compared to males (1.23 % vs 0.43 %, respectively) (Supplementary Table 1).
3.4Disability-adjusted life years (DALYs) attributable to HCCGlobally, HCC-related DALYs in 2021 were estimated at 12,887,652.41, while in Arab countries, they totalled 560,889.26. Egypt reported the highest DALYs at 336,288.49, followed by Iraq with 31,796.39. The lowest DALYs were found in Kuwait (818.27) and Comoros (720.00).
In 2021, Mauritania had the highest ASR-DALYs (528.98; 278.29–775.2), followed by Egypt (476.58; 368.6–598.29) and Qatar (317.75; 234.94–430.8), which are more than twice the global level of 149.29 (135.24–167.48). Kuwait (25.58; 20.47–31.11) and Morocco (14.29; 10.11–18.46) reported the lowest rates among the Arab countries (Table 1).
Similarly, Libya experienced the most significant EAPC increase of ASR-DALYs (0.93 %), followed by Algeria (0.62 %). Conversely, Bahrain (−1.93 %), Mauritania (−2.47 %), and Kuwait (−4.66 %) saw the most declines in ASR-DALYs, possibly reflecting improvements in early-stage disease identification and management.
3.5EtiologyIn 2021, new HCC cases in Arab countries (18,943.59 total) showed a distinct etiology compared to global trends: Hepatitis C virus (HCV) predominated (48.1 % vs. 29.1 %), while HBV was less frequent (23.0 % vs. 38.9 %), alcohol played a lesser role (9.3 % vs. 18.8 %), and MAFLD contributed proportionally more (12.2 % vs. 9.7 %).
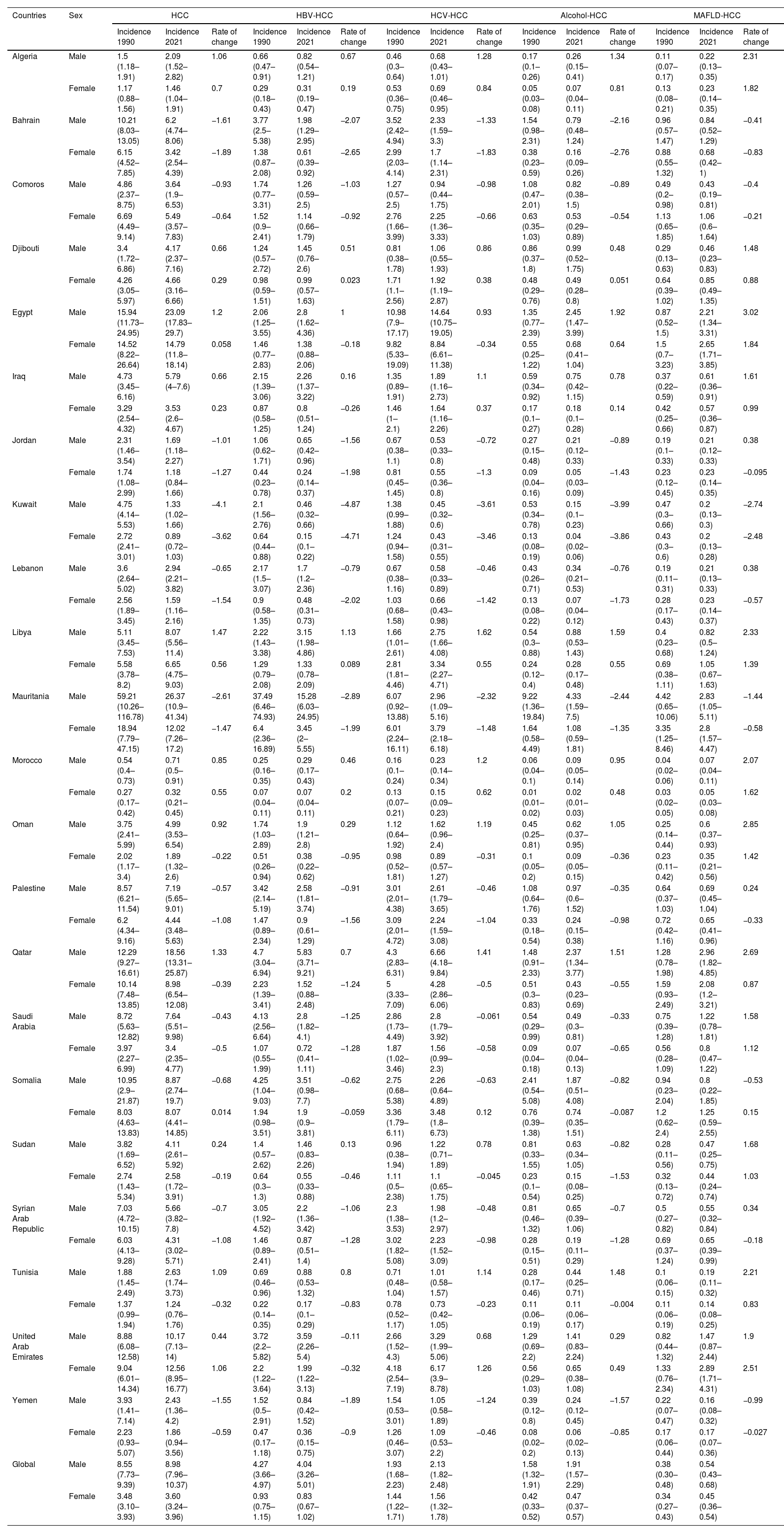
The ASIR from 1990 to 2021 revealed a drastic change in HCC profile across Arab countries (Table 2). While most countries experienced decreases in HBV and HCV-related HCC incidence, notable exceptions include Libya and Algeria, which continued to see a rapid increase in both EAPC. The rates of decline varied, with Kuwait and Mauritania exhibiting the most significant decreases in HBV and HCV-related HCC.
Age-standardized rates of incidence for 1990 and 2021 and the annual rate of change (1990–2021) for various etiologies of HCC in Arab countries.
Abbreviations: HCC, Hepatocellular Carcinoma; HBV, Hepatitis B Virus; HCV, Hepatitis C Virus; MAFLD, Metabolic Dysfunction-Associated Fatty Liver Disease.
Regarding alcohol-related HCC, the majority of countries also showed decreasing incidence rates, and most countries reported significantly lower levels compared to the global average (1.14; 0.93–1.38). Only Mauritania (2.71; 1.26–4.52), Egypt (1.61; 0.97–2.58), Qatar (1.57; 0.91–2.49), and the United Arab Emirates (1.23; 0.73–1.89) reported higher levels than the global average.
In contrast, MAFLD-related HCC incidence generally increased across the region. Except for Djibouti, MAFLD exceeds alcohol consumption, making it the third leading cause of HCC. Mauritania (2.81; 1.51–4.44), Qatar (2.53; 1.57–3.96), and Egypt (2.24; 1.41–3.28) reported significantly higher incidence levels than the global average (0.49; 0.40–0.60). Additionally, virtually all the Arab countries showed increased EAPC, with Oman experiencing the most significant EAPC increase in ASIR (2.24 %), followed by Egypt (2.15 %) and Algeria (2.05 %) (Fig. 2).
The age-standardized mortality rates from 1990 to 2021 reveal trends in HCC etiologies across Arab countries (Table 3) that largely mirrored those observed for incidence. While most countries experienced decreases in HBV and HCV-related HCC mortality, notable exceptions include Libya (0.68 %, 1.01 %) and Algeria (0.5 %, 1.04 %), which still saw an increase. The rates of decline varied, with Kuwait (−5.07 %, −3.53 %) and Mauritania (−2.63 %, −1.82 %) exhibiting the most significant decreases in HBV and HCV-related HCC mortality. Regarding alcohol-related HCC mortality, the majority of countries also showed decreasing rates, and most countries reported significantly lower levels compared to the global average (1.06; 0.86–1.29). Only Mauritania (2.94; 1.38–4.9), Egypt (1.71; 1.03–2.72), Qatar (1.63; 0.94–2.59), and the United Arab Emirates (1.33; 0.78–2.05) reported higher levels than the global average. MAFLD-related HCC mortality generally increased across the region, with Mauritania (3.13; 1.66–4.95), Qatar (2.68; 1.65–4.21), and Egypt (2.42; 1.5–3.54) reporting significantly higher mortality levels than the global average (0.48; 0.39–0.58). Furthermore, almost all the Arab countries showed increased EAPC, with Oman experiencing the most significant EAPC increase in ASMR (2.17 %), followed by Egypt (2.09 %) and Algeria (2.02 %). Similar results were discerned in an analysis stratified by gender, with mortality rates generally higher in males compared to females across the different etiologies (Supplementary Table 1).
Age-standardized rates of mortality for 1990 and 2021 and the annual rate of change (1990–2021) for various etiologies of HCC in Arab countries.
Abbreviations: HCC, Hepatocellular Carcinoma; HBV, Hepatitis B Virus; HCV, Hepatitis C Virus; MAFLD, Metabolic Dysfunction-Associated Fatty Liver Disease.
The ASIR in 1990 and 2021, stratified by gender and etiology is depicted in Table 4. Overall, males exhibited higher incidence rates of HCC compared to females. Notably, the United Arab Emirates was the only country that has a faster EAPC for females than for males. Several countries, including Algeria, Egypt, Libya, Morocco, and the United Arab Emirates, experienced increases in overall HCC incidence in both males and females. In contrast, Kuwait, Mauritania, and Bahrain saw significant declines in overall HCC incidence across both genders.
Age-standardized incidence rates of liver cancer in 1990 and 2021 based on the gender and etiology in Arab countries.
Abbreviations: HCC, Hepatocellular Carcinoma; HBV, Hepatitis B Virus; HCV, Hepatitis C Virus; MAFLD, Metabolic Dysfunction-Associated Fatty Liver Disease.
In 2021, the morbidity and mortality rates of HCC in the Arab region exceeded the global average, based on the GBD 2021 study. From 1990 to 2021, there was a consistent decline in the occurrence and death rates of HCC due to HBV and HCV, while there was an increase in cancer caused by alcohol use and MAFLD [4]. The burden as well as the main reasons for HCC related mortality and morbidity varied substantially across regions and exhibited gender bias [15].
In this study, we report a significantly declining HCC-specific mortality in the Arab region during 1990–2021, with continuously declining incidence and improved survival. The highest decline in HCC mortality rates has been observed in Kuwait (−4.01 %), while the highest increase was in Libya (0.99 %). These findings reflect ongoing efforts in the prevention, early detection, and treatment of HCC.
The profile of liver diseases in the Arab region is evolving, and viral hepatitis is declining, while fatty liver disease is increasing dramatically [16]. However, the impact of these changes on the profile of HCC remains uncertain. In this work, we discerned that though it still represents the underlying cause for the vast majority of HCC cases in the region, the trend of HBV and HCV related HCC is declining from 1990 to 2021. The largest decline was observed in Kuwait (−5.07 %, −3.53 %), while Algeria still reported increases (0.5 %, 1.04 %).
Historically, various countries in the Arab region, particularly Egypt, are classified as high-prevalence locations for HCV. Egypt has launched one of the most impressive and widespread national programs for HCV testing and treatment over the last decade, accompanied with wide availability of direct anti-viral drugs [17]. Similar programs have been adopted in virtually all countries in the region, which should have an impact on the decline of complications associated to HCV [18].
With the introducing the hepatitis B vaccine for infants countrywide across the regions, significantly increasing the hepatitis B immunization rate for newborns, subsequently substantially reducing the risk of HBV-related HCC [19]. This pattern indicates the need for a free catch-up HBV vaccination program, more active case detection of HBV patients, and viral load management.
We found that the absolute numbers and rates of MAFLD-related HCC incidence, mortality, and DALY significantly increased from 1990 to 2021, with the highest rate of increase seen in Oman (2.17 %) and the lowest in Kuwait (−2.65 %). The HCC linked to MAFLD represents between 7.2 % (Yemen) to 16.2 % (Saudi Arabia) of HCC cases in the Arab region in 2021. The Arab region has one of the highest prevalences of MAFLD, which increases even among children and young adolescents, further emphasising the urgent need for comprehensive approaches for combating the growing MAFLD burden to prevent the future surge of MAFLD-related HCC [20–22].
The HCC profile and pattern of changes in HCC features over the course of the last 3 decades are another important finding of this work. Though the HCC pattern still displays a gender bias, being more prominent among males, notably this disparity is blunted for MAFLD-related HCC, which shows almost equal rates in males and females. This concerning observation implies that the systemic metabolic milieu predisposing to MAFLD-related HCC is likely overcoming the gender protective effect in females, mainly attributed to a hormonal basis and less exposure to classical risk factors such as smoking, pollution and alcohol [23]. Consistently, a recent study showed that among all primary malignancies between 2008 and 2017, HCC had the biggest annual percentage increase in incidence among women worldwide [24].
A recent research on the Asia-Oceania region, also utilizing the GBD 1990–2021 dataset, reports a similar shifting profile in the etiology of HCC [25]. It highlighted a decline in viral hepatitis-related HCC, coupled with a rapid increase in MAFLD-related cases, which aligns with our findings. Moreover, evidence from liver transplant data indicates that MAFLD has become the fastest-growing cause of HCC among recipients and candidates on the waiting list in the United States, with comparable trends observed over the past 20 years in Europe, South Korea, and Southeast Asia [26–29]. This consistency suggests that the transition from viral to metabolic etiologies may be a widespread, possibly global, phenomenon, reflecting the success of viral hepatitis control measures alongside the emerging challenge of metabolic syndrome worldwide.
Some limitations of our study must be acknowledged. First, there are limited data sources in developing countries and populations, necessitating epidemiological studies that concentrate on standardized age groups. Second, the specific etiologies in different countries, when interpreting the findings, readers should consider the perspectives of informants in different countries when interpreting the results to ensure a comprehensive understanding of the disease patterns and trends.
Continued research and targeted interventions are essential to further reduce the burden of HCC in the Arab region. Future research should focus on expanding data collection efforts across the region, as well as incorporating more standardized age groups and multimorbidity tracking. This will help improve the accuracy and generalizability of epidemiological studies on HCC, ultimately informing more effective public health interventions. Moreover, efforts should be made to strengthen surveillance infrastructure in countries with limited healthcare resources to enhance disease tracking and early detection of HCC cases. Collaboration between international organizations, governments, and local healthcare providers is essential to build robust surveillance systems and ensure timely reporting of data [30]. By tailoring interventions to the specific needs of different geographic areas, healthcare providers can better address the unique challenges of HCC prevention and management in diverse populations [12].
We observed generally consistent trends between HCC prevalence, incidence, mortality and DALYs across the Arab countries. This is likely due to similarities in risk factor profiles, such as high rates of metabolic syndrome and shared exposure to hepatitis viruses [31,32]. Additionally, similarities in healthcare systems and access to treatment may contribute to correlated mortality and DALYs trends [33]. However, variations in data quality across countries should also be considered. While a formal correlation analysis is beyond the scope of this study, it would provide a more comprehensive understanding of the HCC burden and guide targeted interventions. Future research could explore these relationships more rigorously.
5ConclusionsIn conclusion, our analysis of GBD 2021 data highlights that many areas of the Arab region experience a disproportionately high burden of HCC, with incidence and mortality rates often surpassing global averages. While the past three decades have seen successful regional efforts to reduce HCC cases related to viral hepatitis B and C, these achievements are being countered by a troubling increase in MAFLD-related HCC, driven by the growing prevalence of metabolic risk factors in these countries [27,29]. This shifting etiological landscape also has distinct gender implications, as the previously significant male predominance in HCC is decreasing for metabolically driven diseases. Together, these findings underscore the pressing need for comprehensive public health strategies tailored to the distinct epidemiological profiles of each Arab country. Priority should be given to addressing the growing epidemic of MAFLD through widespread lifestyle interventions, early identification of at-risk individuals, and enhanced clinical surveillance, while maintaining progress in managing viral hepatitis to prevent a resurgence of infection-related HCC [34]. Further research is needed to refine our understanding of HCC risk factors among different Arab subpopulations and to develop optimized, tailored interventions, including surveillance and treatment approaches, that can effectively reduce HCC incidence and improve outcomes. By proactively addressing these multifaceted challenges, the Arab region can strive to reduce the rising tide of HCC and ultimately enhance liver cancer–related survival for its populations.
None.