The aim of this study is to describe the experience of a tertiary referral centre in Portugal, of the placement of BAHA in children.
MethodsThe authors performed a retrospective analysis of all children for whom hearing rehabilitation with BAHA was indicated at a central hospital, between January 2003 and December 2014.
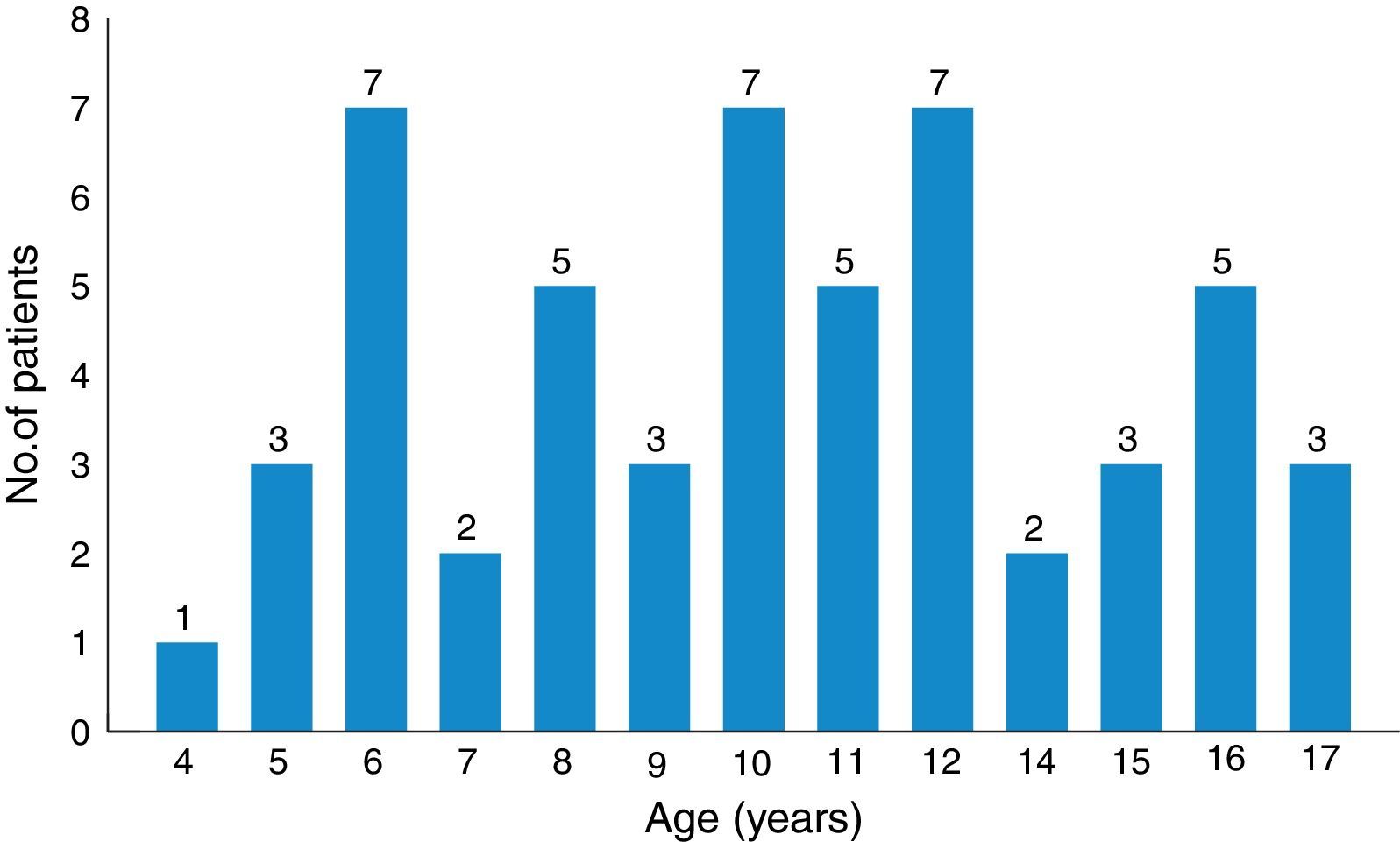
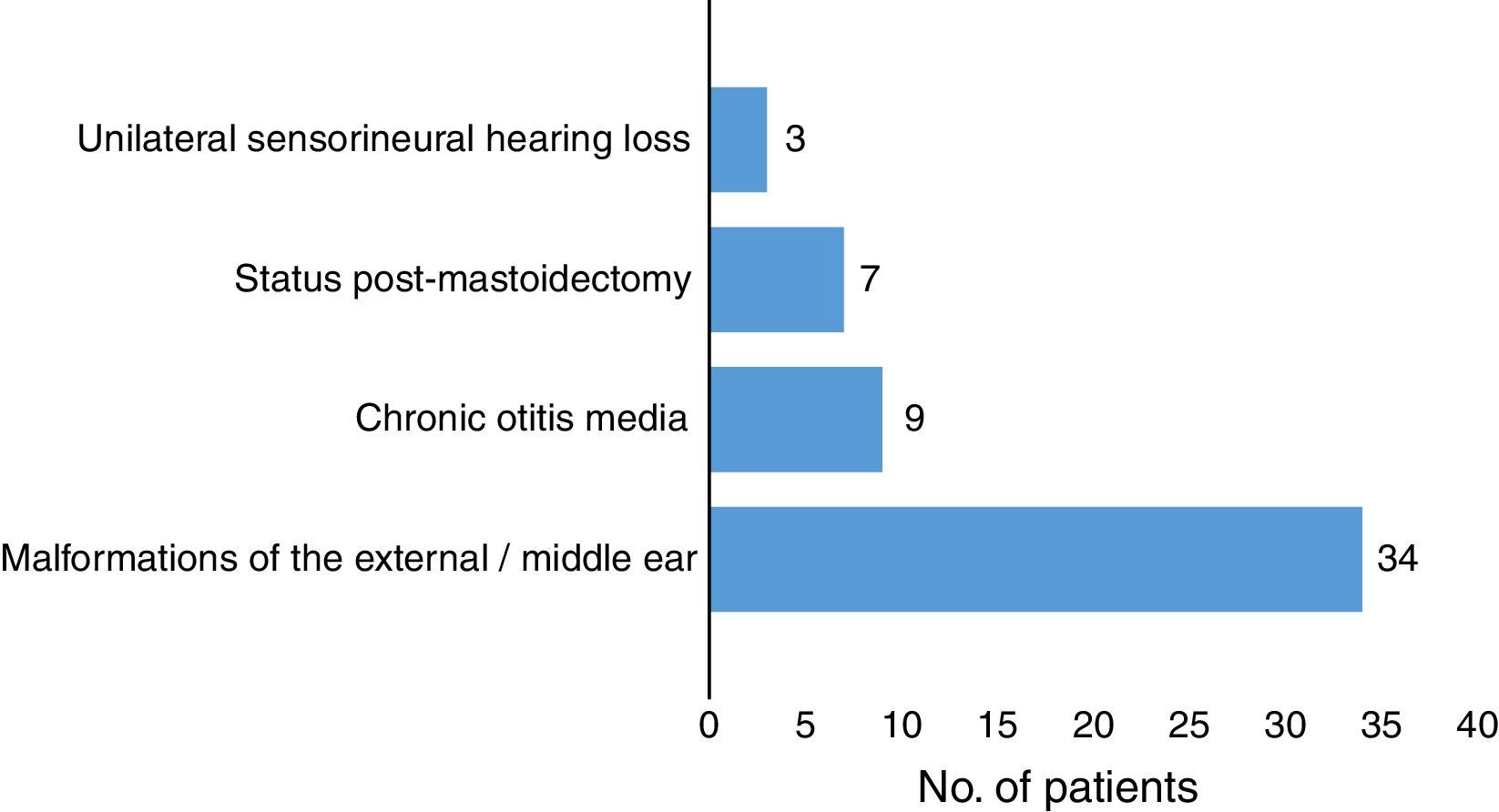
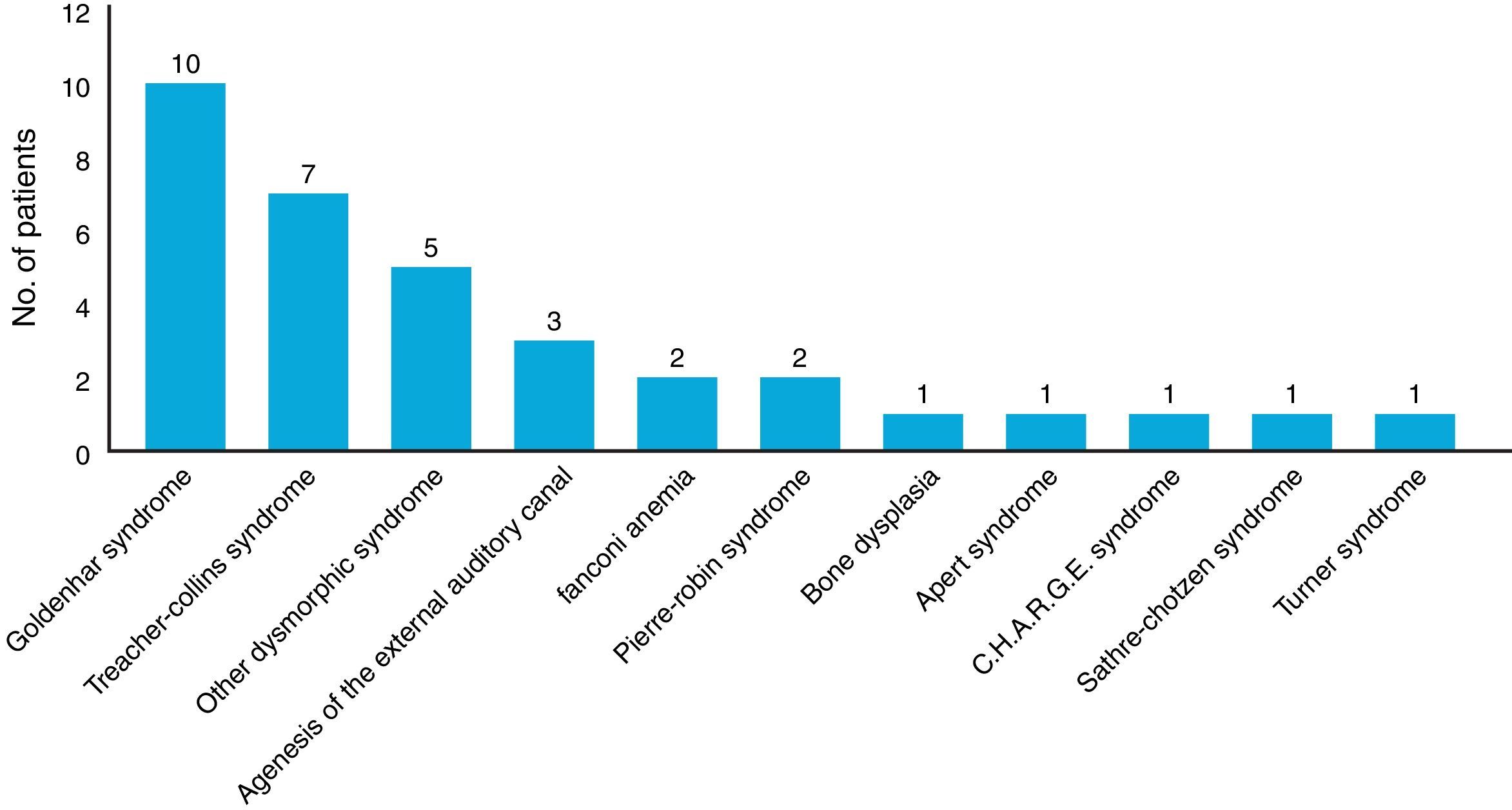
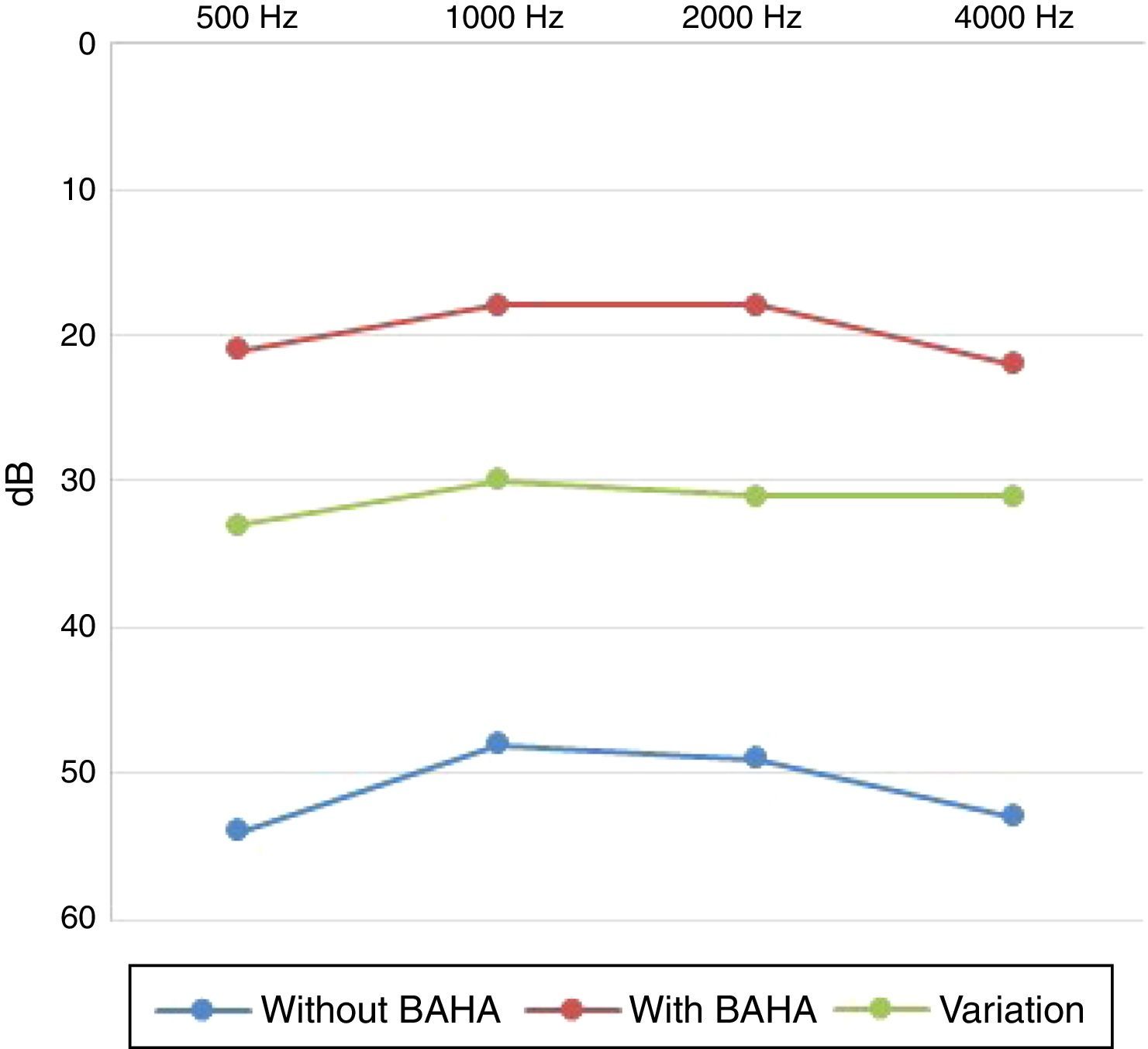
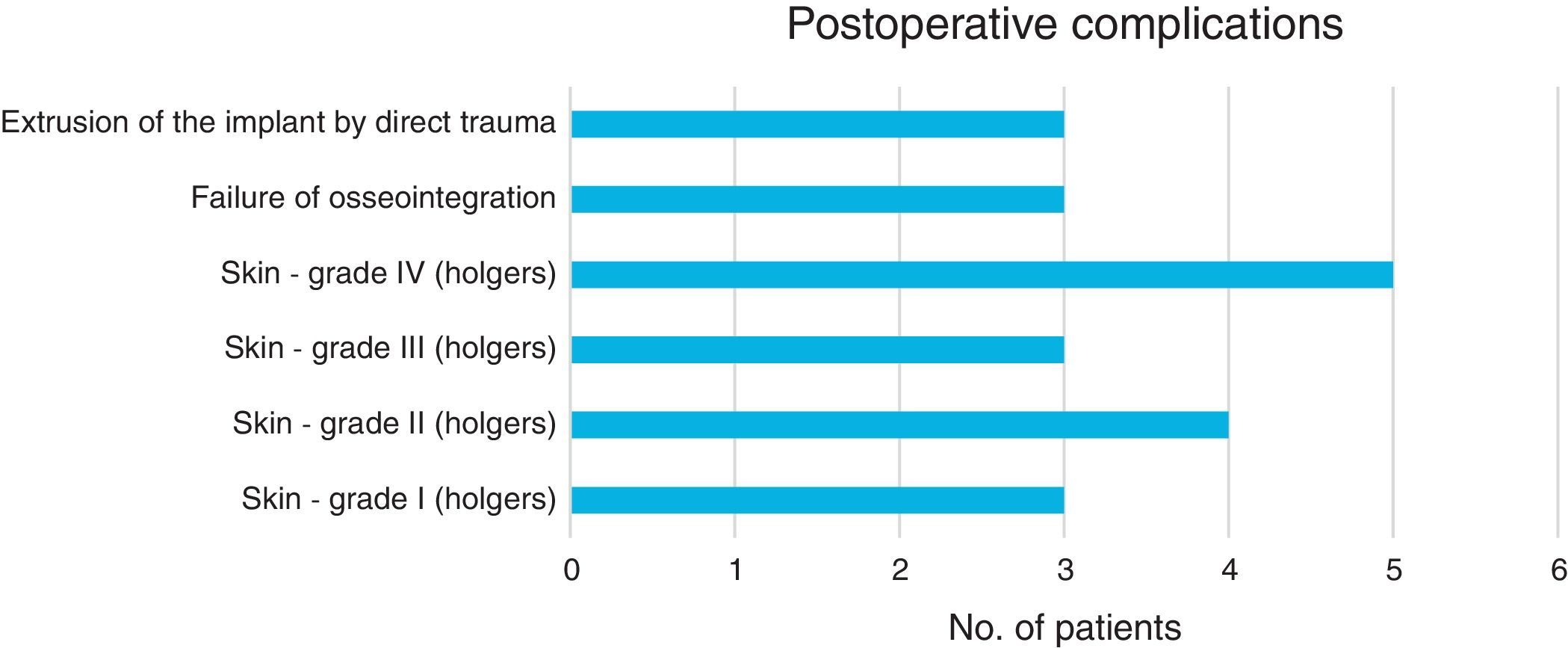
Results53 children were included. The most common indications for placement of BAHA were external and middle ear malformations (n=34, 64%) and chronic otitis media with difficult to control otorrhea (n=9, 17%). The average age for BAHA placement was 10.66±3.44 years. The average audiometric gain was 31.5±7.20dB compared to baseline values, with average hearing threshold with BAHA of 19.6±5.79dB. The most frequent postoperative complications were related to the skin (n=15, 28%). There were no major complications.
ConclusionsThis study concludes that BAHA is an effective and safe method of hearing rehabilitation in children.
El objetivo de este estudio es describir la experiencia de un centro terciario de referencia en Portugal, en la colocación de prótesis auditivas osteointegradas (BAHA) en los niños.
MétodosLos autores realizaron un análisis retrospectivo de todos los niños con indicación para rehabilitación auditiva con BAHA en un hospital central, entre enero de 2003 y diciembre de 2014.
ResultadosSe incluyeron 53 niños. Las indicaciones más frecuentes para la colocación de BAHA fueron las malformaciones del oído externo y medio (n=34; 64%) y la otitis media crónica con otorrea de difícil control (n=9; 17%). La edad media de la colocación de BAHA fue de 10,66±3,44 años. La ganancia de audiometría promedio fue de 31,5±7,20dB en comparación con los valores basales, con un umbral medio de audición con BAHA de 19,6±5,79dB. Como complicaciones postoperatorias, las más frecuentes se relacionaron con la piel (n=15; 28%). No hubo complicaciones mayores.
ConclusionesEn este estudio se concluye que la BAHA es un método eficaz y seguro de rehabilitación auditiva en niños.