Tracheostomy (TR) remains one of the most performed procedures in the Intensive Care Unit (ICU). The literature normally focusses on technical issues and its timing; however, it is important to identify modifiable factors that increase the risk of mortality.
DesignProspective cohort study between October 2013 and April 2019.
SettingICU in a University Hospital in Spain.
PatientsAdmitted to the ICU who underwent a TR during their ICU stay.
InterventionsNone.
MeasurementsMain comorbidities, baseline frailty status, severity scores, and variables related to mechanical ventilation (MV), TR weaning, decannulation, and mortality.
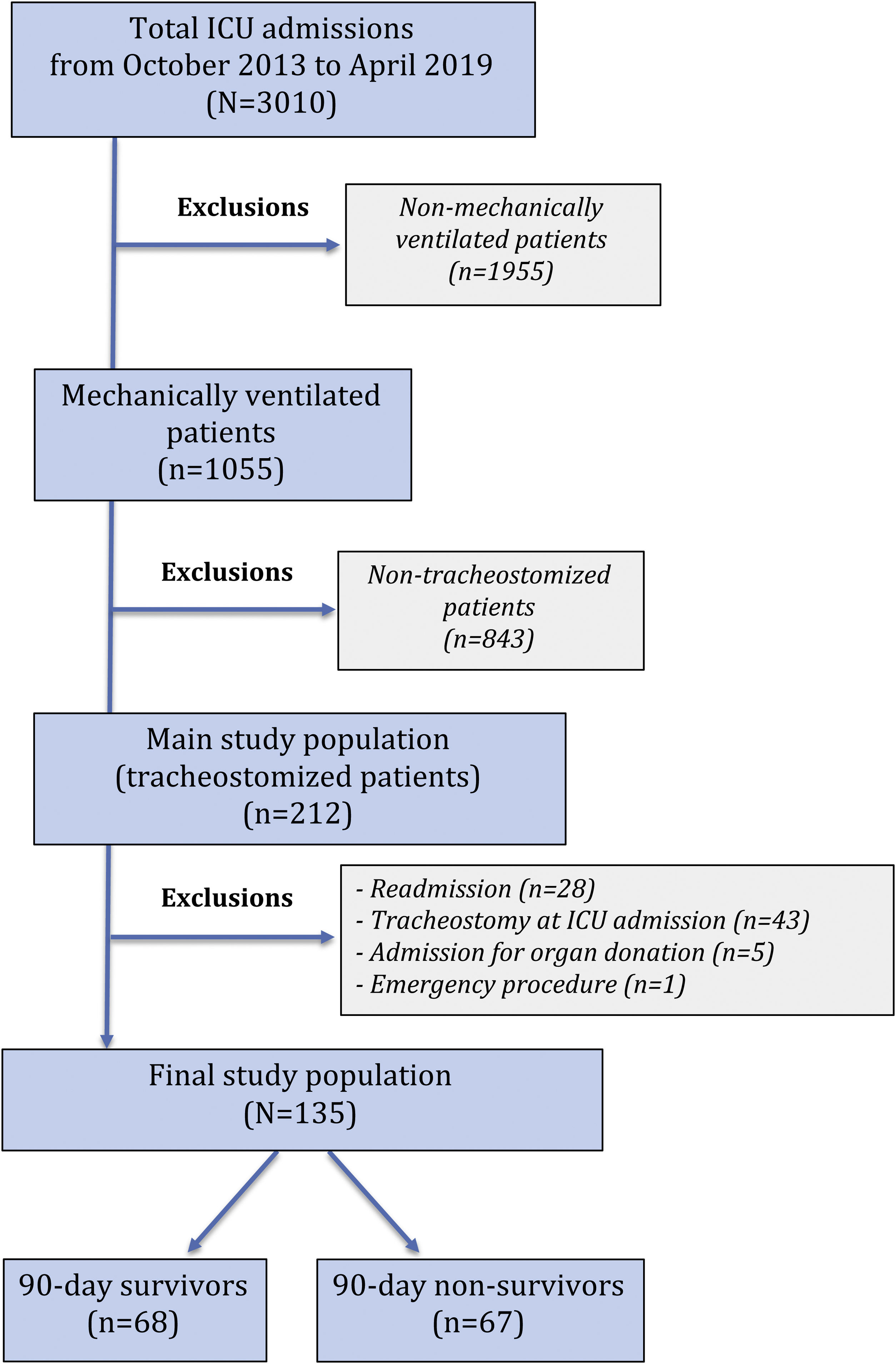
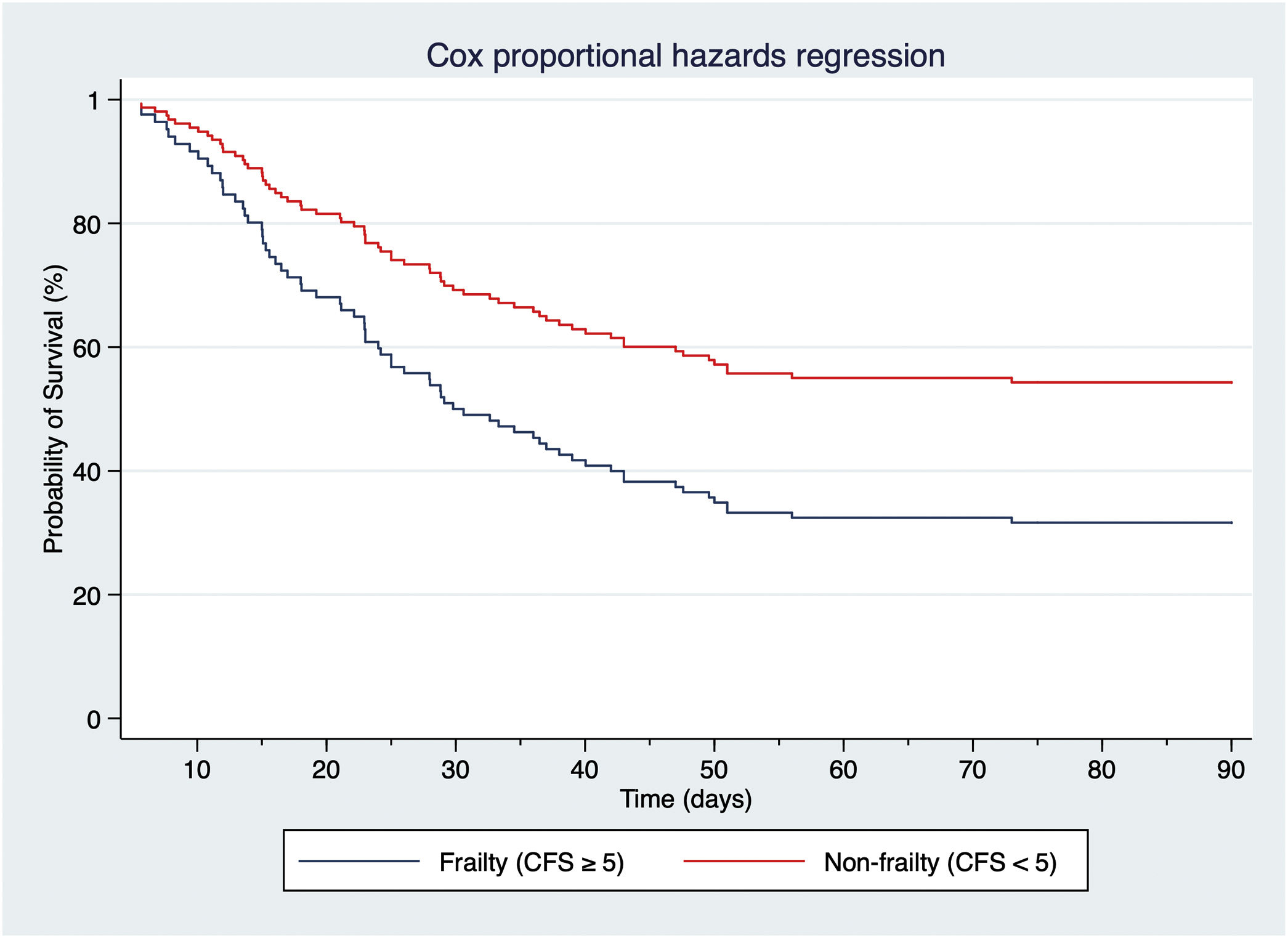
ResultsA total of 3010 admissions were identified; 212 (7%) underwent TR during their ICU stay. The final cohort comprised 135 patients. Median age was 69.6 (61.5–77.4) years; prevalence of frailty was 17.8%. Median time of MV before TR was 8.3 (5.3–11.1) days. All-cause 90-day mortality was 49.6%. Age, severity of illness, the impossibility of attempting a spontaneous breathing (SB) trial, SB time less than 50% of the time with TR, and TR in place at ICU discharge were independent predictors of 90-day mortality. The 90-day mortality rate was 2.2-fold higher in frail (Clinical Frailty Scale, CFS≥5), tracheostomized patients.
ConclusionsFrailty (CFS≥5), the inability of maintaining SB for more than 50% of the time with TR and discharge from ICU with TR in place were independent predictors of 90-day mortality. The creation of a surveillance team focusing on frail and non-decannulated patients to decrease 90-day mortality warrants further investigation.
La traqueotomía (TR) es uno de los procedimientos más empleados en las Unidades de Cuidados Intensivos (UCI). La literatura se centra en aspectos técnicos y en el momento de realización; sin embargo, es importante identificar factores modificables que aumenten el riesgo de mortalidad.
DiseñoEstudio de cohortes prospectivo llevado a cabo entre 2013-2019.
ÁmbitoUCI en un Hospital Universitario en España.
PacientesIngresados en UCI que precisaron TR.
IntervencionesNinguna.
DeterminacionesComorbilidades, fragilidad basal, scores de gravedad, relacionadas con ventilación mecánica (VM), TR, decanulación y mortalidad.
ResultadosDe 3.010 ingresados, 212 (7%) precisaron TR. La cohorte final fue de 135 pacientes. Mediana de edad 69,6 (61,5-77,4) años, mediana de tiempo en ventilación mecánica (VM) antes de TR 8,3 (5,3-11,1) días. Mortalidad global 49,6% a 90 días. Los factores predictores de mortalidad a 90 días fueron la edad, gravedad, imposibilidad de realizar un intento de respiración espontánea (RE), un tiempo en RE inferior al 50% del tiempo con TR y ser dado de alta a planta sin decanular. La mortalidad fue 2,2 veces mayor en los pacientes frágiles (Clinical Frailty Scale ≥ 5).
ConclusionesLos factores predictores de mortalidad a 90 días fueron fragilidad (CFS ≥ 5), imposibilidad de realizar un intento de RE o mantenerlo menos del 50% del tiempo con TR y ser dado de alta a planta con TR. Para disminuir la mortalidad, deberían realizarse nuevos estudios enfocados a evaluar la utilidad de equipos entrenados en el manejo de pacientes frágiles y/o dados de alta de UCI sin decanular.
Artículo
Socios de la Asociación de Medicina Crítica y Cuidado Intensivo
Para acceder a la revista
Es necesario que lo haga desde la zona privada de la web de la AMCI, clique aquí