One of the great challenges during the COVID-19 pandemic was the management of ventilatory support. Extracorporeal membrane oxygenation (ECMO) was the main strategy for the management of refractory acute respiratory distress syndrome.
ObjectiveRetrospective, multicentre cohort study of adult patients who required extracorporeal membrane oxygenation (ECMO) in participating centers. Clinical and paraclinical characteristics were recorded. A comparison was made between surviving and non-surviving patients. In addition, time from symptom onset to ECMO placement, time from mechanical ventilation, and cannulation were analyzed.
Material and methodsRetrospective, multicentre cohort study of adult patients who required extracorporeal membrane oxygenation (ECMO) in participating centers. Clinical and paraclinical characteristics were recorded. A comparison was made between surviving and non-surviving patients. In addition, time from symptom onset to ECMO placement, time from mechanical ventilation, and cannulation were analyzed.
ResultsTwenty-six patients were included in the analysis. Mortality during ECMO was 42.3% (n=11) and overall hospital mortality was 65.3% (n=17). The patient cohort did not differ in terms of sociodemographic characteristics and predictors of mortality at ICU admission between survivors and non-survivors. Mobile ECMO was performed in 10 patients, while 16 were cannulated in situ at the participating centers. The median time from symptom onset to ECMO was 14.5 days (IQR 10.7–21.5), 11 days (IQR 9.5–15.5) in the survivor group, and 17 days (IQR 12.5–27) in non-survivors. The median IMV time was 28.5 (IQR 13–38.25) days. Driving pressure (12 vs 10cmH2O; p<.01), compliance (37.2 vs 21.4ml/cmH2O; p<.01), and mechanical power (17.4 vs 11.3J/min; p=.051) of the respiratory system showed statistically significant differences when comparing survivors and non-survivors, during the 3rd day of ECMO support.
ConclusionIn our cohort, mortality after ECMO and after 30 days of hospital stay, was 42.3%, similar to that stated on the extracorporeal life support organization (ELSO) COVID-19 registry dashboard. Information about patients with COVID-19 who required ECMO during the first wave in Argentina was provided in this analysis.
Uno de los grandes retos durante la pandemia por la COVID-19 fue el manejo del soporte ventilatorio. La oxigenación por membrana extracorpórea (ECMO) fue la principal estrategia para el manejo del síndrome de dificultad respiratoria aguda refractaria.
ObjetivoEl objetivo de este proyecto fue evaluar las características de los pacientes con COVID-19 que requirieron soporte con ECMO.
Materiales y métodosEstudio de cohorte retrospectivo, multicéntrico, de pacientes adultos que requirieron de ECMO en los centros participantes. Se registraron características clínicas y paraclínicas. Se realizó comparación entre los pacientes sobrevivientes y no sobrevivientes. Además, se analizó el tiempo transcurrido desde el inicio de los síntomas hasta la colocación de ECMO, el tiempo desde la ventilación mecánica y la canulación.
ResultadosSe incluyeron 26 pacientes en el análisis. La mortalidad durante ECMO fue de 42,3% (n = 11) y la hospitalaria global fue de 65,3% (n = 17). La cohorte de pacientes no fue diferente, en términos de características sociodemográficas y predicadores de mortalidad al ingreso a Unidad de Cuidados Intensivos (UCI) entre los sobrevivientes y no sobrevivientes. Se realizó ECMO móvil en 10 pacientes, mientras que 16 fueron canulados in situ en los centros participantes. La mediana de tiempo desde el inicio de los síntomas hasta ECMO fue de 14, 5 días (RIC 10,7-21,5), 11 días (RIC 9,5-15,5) en el grupo de supervivientes y 17 días (RIC 12,5-27) en los no supervivientes. La mediana de tiempo de VMI fue de 28,5 (RIC 13-38,25) días. La presión de conducción (12 vs. 10 cmH2O; p < 0,01), el cumplimiento (37,2 vs. 21,4 mL/cmH20; p < 0,01), y el poder mecánico (17,4 vs. 11,3 J/min; p = 0,051) del sistema respiratorio mostraron diferencias estadísticamente significativas al comparar sobrevivientes y no sobrevivientes, durante el tercer día de soporte con ECMO.
ConclusionesEn nuestra cohorte, la mortalidad tras ECMO y a los 30 días de estancia hospitalaria fue de 42,3%, similar a la data recogida por la Extracorporeal Life Support Organization (ELSO) COVID-19.
En este estudio se proporcionó información sobre pacientes que requirieron ECMO durante la primera ola de COVID-19 en Argentina.
During the 2009 H1N1 influenza pandemic, CESAR study contributed to base usefulness and feasibility of extracorporeal circulation membrane support (ECMO) used as an oxygenation strategy in critical patients.1 Following this, EOLIA trial2,3 and ulterior Bayesian analysis of its data, provided information on the benefits of utilization of early ECMO among patients with severe acute respiratory distress syndrome (ARDS).2,3 Consequently, since the beginning of the current COVID-19 pandemic, ECMO has been proposed as a strategy in the treatment of patients with refractory ARDS.4 Approximately, 17% of COVID-19 patients need invasive mechanical ventilation and 1% need ECMO.5 In South America, a recently published Chilean report informed that the 90-day mortality of ECMO-supported patients with COVID-19 (38.8%).6 In Argentina, data providing information about ECMO related mortality is not available.
Despite the greater availability of this technology and the incipient ECMO projects in the region,7,8 a global picture of the results of ECMO support in COVID-19 is still in production6,9 and a coordinated national ECMO Program in Argentina is lacking even now.
The present study evaluates characteristics and outcomes of ECMO utilization in critically ill patients with COVID-19. Diverse Argentinian adult ECMO Centers are included as a first step to further achieve the setting up of a Nationwide Coordinated ECMO Program.
Material and methodsThe present Argentinian retrospective multicentre study analyze epidemiological characteristics, ventilatory mechanics, ECMO settings and outcomes in adult COVID-19 patients with ECMO support during the first surge.
Patients with COVID-19, aged 18 years or older, with ECMO support initiated between March 18th and December 31st of 2020, and treated at participating centers were included in this analysis. Diagnosis for SARS-CoV-2 was confirmed by reverse transcription-polymerase chain reaction (RT-PCR), collected through nasopharyngeal and/or oropharyngeal swabs. Follow-up data was updated until February 1st of 2021. Criteria to ECMO initiation was defined by each treating center following extracorporeal life support organization (ELSO) recommendations.10
Data was collected anonymously for each patient, including demographics, comorbidities, PaO2/FiO2 ratio (ratio of arterial oxygen partial pressure to fractional inspired oxygen), inflammatory biomarkers, prone positioning, neuromuscular blockers use, blood lactate and severity scores (Sequential Organ Failure Assessment [SOFA] score), as well as pre-ECMO intubation days. Ventilatory settings and respiratory mechanics immediately pre-ECMO, at ECMO day 3, and after ECMO weaning were also collected. Mechanical Power was calculated according to what was already published by Chiumiello et al.11 The primary outcome was Hospital mortality after ECMO initiation. Secondary outcomes included ECMO survival and frequency of ECMO-associated complications.
The present study was approved by the Institutional Ethics Committees of each participating center, in particular by the Ethics committee of the Hospital Italiano de Buenos Aires under protocol number 5563 and adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (Supplementary material – Table E1). Informed consent was waived due to retrospective design of the study, and confidentiality regarding patients identity was assured.
Categorical variables are presented with their counts and n over total cases. Numerical variables that assumed a normal distribution were reported with the mean and standard deviation (SD). Otherwise, median and interquartile range (IQR) were used. To determine the sampling distribution of continuous variables, the Shapiro–Wilk test was used. Two groups were formed according to hospital discharge status (survivors/non-survivors). To compare the categorical variables, the Chi-square test or the Fisher's exact, were used as appropriate. For comparison of continuous variables, the t test for independent samples or the Mann–Whitney U test was used, as appropriate; a p-value<0.05 was considered significant. All findings should be interpreted as exploratory and descriptive. Finally, for data analysis, the IBM SPSS Macintosh software, version 26.0 (IBM Corp., Armonk, NY, USA)
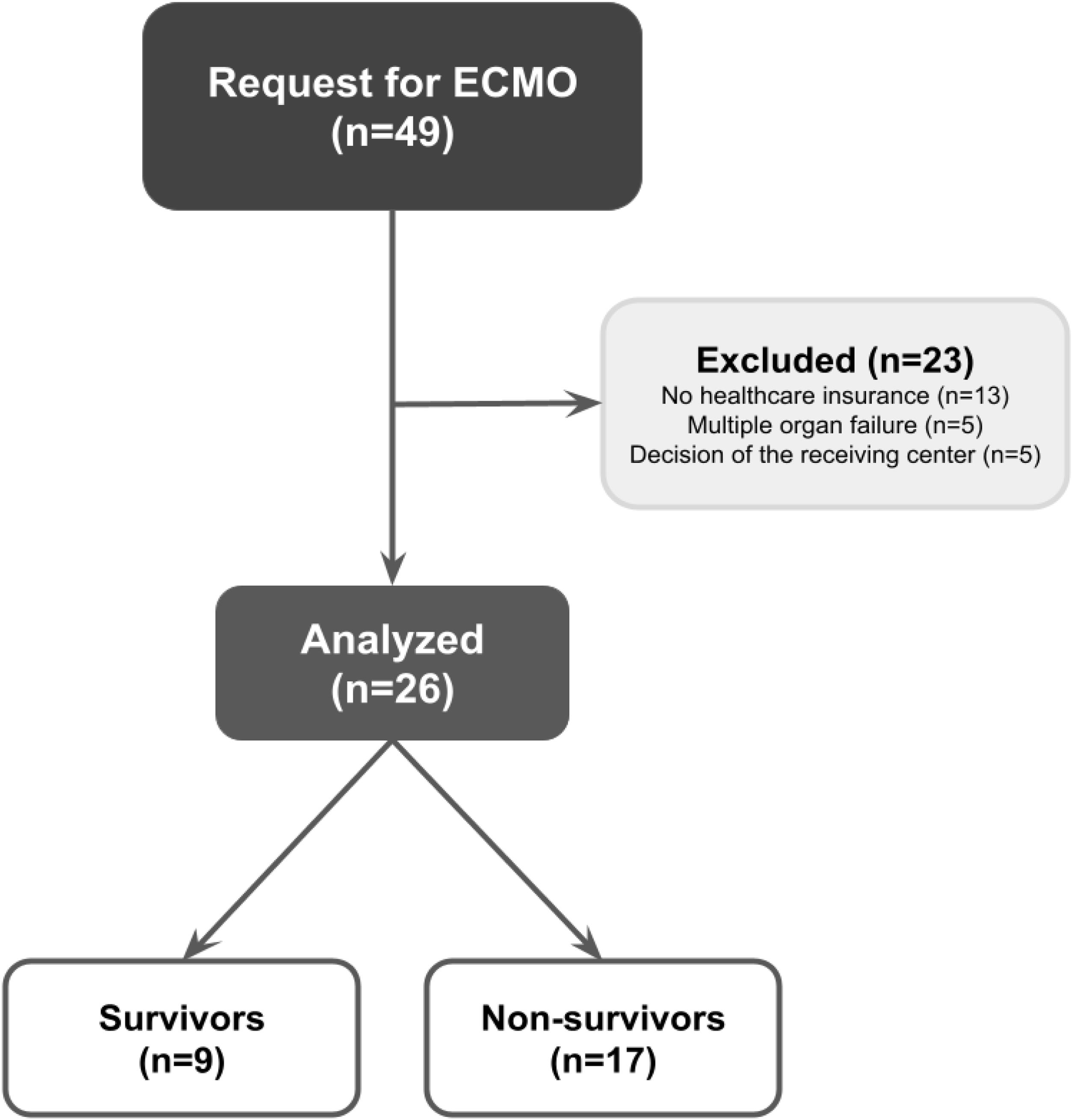
ResultsA total of 49 requests for ECMO were received during the study period but twenty three were excluded for the following reasons: patient had no healthcare insurance (n=13), or multiple organ failure (n=5), or due to decision of the receiving-center medical team because of patient clinical condition or age (n=5). Finally, a total of 26 patients who were treated at the participating centers entered the analysis as was mentioned. Mortality during ECMO support was 42.3% (n=11) while overall hospital mortality was 65.3% (n=17). Fig. 1 illustrates the flow chart of the participants. Patients’ baseline characteristics at ICU admission are shown in Table 1.
Characteristics of the patients at admission to ICU.
| Variables | All(n=26) | Survivors(n=9) | Non survivors(n=17) | Power | p value |
|---|---|---|---|---|---|
| Male, n (%) | 21 (80.8) | 5 (55.6) | 16 (94.1) | 64.8 | 0.034 |
| Age, media (SD), years | 48.3 (13.7) | 45.2 (11.7) | 49.9 (14.8) | 14.2 | 0.42 |
| BMI, median (IQR) | 32.4 (27.9–37) | 35.1 (28.7–38.4) | 30.9 (26.3–37.4) | 20.8 | 0.24 |
| BMI≥30, n (%) | 14 (53.8) | 5 (55.6) | 9 (52.9) | 3.3 | 0.99 |
| Comorbidities, n (%) | |||||
| Arterial hypertension | 8 (30.8) | 3 (33.3) | 5 (29.4) | 4.1 | 0.99 |
| Diabetes | 5 (19.2) | 2 (22.2) | 3 (17.6) | 5.1 | 0.99 |
| Respiratory | 9 (34.6) | 4 (44.4) | 5 (29.4) | 12 | 0.67 |
| Others | 3 (11.5) | 0 (0) | 3 (17.6) | 18.8 | 0.53 |
| Charlson index, median (IQR), score | 1 (0–2) | 1 (0–2) | 1 (0–2) | 5.6 | 0.75 |
| APACHE II, media (SD), score | 9.16 (6.5) | 9.6 (6.5) | 12.9 (6.3) | 23.7 | 0.21 |
| SOFA, media (SD) score | 5.5 (2.9) | 4.8 (3) | 5.8 (2.8) | 12.9 | 0.39 |
| Days of symptoms until admission to ICU, median (IQR) | 7.5 (5–11.2) | 7 (4.5–8) | 10 (5–16.5) | 59.4 | 0.26 |
IQR (interquartile range), SD (standard deviation), BMI (body mass index), APACHE II (Acute Physiology and Chronic Health disease Classification System II), SOFA (Sequential Organ Failure Assessment score).
The results of the laboratory findings at ECMO admission are depicted in Table 2. Only the platelet count and ferritin values were statistically significant when comparing survivors and nonsurvivors (p=0.022 and p=0.04, respectively).
Laboratory variables at admission to ECMO.
| Variables | All(n=26) | Survivors(n=9) | Non survivors(n=17) | Power | p value |
|---|---|---|---|---|---|
| Hemogram | |||||
| Hemoglobin, g/dL* | 11.4 (1.6) | 12.1 (1.1) | 11 (1.7) | 51.3 | 0.10 |
| Leukocytes, mm3 | 13,105 (10,665–17,742) | 15,214 (12,250–18,178) | 12,900 (8421–17,063) | 5.8 | 0.31 |
| Platelets, mm3,* | 278,960 (129,916) | 357,089 (142,659) | 237,598 (104,619) | 60.1 | 0.022 |
| Chemistry | |||||
| Creatinine, mg/dL | 0.81 (0.63–1.27) | 0.79 (0.47–0.93) | 0.9 (0.73–1.65) | 52.7 | 0.05 |
| Total bilirubin, mg/dL | 0.89 (0.64–1.60) | 0.62 (0.48–0.84) | 0.66 (0.51–1.08) | 29.9 | 0.63 |
| Arterial acid base state | |||||
| pH* | 7.33 (0.13) | 7.34 (0.1) | 7.32 (0.14) | 6.2 | 0.79 |
| pCO2, mmHg* | 57.2 (14.4) | 52.2 (9.6) | 59.9 (16.1) | 33.4 | 0.20 |
| pO2, cmH2O | 71.1 (60.9–85.8) | 71.8 (66.7–90.8) | 65 (58.5–84.6) | 12.4 | 0.29 |
| Lactic, mmol/L | 1.9 (1.5–2.5) | 1.8 (1.3–2.3) | 2.0 (1.6–2.5) | 3.1 | 0.29 |
| Biomarkers | |||||
| ProBNP, pg/ml | 150 (95.2–345) | 121 (74–417) | 233.9 (133–2465) | 43.9 | 0.22 |
| Troponin, ng/ml | 19.9 (4.8–33.5) | 4.8 (3.93–33.48) | 25.4 (11.6–34.5) | 15.8 | 0.18 |
| D dimer, ng/ml | 916.5 (8.1–31,452) | 702.5 (2.1–34,963) | 1372 (26–3145) | 2.8 | 0.74 |
| C reactive protein, mg/l* | 114.8 (1127) | 1653 (1393) | 74.4 (69.4) | 45.2 | 0.12 |
| Ferritin, mg/l | 11,807 (626–1726) | 6005 (3998–114,633) | 1604 (772–2384) | 4.0 | 0.04 |
All numerical values are expressed as median and interquartile range. (IRQ). (*) Standard deviation (SD), ECMO (extracorporeal membrane oxygenation), ProBNP (Pro-B-type natriuretic peptide)
Median time from symptoms onset to mechanical ventilation was 8 days (IQR 5–14.2), in the survivors group the median was 8 days (IQR 5–9) and in the non survivors group was 10 days (IQR 5–19). Median time from mechanical ventilation to ECMO was 6 days (IQR 3.75–9.25), showing a median of 5 days (IQR 2.5–8) in the survivors group and a median of 6 days (IQR 3.5–10.5) in the non survivors group. Regarding the time from symptoms onset to ECMO, the median time was 14, 5 days (IQR 10.7–21.5). The median in the survivors group was 11 days (IQR 9.5–15.5) and 17 days (IQR 12.5–27) in the non survivors.
Among the 26 patients included, 10 used high-flow nasal cannula (HFNC) before invasive mechanical ventilation (IMV) and 16 were directly intubated. In the group of HFNC users, 8 of 10 died, and the median number of days from the onset of symptoms to IMV was 10 (IQR 6–20) days. In the subgroup that was directly intubated, 9 of 16 died, and the median number of days from the onset of symptoms to the onset of IMV was 7.5 (IQR 4.2–9.7) days. Previous to ECMO all patients were on neuromuscular blockers, 25 patients were in a prone position and one patient required inhaled nitric oxide. Additionally, all patients were receiving antibiotics and 25 received dexamethasone.
Mobile ECMO was performed on 10 patients, and 16 were cannulated in the participating centers. Eight patients and nine patients died in each group, respectively. Regarding the type of ECMO, 25 received VV ECMO (venous–venous) and one patient received VA ECMO (venous–arterial). 17 patients that received VV ECMO died, and the patient on VA ECMO survived.
The median IMV time was 28.5 (IQR 13–38.25) days. Mechanical ventilation settings recorded before ECMO and at ECMO day 3 are displayed in Table 3. Driving pressure and respiratory system compliance showed statistically significant differences when comparing survivors and non-survivors, before ECMO and at ECMO day 3.
Mechanical ventilation parameters.
| Variables | All(n=26) | Survivors(n=9) | Non survivors(n=17) | Power | p value |
|---|---|---|---|---|---|
| Pre ECMO | |||||
| TV according to theoretical weight, media (SD), ml/kg | 5.9 (0.8) | 6.2 (0.5) | 5.7 (0.9) | 44.5 | 0.19 |
| PaO2/FiO2, median (IQR) | 88 (67–102) | 8975 (77.62–104.8) | 86.57 (62.5–103) | 22.2 | 0.34 |
| PEEP, median (IQR), cmH2O | 10 (7.5–12) | 11 (9–16) | 10 (6–10.5) | 74.4 | 0.04 |
| Driving pressure, media (SD), cmH2O | 15.5 (5.5) | 11.2 (2.1) | 17.7 (5.5) | 99.1 | <0.01 |
| Static compliance, median (IQR), ml/cmH2O | 26.8 (20.6–33.1) | 31.8 (29.2–45) | 22.5 (17–28.7) | 62.9 | <0.01 |
| 3rd ECMO day | |||||
| TV according to theoretical weight, media (SD), ml/kg | 4.8 (1.7) | 5.9 (1.1) | 4.3 (1.7) | 24.1 | 0.021 |
| PEEP, median (IQR), cmH2O | 10 (8–11) | 10 (9–12.5) | 9.5 (8–11.5) | 82.6 | 0.3 |
| Respiratory minute volume, media (SD), L | 4.7 (3) | 6.7 (2.6) | 3.6 (2.7) | 81.4 | 0.01 |
| Driving pressure, median (IQR), cmH2O | 12 (10–15) | 10 (8–12) | 13.5 (12–15.7) | 88.2 | <0.01 |
| Static compliance, median (IQR), ml/cmH2O | 24.2 (19.6–37) | 37.27 (25.5–46.4) | 21.4 (14–25) | 85.9 | <0.01 |
| Mechanical power, media (SD), J/min | 13.5 (7.6) | 17.4 (7.5) | 11.3 (6.9) | 52.7 | 0.051 |
IQR (interquartile range), SD (standard derivation). ECMO (extracorporeal membrane oxygenation), TV (tidal volume), PEEP (positive end-expiratory pressure).
Regarding circuit changes during ECMO application, 9 patients required at least one circuit change, and 17 did not require change, of which 8 and 9 died in each group, respectively. A total of 14 circuit changes were made (n=6 only one, n=2 two, and n=1 four). Median ECMO running time was 11 (IQR 7–20.25).
Median ICU LOS was 30 days (IQR 18–52), 32 days (IQR 17.5–62) among survivors, and 30 days (IQR 18.5–44) among non-survivors. Median hospital LOS was 35 days (IQR 24–56), 49 days (IQR 27.5–72.5) among survivors, and 34 days (18.5–49) among non-survivors.
DiscussionThe present study observes data from ECMO supported patients in Argentina during the first wave of COVID-19 in 2020. As opposed to other countries with ECMO government programs in place,6,9,12,13 in Argentina a communication network was created by the participating centers, and through which assistance of ECMO requests is still currently channeled. Because of the previous stated and due to a long strict quarantine during 2020,14 numbers in Argentina should differ from other reports of the first surge of COVID-19 patients supported with ECMO.15
65% hospital mortality rate for refractory hypoxemia related to severe COVID 19 in Argentina is a slightly higher ratio than the ones observed in larger studies carried out in the US16 and Europe17 during the first wave. Taking into consideration that mortality observed in mechanically ventilated patients with COVID-19 in Argentina was 57.7%,18 the mortality observed in our highly selected cohort of very severe and refractory patients supported with ECMO is in line with national outcomes.
Nevertheless, mortality after ECMO and after 30 days of Hospital stay, was 42.3% in Argentina, similar to the one stated in the ELSO COVID-19 registry dashboard.19 During the second wave in Europe, mortality was higher (66%), longer ECMO times were observed, and weaning with successful ECMO was less frequent,20 similar to the findings in this study. Furthermore, patients in our cohort shared similarities with European second wave such as a high use of dexametasone, non invasive ventilatory support, and longer time on IMV prior to ECMO. All these variables could represent a selection bias toward patient who would not survive on IMV or ECMO. In the present cohort, patients were predominantly male, obese and with a similar inflammatory profile as was previously described.15 PaO2/FiO2 ratio was higher in these patients [(median 88mmHg, IQR 67–102)] than those in ELSO COVID report [median 72 (IQR 59–94)],21 and Lebreton et al. [median 61 (IQR 54–70)],9 but similar to those in the Diaz et al. report [median 86.8 (IQR 63.7–99.2)].6 Sixteen patients were cannulated at ECMO Centers. The previous could explain the difference of a higher PaO2/FiO2 pre-ECMO due to better management of pre-ECMO treatments as occurred in the CESAR study.1
Comparing the patients included in the mobile ECMO group to the ones that were cannulated in a variety of participating Centers, more patients died in the first group stated. Even though a higher rate of death could account for a sicker population, it cannot be ruled out that pre-ECMO ventilatory settings and delays in consulting ECMO Centers could have influenced the outcome. Despite the complexity in the management of patients with COVID-19, fair results have been obtained with mobile ECMO in this population.6,9,22
A significant finding of this study is that patients who died showed a longer time from the onset of COVID-19 related symptoms to the start of ECMO. Similar data was found in the French and Chilean series,9,6 (although in the latter, the time since diagnosis was analyzed). According to the time elapsed from the onset of the disease to the time of ECMO initiation, lung damage could be in a different stage of evolution as has been shown for non-COVID ARDS,23 and the benefits of an ultra protective setting of the mechanical ventilator allowed by extracorporeal oxygenation and subsequent decarboxylation, would not affect outcome. Although the cohort showed a slight trend toward better survival in patients with a duration of symptoms less than 14 days at the time of ECMO initiation, due to the small number of patients included in this study, it is difficult to draw a conclusion and further analysis is needed.
ECMO allowed an ultra protective mechanical ventilation strategy to be implemented in the cohort, as stated by a nearly 50% reduction in the mechanical power and minute volume, and a decrease in plateau and driving pressure. However, important differences between survivors and non survivors were found and should be stated.
From a mechanical point of view, non-survivors were characterized by more severe lung damage before ECMO cannulation. Usually, they had lower respiratory system compliance, higher driving pressure (despite the same tidal volume (TV) and similar Positive end-expiratory pressure (PEEP) levels) and higher plateau pressure. The longer time elapsed from symptoms onset to ECMO in non-survivors could explain at least partially the greater mechanical compromise of the respiratory system, by the time dependency of the histological changes as demonstrated by Thille et al.23 The previous study confirmed that the presence of proliferation and fibrosis is closely related to the duration of evolution of the disorder. In the study by Katzenstein and colleagues24 fibrosis could be noted on the 10th day of evolution. The elevated ferritin levels in non survivors also could suggest a severe proinflammatory profile in this population. At ECMO day 3, survivors showed a higher TV, lower driving and plateau pressure which should be interpreted as increasing compliance and recovery of lung function. Similar findings were reported by Belliato25 and in the Lifeguards26 trial where a higher VT and lower driving pressure (likely markers of static compliance improvement) across the ECMO course were also associated with better outcomes. Besides, a higher respiratory rate, and minute volume on ECMO day 3 on survivors, could be interpreted as transfering gas exchange from the extracorporeal circuit to the native lung in the face of improving lung function after three days of lung rest and ECMO support.
Main limitations of the present study are related to the small number of patients, the retrospective nature of the data, and the different management among ECMO Centers which could have influenced the outcome. Taking in consideration the small sample size not only p value was considered but also power. A lower than desired power indicates that a comparison is less likely to detect a difference when it actually exists. Therefore comparisons must be interpreted with caution, both the positive and the negative ones. For example, APACHE II and SOFA scores were likely different between the two groups, as was troponin, with a significant clinical difference in the two groups under comparison. However, issues related to the small sample size and the statistical power do not allow conclusions to be drawn. New studies with a higher number of participants would be necessary.
Argentina had one of the longest quarantines in the world in 202027 which could have helped to lower the number of hospitalized patients with severe symptoms in need for extracorporeal support, unlike other countries with open policies. The lack of a centralized national ECMO organization as previously described, could contribute to less patients being offered ECMO and a more heterogeneous patient selection, affecting outcome. Additionally it cannot be ruled out that there may be subtle differences in treatment strategies between centers that might have influenced the result. However, the presence of ECMO specialists certified by ELSO in each of the participating centers, guaranteed a level of care in accordance with current recommendations. Increasing COVID-19 cases could increase the demand for more ECMO for refractory respiratory failure. National guidelines were recently issued28 that could help optimize the selection of such a complex group of patients.
Although it is a small cohort, it represents nearly 90% of the patients who received ECMO for covid 19 during the study period in the Argentine. We believe that the main value of this communication resides in the absence of data on respiratory ECMO not related to transplantation in adults in the country. The study does not intend to draw conclusions about the usefulness or not of ECMO in this situation, but rather to reflect a description of a highly selected cohort of very severe and refractory patients with hypoxemic respiratory failure supported with ECMO.
FundingThere were no funds in this study.
Conflict of interestNone.
Mauro Andreu for the statistical analysis.
Sonia Villarroel for the technical management with mobile ECMO.
Nestor Bertoia for his assistance of data entry.
Maria de Los Angeles Magaz for her technical assistance in the translation of the manuscript.