Vaccination against the COVID-19 pandemic, decreed by the WHO in 2020, has shown in the initial trials an admissible efficacy for the scientific community, but with many doubts and concerns for the communities, developing the phenomenon known as vaccine hesitancy.
ObjectiveTo understand the factors associated with the intention or rejection of vaccination against COVID-19 in the city of Popayán in the year 2022.
MethodologyCross-sectional descriptive-analytical study, carried out between August 2021 and March 2022; with a non-probabilistic sampling, for convenience, with a sample size of 993 people; A questionnaire-type survey was applied in person and virtually to know the intention of vaccination, knowledge and perceptions.
ResultsThe surveyed population was characterized as 56.19% female, 49.24% between 18 and 28 years old; 23.16% state that they do not intend to be vaccinated against COVID-19, the main reasons being: not being well informed 56.29%, ineffective vaccine 54.8% and that the vaccine weakens the immune system 27,5%; as well as the low confidence with the Vaccination Plan and with the pharmaceutical companies that produce the vaccine.
ConclusionThe intention to vaccinate against COVID-19 is determined not only by the technical-administrative dynamics of the immunization program and the health system, variables of the context and the perception of risk, add up to explain the vaccination processes.
La vacunación contra la pandemia COVID-19 decretada por la OMS en el 2020, ha demostrado en los ensayos iniciales una eficacia admisible para la comunidad científica, pero con muchas dudas e inquietudes para las comunidades, desarrollando el fenómeno conocido como vacilación vacunal.
ObjetivoComprender los factores asociados a la intención o rechazo de vacunación contra el COVID-19 en la ciudad de Popayán en el año 2022.
MetodologíaEstudio transversal descriptivo-analítico, realizado entre agosto de 2021 y marzo de 2022; con un muestreo no probabilístico, por conveniencia, con un tamaño muestral de 993 personas; se aplicó una encuesta tipo cuestionario de forma presencial y virtual para conocer la intención de vacunación, conocimientos y percepciones.
ResultadosLa población encuestada se caracterizó por ser de género femenino 56,19%, se encuentra entre los 18 y 28 años el 49,24%; manifiestan no tener intención de vacunarse contra el COVID-19 es del 23,16%, siendo las principales razones: no estar bien informados 56,29%, vacuna no efectiva el 54,8% y que la vacuna debilita el sistema inmunológico el 27,5%; así como también se expresa la baja confianza con el Plan de vacunación y de las farmacéuticas que producen la vacuna.
ConclusiónLa intención de vacunación contra la COVID-19, está determinada no solo por las dinámicas técnico-administrativas del programa de inmunización y del sistema de salud, variables del contexto y de la percepción del riesgo, se suman para explicar los procesos de vacunación.
In 2019, severe acute respiratory syndrome 2 (SARS-CoV-2) emerged in Wuhan China, a disease that the WHO1 declared a pandemic in 2020 and in which immunisation has been shown to be an effective strategy to reduce the spread, severity of symptoms and number of deaths.2,3 According to the National Institute of Health (INS) of Colombia,4 by May 2022, more than 6 million confirmed cases were reported, of which approximately 139,000 died.
As a consequence of the severity of the disease, a vaccination programme for the coronavirus was initiated worldwide, which seeks to reduce related deaths, hospitalisations for severe cases, post-covid sequelae and transmission of the disease. In Colombia, a national vaccination programme against COVID-19 was initiated for all inhabitants over 16 years of age, with a gradual strategy framed in two phases of progressive prioritisation.5
The vaccines mentioned have demonstrated WHO-approved efficacy in their initial trials, acceptable to the scientific community, but with many doubts and concerns for communities, who, in some cases, enter into a phenomenon known as vaccine hesitancy, which refers to "delay in acceptance or refusal of vaccination despite the availability of vaccination services". Vaccine hesitancy is complex and context-specific, and varies according to time, place and vaccines.6 This phenomenon may be influenced by a number of variables, including health and immunisation literacy, confidence in vaccine efficacy and safety, reliability and competence of services, among others.6 According to WHO,7 vaccine hesitancy is among the top 10 causes threatening global health security and according to Nossier8 is one of the greatest threats to vaccination programmes against COVID-19.
A study conducted by the National Administrative Department of Statistics (DANE) in 2020, applied to 24 Colombian cities, inquired about vaccination intention for COVID-19 and found that the intention of the population of Popayán was 61.1%,9 however, the reasons for vaccination intention in the city of Popayán were unknown.
The above results suggest that, even with the availability of COVID-19 vaccines, a part of the population is expected not to be vaccinated. Unwillingness to receive the vaccine remains a major challenge to achieving the required vaccination coverage for population immunity, making it necessary to understand the factors associated with intention or refusal to vaccinate against COVID-19 in the city of Popayán in 2022.
MethodologyA descriptive-analytical cross-sectional study was conducted, with non-probabilistic convenience sampling. The sample size was calculated with the Epidat 3.1 programme, with a population of 210,134 inhabitants between 18 and 59 years of age, for the city of Popayán (DANE, 2019), with a significance level of 99%, expected proportion of 50% and estimation error of 5%, resulting in a sample size of 894 people. A loss rate of 10% (99 persons) was assumed in the event of any inconvenience or difficulty in the data entry, resulting in a final sample size of 993 persons.
Fieldwork was conducted from 1 August 2021 to 1 March 2022. Information was collected through the construction of a survey consisting of 3 dimensions: socio-demographic characteristics, intention to vaccinate, and knowledge and perceptions about vaccination. The survey was applied in person at the points of greatest affluence in the city of Popayán (shopping centres, market galleries, sports venues and the city centre) and virtually through a Google form shared in specific groups of social networks in the city. The inclusion criteria to be part of the study were to be a resident of the city of Popayán and to be between 18 and 59 years of age; people who had already been vaccinated against COVID-19 at the time of the study and those who did not complete the survey in full were excluded from the study.
The statistical package Stata 15 was used for data management. A descriptive analysis of the data was carried out according to the type of variable. For quantitative variables, measures of central tendency and measures of dispersion were used, taking into account their distribution. Categorical variables, both nominal and ordinal, were described through absolute and relative frequencies. For bivariate analysis, continuous variables were compared with respect to the dependent variable (intention to vaccinate) using the Student's t-test if the distribution was normal or the Wilcoxon rank sum test if the distribution was non-normal. For categorical variables, the chi-square test or Fisher's exact test was applied, as appropriate.
Subsequently, separate binary logistic regressions were estimated, examining different independent variables (socio-demographic data, knowledge and confidence about vaccination for COVID-19) with the dependent variable (intention to vaccinate). Multiple logistic regression was then applied. Independent variables with p ≤ .25 were included in the initial model and continued with the forward selection option (conditional - likelihood ratio statistic), at a significance level of .05. Finally, the Hosmer-Lameshow test was applied to demonstrate the goodness-of-fit of the model obtained.
In terms of ethical considerations, the study was categorised as minimal risk research. The principles of bioethics were applied as established by the Declaration of Helsinki, resolution no. 8430 of 1993 of the Colombian Ministry of Health, law 1581 of 2012 and its regulatory decree 1377 of 2013. A document was shared with the participants with the description and purpose of the research, the procedure to be used, the use that would be made of the information, the risks and benefits, the voluntary participation and the mechanisms with which the confidentiality of the information was guaranteed. The study was approved by the research ethics committee of a higher education institution.
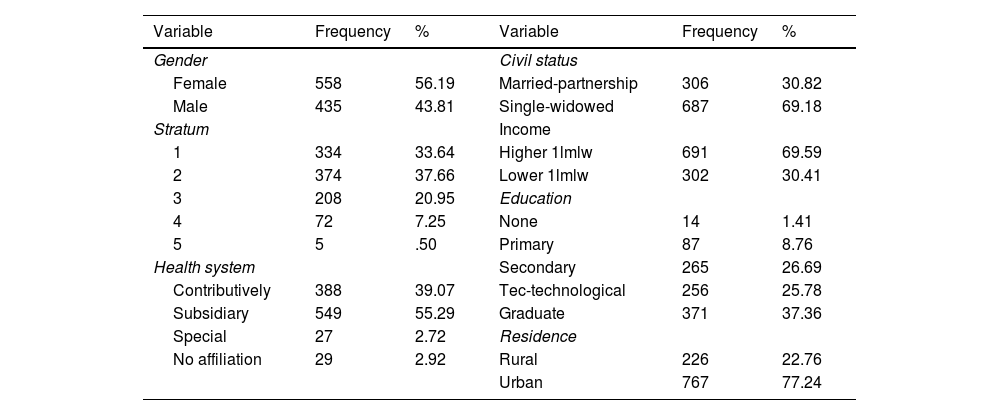
ResultsThe number of individuals who responded to the questionnaire was 1,067, of which 993 individuals met all the inclusion criteria. 49.24% (n = 489) of the study population were between 18 and 28 years old, 27.09% (n = 269) between 29 and 39 years old, 14.10% (n = 140) between 40 and 50 years old and 9.57% (n = 95) between 51 and 59 years old (socio-demographic characteristics are described in Table 1).
Socio-demographic characteristics.
| Variable | Frequency | % | Variable | Frequency | % |
|---|---|---|---|---|---|
| Gender | Civil status | ||||
| Female | 558 | 56.19 | Married-partnership | 306 | 30.82 |
| Male | 435 | 43.81 | Single-widowed | 687 | 69.18 |
| Stratum | Income | ||||
| 1 | 334 | 33.64 | Higher 1lmlw | 691 | 69.59 |
| 2 | 374 | 37.66 | Lower 1lmlw | 302 | 30.41 |
| 3 | 208 | 20.95 | Education | ||
| 4 | 72 | 7.25 | None | 14 | 1.41 |
| 5 | 5 | .50 | Primary | 87 | 8.76 |
| Health system | Secondary | 265 | 26.69 | ||
| Contributively | 388 | 39.07 | Tec-technological | 256 | 25.78 |
| Subsidiary | 549 | 55.29 | Graduate | 371 | 37.36 |
| Special | 27 | 2.72 | Residence | ||
| No affiliation | 29 | 2.92 | Rural | 226 | 22.76 |
| Urban | 767 | 77.24 |
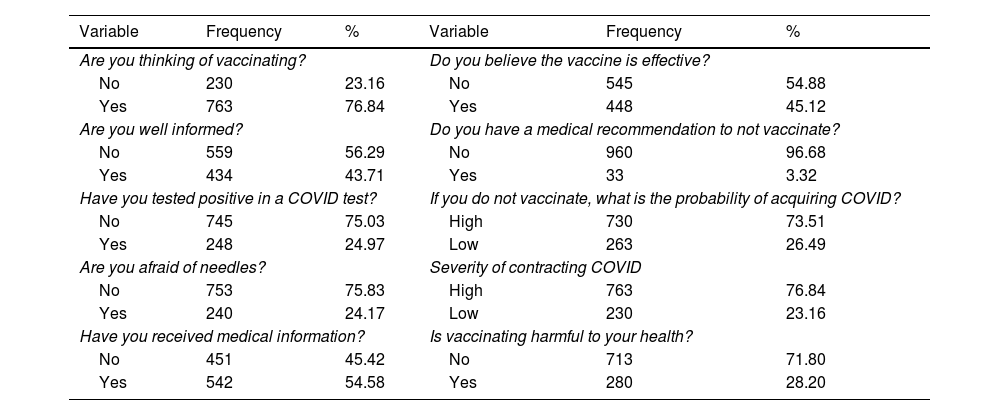
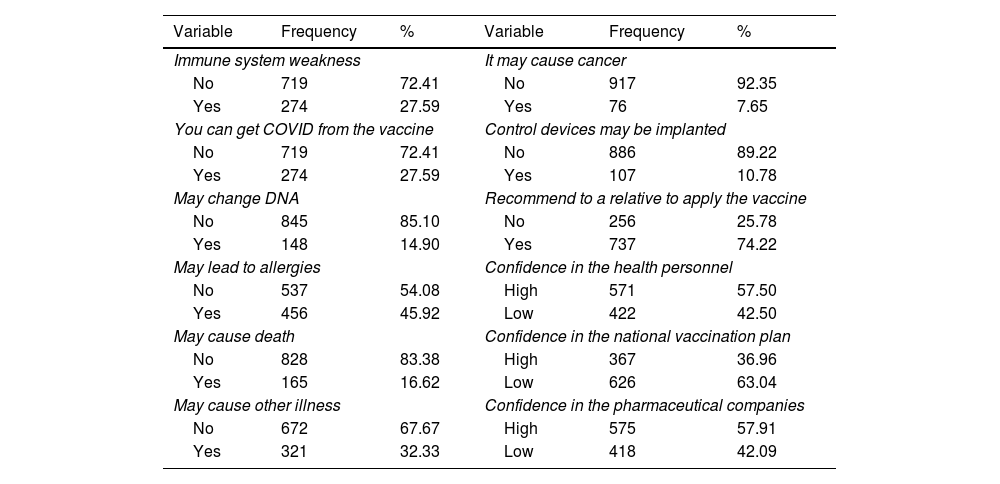
In Popayán, the study population that does not intend to be vaccinated against COVID-19 is 23.16% (n = 230). A total of 24.97% (n = 248) have tested positive for COVID-19. When asked about the reasons for their intention not to vaccinate, they reported not being well informed about vaccination (56.29%), being afraid of needles (24.17%), not having received adequate medical information (45.42%), not considering the vaccine effective (54.88%), considering the probability of contracting COVID-19 without vaccinating to be low (26.49%) or considering the COVID-19 vaccine as harmful to their health (28.20%) (see Tables 2 and 3).
Intention to vaccinate.
| Variable | Frequency | % | Variable | Frequency | % |
|---|---|---|---|---|---|
| Are you thinking of vaccinating? | Do you believe the vaccine is effective? | ||||
| No | 230 | 23.16 | No | 545 | 54.88 |
| Yes | 763 | 76.84 | Yes | 448 | 45.12 |
| Are you well informed? | Do you have a medical recommendation to not vaccinate? | ||||
| No | 559 | 56.29 | No | 960 | 96.68 |
| Yes | 434 | 43.71 | Yes | 33 | 3.32 |
| Have you tested positive in a COVID test? | If you do not vaccinate, what is the probability of acquiring COVID? | ||||
| No | 745 | 75.03 | High | 730 | 73.51 |
| Yes | 248 | 24.97 | Low | 263 | 26.49 |
| Are you afraid of needles? | Severity of contracting COVID | ||||
| No | 753 | 75.83 | High | 763 | 76.84 |
| Yes | 240 | 24.17 | Low | 230 | 23.16 |
| Have you received medical information? | Is vaccinating harmful to your health? | ||||
| No | 451 | 45.42 | No | 713 | 71.80 |
| Yes | 542 | 54.58 | Yes | 280 | 28.20 |
Awareness and perceptions about vaccination.
| Variable | Frequency | % | Variable | Frequency | % |
|---|---|---|---|---|---|
| Immune system weakness | It may cause cancer | ||||
| No | 719 | 72.41 | No | 917 | 92.35 |
| Yes | 274 | 27.59 | Yes | 76 | 7.65 |
| You can get COVID from the vaccine | Control devices may be implanted | ||||
| No | 719 | 72.41 | No | 886 | 89.22 |
| Yes | 274 | 27.59 | Yes | 107 | 10.78 |
| May change DNA | Recommend to a relative to apply the vaccine | ||||
| No | 845 | 85.10 | No | 256 | 25.78 |
| Yes | 148 | 14.90 | Yes | 737 | 74.22 |
| May lead to allergies | Confidence in the health personnel | ||||
| No | 537 | 54.08 | High | 571 | 57.50 |
| Yes | 456 | 45.92 | Low | 422 | 42.50 |
| May cause death | Confidence in the national vaccination plan | ||||
| No | 828 | 83.38 | High | 367 | 36.96 |
| Yes | 165 | 16.62 | Low | 626 | 63.04 |
| May cause other illness | Confidence in the pharmaceutical companies | ||||
| No | 672 | 67.67 | High | 575 | 57.91 |
| Yes | 321 | 32.33 | Low | 418 | 42.09 |
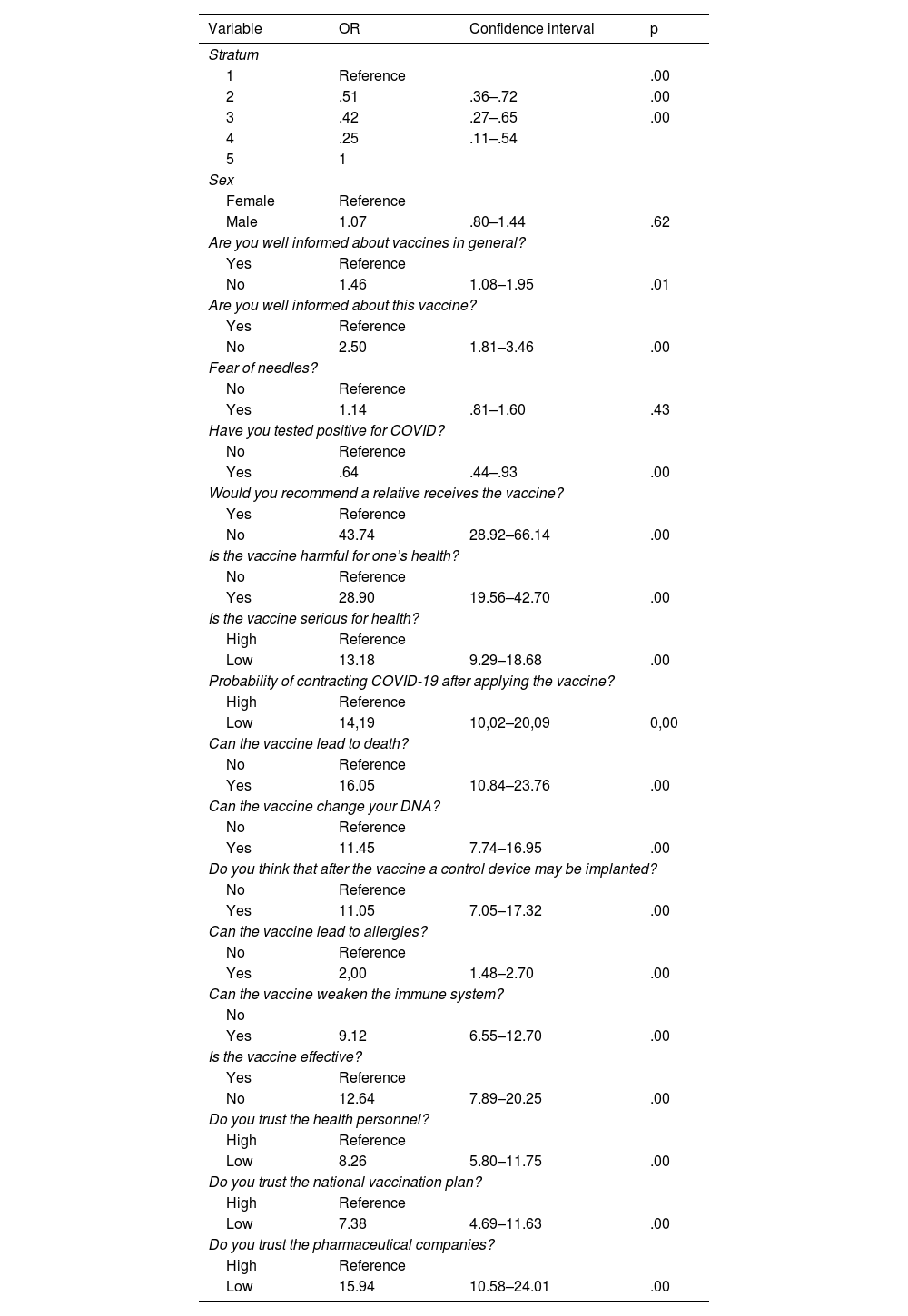
The results of simple logistic regressions showed that considering the COVID-19 vaccine as harmful to health, considering the vaccine as a weakening of the immune system, considering it as an immunobiological capable of causing death and considering COVID-19 as a disease of low severity to health are risk factors for not intending to be vaccinated against COVID-19. Similarly, low trust in health personnel, in the national vaccination plan and in pharmaceutical companies were associated with non-vaccination intention.
In addition, the odds of recommending to the family not to receive the COVID-19 vaccine in people who do not intend to vaccinate are 43.7 times that of people who do intend to vaccinate (OR: 43.74 CI: 28.92–66.14 P < .05).
Furthermore, the intention not to vaccinate against COVID-19 decreases with increasing stratum (intention not to vaccinate versus stratum 1 is 49% lower in stratum 2 (OR: 0.51 CI: 0.36–0.72 P < 0.05), 58% lower in stratum 3 (OR: 0.42 CI: 0.27–065 P < 0.05) and 75% lower in stratum 4 (OR: 0.25 CI: 0.11–0.54 P < 0.05). Similarly, in people who have tested positive for PCR, the chance of not intending to be vaccinated is reduced by 36% (OR: 0.06 CI: 0.44–0.93 P < .05), in contrast to people who have not tested positive for COVID-19 (Table 4).
Bivariate logistic regression.
| Variable | OR | Confidence interval | p |
|---|---|---|---|
| Stratum | |||
| 1 | Reference | .00 | |
| 2 | .51 | .36–.72 | .00 |
| 3 | .42 | .27–.65 | .00 |
| 4 | .25 | .11–.54 | |
| 5 | 1 | ||
| Sex | |||
| Female | Reference | ||
| Male | 1.07 | .80–1.44 | .62 |
| Are you well informed about vaccines in general? | |||
| Yes | Reference | ||
| No | 1.46 | 1.08–1.95 | .01 |
| Are you well informed about this vaccine? | |||
| Yes | Reference | ||
| No | 2.50 | 1.81–3.46 | .00 |
| Fear of needles? | |||
| No | Reference | ||
| Yes | 1.14 | .81–1.60 | .43 |
| Have you tested positive for COVID? | |||
| No | Reference | ||
| Yes | .64 | .44–.93 | .00 |
| Would you recommend a relative receives the vaccine? | |||
| Yes | Reference | ||
| No | 43.74 | 28.92–66.14 | .00 |
| Is the vaccine harmful for one’s health? | |||
| No | Reference | ||
| Yes | 28.90 | 19.56–42.70 | .00 |
| Is the vaccine serious for health? | |||
| High | Reference | ||
| Low | 13.18 | 9.29–18.68 | .00 |
| Probability of contracting COVID-19 after applying the vaccine? | |||
| High | Reference | ||
| Low | 14,19 | 10,02–20,09 | 0,00 |
| Can the vaccine lead to death? | |||
| No | Reference | ||
| Yes | 16.05 | 10.84–23.76 | .00 |
| Can the vaccine change your DNA? | |||
| No | Reference | ||
| Yes | 11.45 | 7.74–16.95 | .00 |
| Do you think that after the vaccine a control device may be implanted? | |||
| No | Reference | ||
| Yes | 11.05 | 7.05–17.32 | .00 |
| Can the vaccine lead to allergies? | |||
| No | Reference | ||
| Yes | 2,00 | 1.48–2.70 | .00 |
| Can the vaccine weaken the immune system? | |||
| No | |||
| Yes | 9.12 | 6.55–12.70 | .00 |
| Is the vaccine effective? | |||
| Yes | Reference | ||
| No | 12.64 | 7.89–20.25 | .00 |
| Do you trust the health personnel? | |||
| High | Reference | ||
| Low | 8.26 | 5.80–11.75 | .00 |
| Do you trust the national vaccination plan? | |||
| High | Reference | ||
| Low | 7.38 | 4.69–11.63 | .00 |
| Do you trust the pharmaceutical companies? | |||
| High | Reference | ||
| Low | 15.94 | 10.58–24.01 | .00 |
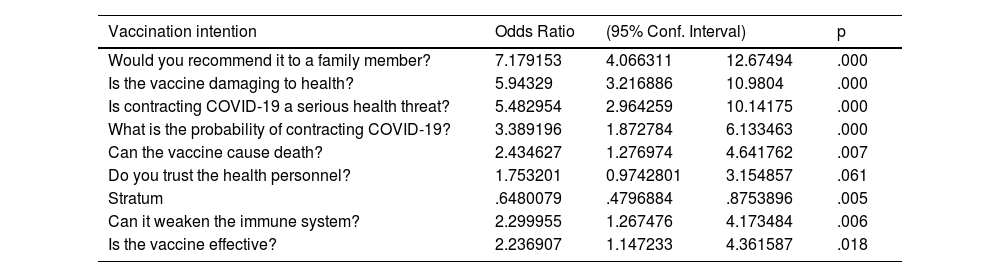
The results of the multivariate logistic regression showed that after controlling for sociodemographic variables, beliefs about the severity of the disease, the consequences of vaccination such as contracting the disease, death and weakening the immune system are risk factors for not intending to vaccinate. Similarly, not considering the vaccine effective, having low trust in health workers and considering the likelihood of contracting COVID-19 to be low were described as additional risk factors (table 5).
Multivariate logistic regression.
| Vaccination intention | Odds Ratio | (95% Conf. Interval) | p | |
|---|---|---|---|---|
| Would you recommend it to a family member? | 7.179153 | 4.066311 | 12.67494 | .000 |
| Is the vaccine damaging to health? | 5.94329 | 3.216886 | 10.9804 | .000 |
| Is contracting COVID-19 a serious health threat? | 5.482954 | 2.964259 | 10.14175 | .000 |
| What is the probability of contracting COVID-19? | 3.389196 | 1.872784 | 6.133463 | .000 |
| Can the vaccine cause death? | 2.434627 | 1.276974 | 4.641762 | .007 |
| Do you trust the health personnel? | 1.753201 | 0.9742801 | 3.154857 | .061 |
| Stratum | .6480079 | .4796884 | .8753896 | .005 |
| Can it weaken the immune system? | 2.299955 | 1.267476 | 4.173484 | .006 |
| Is the vaccine effective? | 2.236907 | 1.147233 | 4.361587 | .018 |
1. Chi-square Hosmer and Lemeshow = 5.32, p = .722.
According to the present study, there is a high prevalence of people who do not intend to be vaccinated (23.1%), this situation was similar to the study by Ruiz,10 where it is evident that 14.8% of respondents have a limited intention to be vaccinated and 23% say they feel insecure; in the same way, Viswanath et al.11 found that 50.3% of respondents stated that they were unlikely to be vaccinated, showing resistance to the vaccination process that is being implemented worldwide.
According to the records obtained, the female gender had greater participation in the surveys carried out in the city of Popayán, as well as in the studies carried out in France,12 the United Kingdom13 and the United States,10 where more than 50% of women showed greater participation in issues related to vaccination against COVID-19, finding that men were less likely to participate, as they are less motivated by the vaccine.12 Likewise, Detoc et al.12 found in their research that those who are most interested in participating in this type of study have a technical-technological or university level of education, which is similar to what was found in the present study.
Similarly, the results from Popayán showed that socioeconomic factors, level of education and high income are associated with a greater intention to be vaccinated, similar to the study by Nikolovskiid et al.14 in the United States, where it was found that poor populations and those with a low level of education were less willing to be vaccinated.
According to DANE figures, Popayán has 328,129 inhabitants. According to official records, by May 2022, 93 per cent of the population received the first dose and 81.4 per cent received the second dose, leaving approximately 61,193 people in the city who have not yet been fully vaccinated.15 Despite the great insistence by the National Government to promote vaccination and the great media coverage of COVID-19, there is still a significant number of inhabitants who have not been vaccinated.
Furthermore, the Ministry of Health and Social Protection, by means of resolution no. 350 of 2022,16 established new guidelines regarding the use of face masks, making the use of this personal protection element in open spaces not required in regions where at least 70% of the population had a complete vaccination schedule, meaning the first and second doses, without boosters. According to INS figures,4 Popayán met the percentage for the implementation of the measure, however, the department of Cauca did not reach the required threshold. By May 2022, only 41.7% of the total population of the department has the complete scheme; a situation that generates uncertainty about the emergence of a new epidemiological peak due to the constant displacement of inhabitants from rural areas to the departmental capital, increasing the risk of exposure of the unvaccinated and those who do not intend to be vaccinated and, consequently, the increase in morbidity and mortality due to COVID-19.
According to the study by Ruiz and Bel,10 there are at least 4 reasons for vaccine hesitancy: concerns about the side effects of the vaccine, concerns about allergic responses to the vaccine, doubts about the efficacy of the vaccine, and concerns about developing immunity through infection. In the present study, 54% of the population do not consider the vaccine to be effective and a high percentage have concerns about side effects, including DNA alteration, generation of other diseases and even death. Similarly, it should be noted that one of the reasons that least supports non-vaccination is fear of needles, with a representation of only 11% in the study by Ruiz and Bell10 and 24.1% in the present study.
Regarding knowledge and perceptions about vaccination against COVID-19, 27.59% of the study population believe that they can contract the disease through vaccination, a figure that coincides with the study by Sherman et al.,13 where the population believes that a vaccine against the coronavirus could transmit the virus. Only 32.33% of the study population believe that the vaccine may cause other diseases, which is lower, compared to the perception found in the aforementioned study, where the concern about experiencing side effects from a coronavirus vaccine is higher.
Regarding the perception of the surveyed population of the seriousness of contracting COVID-19, in this research it was quite high at 76.84%, which is in line with the data from the article by Sherman et al.,13 where 73.4% believe that the coronavirus represents a significant to important risk to people in the UK.
The intention not to be vaccinated against COVID-19 decreases with increasing stratum; living in rural areas where the socio-economic strata are low increases the fear of adverse effects that could be caused by the vaccine.17 As these areas are vulnerable and difficult to access due to their geographic barriers, their population does not have useful coverage that provides adequate and timely information on promotion and preven tion services, within which immunisation strategies against the virus are outline.
On the other hand, the present study shows an association between people who do not intend to be vaccinated and those who do not recommend vaccination to their friends and family members. According to the study by Urrunaga-Pastor et al.,17 the recommendation of friends and family has a positive influence on the intention to vaccinate, but is associated with a higher prevalence of adverse effects. This situation suggests that excessive exposure to false and fatalistic news may generate resistance to vaccination and lead to vaccination refusal.
The results of the present study indicate that 63.04% of the surveyed population has low confidence in the implementation of the national vaccination plan, contrary to what was found in the study by Sherman et al.,13 where the population indicated confidence in the National Health Service to manage the coronavirus pandemic in the UK. According to Urrunaga-Pastor et al.,17 the low trust in government entities could be due to the fact that the measures adopted have been affected by political decisions or groups, which has led to clandestine vaccination outside the context of a clinical trial and influence peddling.
ConclusionThe intention to vaccinate against COVID-19 is determined not only by the technical-administrative dynamics of the immunisation programme and the health system, but also by the variables of the context and the perception of risk, which add up to explain the vaccination processes.
It should be noted that this research has the limitations inherent to cross-sectional studies, including the impossibility of establishing causal relationships, among other aspects, such as the lack of approximation of the population's perception of the appearance of new strains of the virus, since it is a phenomenon that generates changes in its infectious capacity, clinical evolution and prognosis, which becomes a factor that reduces the effectiveness of current vaccines and can consequently reduce the population's confidence both in the application of the first dose and in completing vaccination schedules.
It is suggested that health authorities refer to variables such as those expressed in this study, in order to strengthen decisions in the planning, implementation and evaluation of health policy related to immunisation against COVID-19.
FundingThis research was funded by the University of Cauca.
AuthorshipAuthors Omar Andrés Ramos Valencia, Yuliana Buitrón González and Jorge Sotelo Daza participated in the conceptualisation, research, methodological design, data curation, data analysis and writing of the manuscript. Authors Omar Andrés Ramos Valencia, Yuliana Buitrón González and Andrés Felipe Villaquiran participated in the revision and editing of the final manuscript.
Our thanks to the people who participated and made possible the development of this study.
Please cite this article as: Ramos Valencia OA, Buitrón Gonzalez Y, Sotelo Daza J, Villaquiran AF. Factores asociados a la intención de vacunación contra el COVID-19 en Popayán, Cauca, Colombia. Vacunas. 2023. https://doi.org/10.1016/j.vacun.2023.01.003