Rathke cleft cysts (RCCs) are asymptomatic benign sellar cysts. Their surgical treatment may lead to a series of well known complications, many of which can be interpreted as failed surgical interventions. We present a retrospective study on patients with treated RCCs that filed a claim for compensation for medical professional liability, with the aim of reporting the medico-legal issues related to the surgical resection of RCC.
A retrospective analysis was performed between 1999 and 2016 on patients diagnosed with RCCs and who underwent surgical resection. The clinical experience of the patients alleging medical liability was analysed by an interdisciplinary group following the European Guidelines proposed by the European Academy of Legal Medicine. Eight patients developed late complications and made a claim for compensation. Only in one case a prognostic error was detected. The pre- and postoperative conditions, as well as the onset of early and late complications are reported and discussed in the paper, as well as the differentiation between “error-free” vs “error-related” complications.
Understanding the underlying causes of the increase in compensation claims, as in the specific case, can help not only in the reduction of errors, but also in the prevention of compensation claims, which result in an increase in public and private spending. One of the main causes of the disproportion between the request for compensation and actual compensation is the expectation regarding surgery and the onset of complications, which could be solved through the appropriateness of consent submitted before the intervention.
Los quistes de hendidura de Rathke (Rathke cleft cysts [RCC]) son quistes sellares benignos asintomáticos. Su tratamiento quirúrgico puede llevar a una serie de complicaciones bien conocidas, muchas de las cuales pueden interpretarse como intervenciones quirúrgicas fallidas. Presentamos un estudio retrospectivo sobre pacientes tratados con RCC que presentaron una reclamación de compensación por responsabilidad profesional médica, con el objetivo de informar los problemas médico-legales relacionados con la resección quirúrgica del RCC.
Se realizó un análisis retrospectivo entre 1999 y 2016 en pacientes diagnosticados con RCC y resecados quirúrgicamente. La experiencia clínica de los pacientes que alegaban responsabilidad médica fue analizada por un grupo interdisciplinario siguiendo las pautas europeas propuestas por la Academia Europea de Medicina Legal. Ocho pacientes mostraron complicaciones tardías e hicieron una reclamación de compensación. Solo en un caso se detectó un error pronóstico. Las condiciones pre y postoperatorias, así como el inicio de las complicaciones tempranas y tardías, se analizarán en el documento, así como la diferenciación entre las complicaciones «sin errores» y las complicaciones que fueron consecuencia de un error médico.
Comprender las causas subyacentes del aumento de las reclamaciones de indemnización, como en el caso específico, puede ser de ayuda no solo en la reducción de errores, sino también en la prevención de reclamaciones de indemnización, que dan como resultado un aumento del gasto público y privado. Una de las principales causas de la desproporción entre la solicitud de compensación y la compensación real es la expectativa con respecto a la cirugía y la aparición de complicaciones, que podrían resolverse mediante la adecuación del consentimiento presentado antes de la intervención.
Rathke cleft cysts (RCCs) are benign sellar cysts and are included between 6% and 10% of sellar lesions.1 They arise from a remnant of the embryological structure, the Rathke pouch, which is typically positioned between the adenohypophysis and the neurohypophysis.2 Small RCCs are often incidentally discovered. Only a small proportion of RCCs exert sufficient mass effect on surrounding structures to result in symptoms such as headache, endocrine dysfunction and visual loss.3 In case of symptomatic RCCs, the aim of surgical management is to drain the cyst content and remove the cystic wall.4 The endoscopic surgery has become the most common approach. In the last two decades, endoscopic transnasal transsphenoidal approaches have become widely used.5
Postoperative complications include a cerebrospinal fluid (CSF) leak (up to 25%) transient and/or permanent diabetes insipidus (respectively up to 67% and up to 20%), anterior pituitary hormone deficits (4–30%), hyponatraemia, meningitis and sinusitis. Headaches and major visual field defects are improved or resolved in a significant number of patients (40–100% and 33–100%, respectively), and hyperprolactinaemia is the most frequently resolved pituitary hormone abnormality. Partial hypopituitarism may recover after surgery (14–50%), whereas panhypopituitarism is seldom resolved.6 In a recent meta-analysis regarding 1151 cases of RCCs undergoing surgical resection, it was observed that the microsurgical transsphenoidal approach had a higher recurrence rate (14% versus 8%) and new endocrine dysfunction rate (25% versus 10%) compared to the endoscopic approach. A subtotal resection is recommended (STR) in all cases of RCCs, apart from recurrences, for which gross total resection (GTR) is indicated.7
Despite the high recurrence rate, as well as the high incidence of complications described in the literature even after surgery, in today's medical practice there are increasing requests for compensation from patients or families with a hypothesis of professional medical liability.8 Many of these requests are based on expectations higher than those actually contemplated ex-ante by the best neurosurgical evidence-based medicine and could be avoided through the promulgation of comprehensive information and the collection of surgical consent, focusing not only on the indication and the type of neurosurgical intervention, but also on the expected outcomes and possible complications, resulting in a significant reduction in costs and public spending.
In the paper we present a retrospective case series of patients with RCCs that underwent surgical management in the healthcare facilities of the north-east of Italy – some of whom filed a claim for compensation – with the aim of evaluating the medico-legal issues regarding the surgical resection of RCC, with reference to the following issues:
- •
preoperative management, postoperative complications and the possible presence of errors in medical conduct;
- •
differentiation between “error-free” and “error-related” complications;
- •
expected outcomes of the surgical intervention as a result of the best neurosurgical evidence-based medicine, to be included in the discussion of the practice of informed consent.
A retrospective analysis was performed between April 1999 and February 2016 on patients with radiological and histological diagnosis of RCCs and who underwent surgical resection. Radiological diagnosis was performed through MRI and/or CT. The patients’ characteristics, preoperative and postoperative data were collected, as follows.
- •
Characteristics of the included cases. Gender and age of the patient, clinical features at the first medical examination, type of surgery.
- •
Preoperative data. The dimensions and location of the lesion detected, preoperative clinical symptoms, ophthalmological (visual field) and endocrine examination (levels of serum prolactin, free T4, thyroid-stimulating hormone, morning fasting cortisol, adrenocorticotropic hormone, insulin-like growth factor-1, follicle-stimulating hormone and luteinizing hormone in women, and free testosterone in men), size and localization at neuroimaging studies (CT and/or MRI) and histological examination.
- •
Postoperative data. A 30-months follow-up, through clinical and instrumental examination, assessing early and/or late complications.
The clinical experience of the patients alleging medical liability was retrospectively analysed by an interdisciplinary group coordinated by the Legal Medicine Unit of the Hospital-University of Padova following the European Guidelines on Methods of Ascertainment and Criteria of Evaluation, proposed by the European Academy of Legal Medicine (EALM) and adopted at international level. This group included specialists in legal medicine (coordinator), neurosurgery, anatomical pathology, endocrinology and urology. In particular, errors and/or non-observance of required rules of professional medical conduct were assessed (patient's consent, diagnosis, prognosis and treatment).9–11
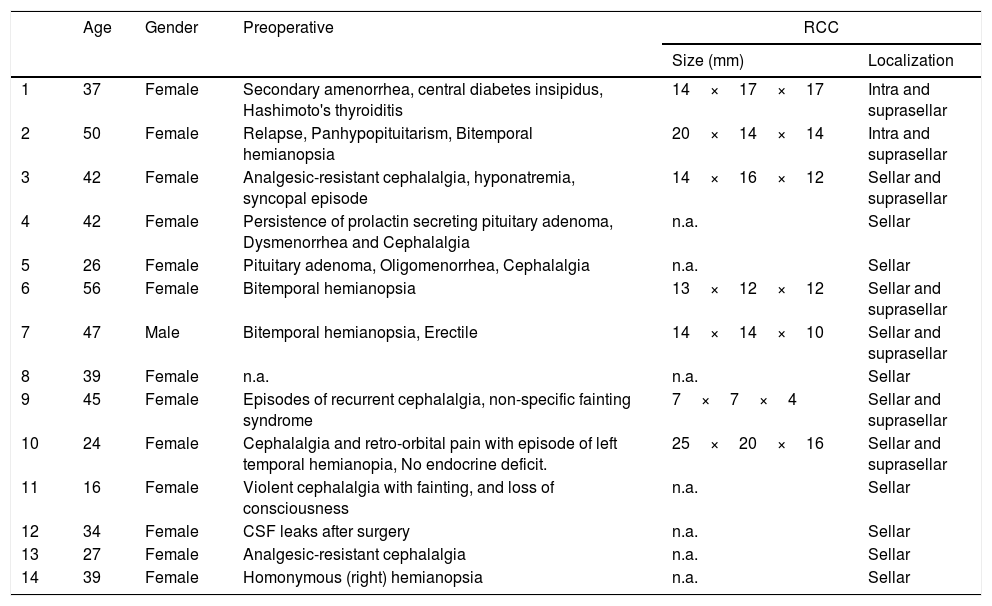
ResultsFourteen patients fulfilled the inclusion criteria: one male and 13 females, with a median age at diagnosis of 37.4 years (range 16–56). Age, gender, preoperative evaluation and size/localization of the RCCs are reported in Table 1. Seven out of 14 cases (50.0%) only showed the presence of an intrasellar cystic lesion; the remaining 7 were characterised by an intrasellar lesion with suprasellar extension. All the lesions were treated with transnasal transsphenoidal surgery. In 1 case it was impossible to trace preoperative clinical data.
Gender, age, and preoperative conditions are reported.
| Age | Gender | Preoperative | RCC | ||
|---|---|---|---|---|---|
| Size (mm) | Localization | ||||
| 1 | 37 | Female | Secondary amenorrhea, central diabetes insipidus, Hashimoto's thyroiditis | 14×17×17 | Intra and suprasellar |
| 2 | 50 | Female | Relapse, Panhypopituitarism, Bitemporal hemianopsia | 20×14×14 | Intra and suprasellar |
| 3 | 42 | Female | Analgesic-resistant cephalalgia, hyponatremia, syncopal episode | 14×16×12 | Sellar and suprasellar |
| 4 | 42 | Female | Persistence of prolactin secreting pituitary adenoma, Dysmenorrhea and Cephalalgia | n.a. | Sellar |
| 5 | 26 | Female | Pituitary adenoma, Oligomenorrhea, Cephalalgia | n.a. | Sellar |
| 6 | 56 | Female | Bitemporal hemianopsia | 13×12×12 | Sellar and suprasellar |
| 7 | 47 | Male | Bitemporal hemianopsia, Erectile | 14×14×10 | Sellar and suprasellar |
| 8 | 39 | Female | n.a. | n.a. | Sellar |
| 9 | 45 | Female | Episodes of recurrent cephalalgia, non-specific fainting syndrome | 7×7×4 | Sellar and suprasellar |
| 10 | 24 | Female | Cephalalgia and retro-orbital pain with episode of left temporal hemianopia, No endocrine deficit. | 25×20×16 | Sellar and suprasellar |
| 11 | 16 | Female | Violent cephalalgia with fainting, and loss of consciousness | n.a. | Sellar |
| 12 | 34 | Female | CSF leaks after surgery | n.a. | Sellar |
| 13 | 27 | Female | Analgesic-resistant cephalalgia | n.a. | Sellar |
| 14 | 39 | Female | Homonymous (right) hemianopsia | n.a. | Sellar |
n.a., not available.
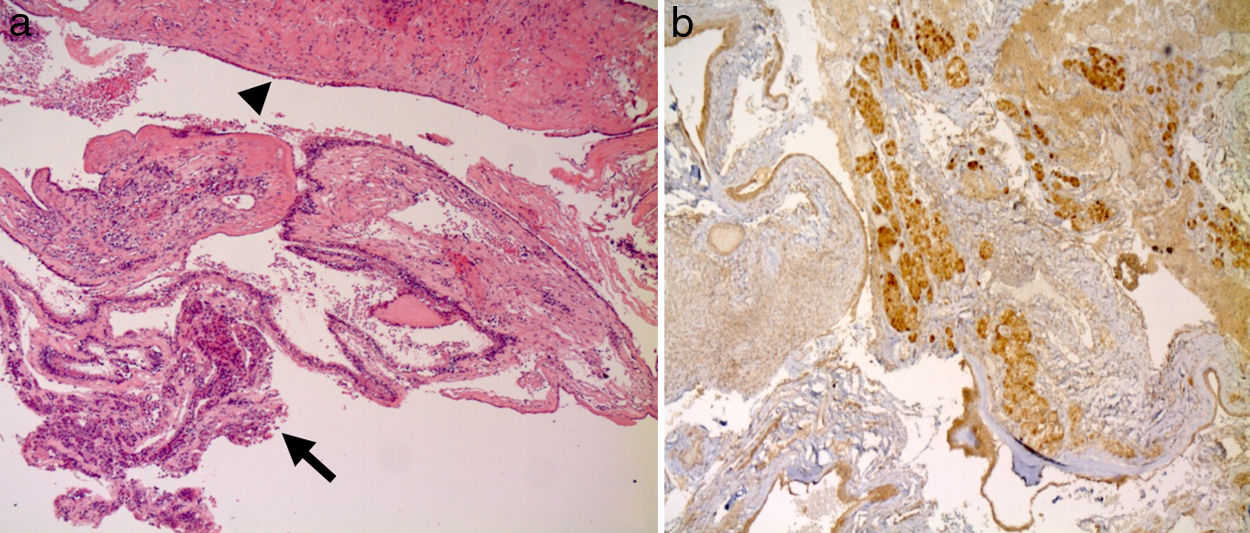
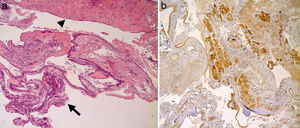
In 10 out of 14 cases (71.4%) the diagnosis of Rathke cleft cysts was made with imaging techniques and confirmed through histology (Fig. 1). Among the 4 cases in which imaging techniques led to the suspicion of the presence of a secreting pituitary adenoma, in 2 cases the histological examination showed no secreting element and diagnosed Rathke cleft cysts, while in the remaining 2 cases it showed the concomitant presence of secreting pituitary adenoma and Rathke cleft cyst.
(a) Images of cysts of Rathke's pouch, which show prevailing monolayer columnar epithelium of cystic wall (arrow) with focal phenomena of squamous metaplasia (arrowhead); (b) Proportion of healthy pituitary tissue removed during resection of the cyst wall, visible with immunohistochemical studies that detect the weak positivity for ACTH and FSH.
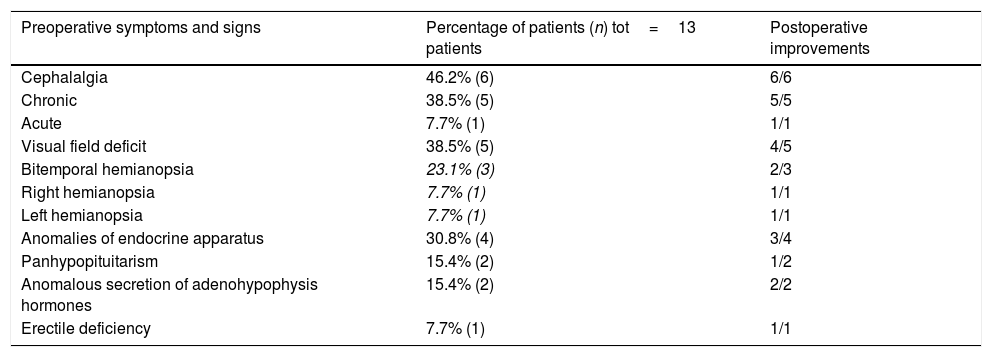
Table 2 reports the preoperative clinical symptoms and the postoperative improvements. Chronic and/or acute cephalalgia was present in 6 out of 13 cases (46.2%); visual field deficits (left or right hemianopsia, bitemporal hemianopsia) were detected in 5 cases (38.5%); hormonal deficit of adenohypophysis were detected in 2 out of 13 cases (15.4%); and the anomalous secretion of adenohypophyseal hormones in 2 out of 13 cases (15.4%) due to the presence of a secreting pituitary adenoma. In 10 out of 14 cases a clinical improvement was observed. A resolution of cephalalgia occurred in all the cases and, in 4 cases out of 5, the visual field deficit was resolved. In one case a slight improvement of the temporary hemianopsia in the left eye and temporal inferior field scotoma in the right eye occurred. In 3 out of 4 cases the hormonal deficit or the preoperative hormonal disorder/anomaly were resolved, while in 1 case the preoperative clinical picture of central diabetes insipidus and secondary amenorrhea remained unchanged.
Preoperative and postoperative clinical data: frequencies of signs and symptoms. Postoperative improvements of signs and symptoms.
| Preoperative symptoms and signs | Percentage of patients (n) tot=13 patients | Postoperative improvements |
|---|---|---|
| Cephalalgia | 46.2% (6) | 6/6 |
| Chronic | 38.5% (5) | 5/5 |
| Acute | 7.7% (1) | 1/1 |
| Visual field deficit | 38.5% (5) | 4/5 |
| Bitemporal hemianopsia | 23.1% (3) | 2/3 |
| Right hemianopsia | 7.7% (1) | 1/1 |
| Left hemianopsia | 7.7% (1) | 1/1 |
| Anomalies of endocrine apparatus | 30.8% (4) | 3/4 |
| Panhypopituitarism | 15.4% (2) | 1/2 |
| Anomalous secretion of adenohypophysis hormones | 15.4% (2) | 2/2 |
| Erectile deficiency | 7.7% (1) | 1/1 |
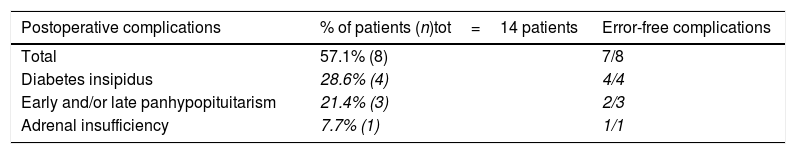
Table 3 reports postoperative early and/or late complications and the identification of “error-free complication”. Eight out of 14 cases (57.1%) developed early and/or late, temporary and/or permanent complications. Four patients (26.6%) developed an early triphasic diabetes insipidus occurred and developed into permanent central diabetes insipidus. In 3 cases (21.4%) early and late panhypopituitarisms occurred. In 1 case an adrenal insufficiency occurred.
Postoperative early and/or late, temporary and/or permanent/persistent complications.
| Postoperative complications | % of patients (n)tot=14 patients | Error-free complications |
|---|---|---|
| Total | 57.1% (8) | 7/8 |
| Diabetes insipidus | 28.6% (4) | 4/4 |
| Early and/or late panhypopituitarism | 21.4% (3) | 2/3 |
| Adrenal insufficiency | 7.7% (1) | 1/1 |
All 8 patients who developed early and/or late complications filed a claim for compensation for professional liability, which was reviewed by the Legal Medicine unit of the University-Hospital of Padova. This evaluation pointed to the presence of a “true error” in one case (Case 9 of Table 1). In fact, compared to a cyst of the small Rathke pocket, of a maximum diameter of 7mm and therefore inferior to the diameter of 10mm, and in the absence of signs or symptoms of compression in the surrounding structures (campimetric deficits, endocrinological pathologies and/or chronic headache), surgery was performed to remove the lesion by endoscopic transsphenoid, which was not indicated. In this case, a prognostic error was identified and all the complications resulting from the intervention, foreseeable but not preventable (permanent panipopituitarism), were compensated in civil proceedings.
In the remaining cases, no medical error was found in any phase of the medical conduct (patient's consent acquisition; diagnosis, prognosis, treatment). The evaluation of the interdisciplinary group (performed in the prejudicial phase) was also confirmed in the judicial phase, since in no case has a judgment in a civil case been made to the detriment of the hospital.
DiscussionPreoperative dataDemographic data are in line with the reported studies: a mean age of 37.4 years, and 93% of patients were female.12–16 Headache is the most prevalent manifestation, with reported frequencies between 33% and 81%6; frontal, episodic, non-pulsating, bilateral headache or deep retroorbital pain are the most common.17 Visual loss has been reported to develop in 11–67% of patients undergoing surgical intervention and may include deficits in visual fields as well as in visual acuity.4,14,18 In a published series of surgically treated RCCs, gonadotrophin deficiency was found in 60%, ACTH deficiency in 36%, TSH deficiency in 36% and hyperprolactinaemia in 31% of the cases.19 GH deficiency has also been reported in 12–79% of the patients,6 while diabetes insipidus in approximately 7–20% of them.3 In this series, headache was the most common clinical feature at presentation (46.2%), visual field defects were identified in 38.5% of the subjects, while endocrine disturbances (panhypopituitarism and hyperprolactinaemia) in 30.8%. In two cases, the RCCs co-existed with a prolactinoma that caused hyperprolactinaemia.
At RM, RCCs often appear as well-circumscribed, centrally located spherical or ovoid lesions of the sellar region; the signal intensity of cyst contents on MR images demonstrates high variability on T1 and T2 sequences and has been reported to correlate with the nature of the cystic contents.20 Alternatively, on CT, they usually appear as low or isodensity homogeneous lesions or with slight hyperdensity relative to the brain parenchyma.6 However, the anatomo-pathological analysis remains the gold standard of diagnosis, which reveals some characterising features of RCCs, showing a cyst wall lined by simple cuboidal or columnar epithelium with or without cilia and occasionally goblet cells secreting mucous into the cyst; pseudostratified, columnar, ciliated respiratory-type epithelium may be present in up to 49% of cases.21 In our case series, the RCCs were pre-operatively investigated with CT or with MRI, and subsequently confirmed at the anatomo-pathological diagnosis; however, CT or MRI had poor sensibility (71.4%), in accordance with the previous literature data,20 and the gold standard for establishing a diagnosis of RCC was the histopathological analysis of the cyst wall.
In this case series, the range of RCC size was from 7 to 25mm; however, in the study, the detected range is affected by a bias, that is, a sellar lesion has been included that should have been considered inoperable. Indeed, the lesion measured 7mm and was asymptomatic and, as such, it should have been observed with laboratory and instrumental investigations over time. Excluding this lesion, the size range is included between 10 and 25mm in diameter, according to the data reported in literature.22,23
Postoperative improvements and complicationsSurgical intervention improved visual field defects in 80% (4/5) of the subjects and headache in all the patients. In our study, we found a considerable improvement of endocrine disturbances (75% of the subjects), although most of these (2/3) are attributable to the resolution of hyperprolactinaemia due to surgical resection of a co-existed prolactinoma, while hypopituitarism and panhypopituitarism had a poor prognosis.
Because of the particular position of RCC (the intermediate lobe of the pituitary gland), the endoscopic resection surgery of this benign lesion is not exempt from immediate and/or late postoperative complications, some of which are serious or disabling. Postoperative complications include transient and/or permanent diabetes insipidus, anterior pituitary hormone deficits, hyponatraemia, meningitis and sinusitis. Literature data show that headaches and major visual field defects improve or are resolved in a significant number of patients (33–100%), and hyperprolactinaemia is the most frequently resolved pituitary hormone abnormality (in most series, in 100%). Partial hypopituitarism may recover after surgery (14–50%), whereas panhypopituitarism seldom resolves.6 In our study, the most frequently identified postoperative complications are panhypopituitarism and diabetes insipidus; those complications are not associated with the dimensions of the lesion or with its position.
The majority of clinical and epidemiological studies reporting early and late outcomes following surgery for RCC do not differentiate between “error-free complication” (also named clinical complication) and “error-related complications”. The differentiation not easy, since it must be the result of an interdisciplinary assessment of medical liability of each case and, if possible, through an external second opinion (i.e. legal outcome). In this study we observed that, among the complication observed, only in one case the negative outcome was preventable through a different medical approach. In other cases, no errors were detected, and the poor outcome was classified as “error free complication” in all cases.
Medico-legal considerationsAmong high-risk medical specialists, neurosurgeons remain disproportionately at risk of facing a lawsuit.24 Procedural error was the most commonly cited basis for litigation. In the United States, failure to diagnose and to treat a preexisting condition were the next 2 most commonly alleged reasons for malpractice.25
Since the natural history of RCCs is still completely unclear, neither guidelines nor consensus conferences about the management of RCCs exist, and the suspected errors in our cases have been evaluated in accordance to source hierarchy (operational procedures – evidence based publications – national literature). In these specific cases, evidence based publications referred to the times when event occurred have been used.2,3 In 7 of the 8 cases in which there was the hypothesis of professional liability, the presence of errors in the diagnostic–prognostic–therapeutic phases was excluded. Only in case 9 (Table 1) an error was detected. In fact, compared to a cyst of the small Rathke pocket, equal to 7mm of maximum diameter and therefore inferior to the diameter of 10mm, and in the absence of signs or symptoms of compression in the surrounding structures (campimetric deficits, endocrinological pathologies and/or chronic headache), surgery was performed to remove the lesion by way of endoscopic transsphenoid, which was not indicated. As a result of this, a permanent panipopituitarism developed, which was fully compensated.
The cause of the disproportion between the request for compensation and actual compensation must undoubtedly be sought in the expectations of surgery and the onset of complications. All the patients included in the present study signed an informed consent form. It represents a generic preprinted model, valid for any neurosurgical intervention and which refers to the oral communication of the information regarding the benefits and risks and/or complications of the neurosurgical intervention. However, the eight patients experiencing early/late complications complained of a lack of consent to neurosurgical intervention and/or other medical errors. This evidence stimulated our medical-legal evaluation regarding the importance of a detailed informed consent form, as accurate and comprehensive as possible and adapted, in anticipation, to the complications that may occur not in a generic way, but in relation to the specific case. In fact, understanding the underlying causes that led patients to start a lawsuit against healthcare professionals is the first step for: (i) reducing real medical errors that would led to an economic compensation and (ii) reducing perceived malpractice risk among neurosurgeons, that may led practitioners to eliminate high risk procedures and contribute to the practice of defensive medicine, with its negative impact in the healthcare system (i.e. quality of care, limit access to care, increased costs of healthcare delivery).26
The aim of informed consent documents is for the patient to have all necessary and sufficient information in order to be able freely to choose or reject a treatment or a diagnostic test. Several authors27–30 studied the subject of informed consent in neurosurgery, under the assumption that in the majority of neurosurgical cases patients expect particular kinds of results and, when the outcomes are poorer or different, they reflect on what they had understood or believed they would be provided. Diverse complications may occur in patients that underwent endoscopic neurosurgeries due to other sellar pathologies (craniopharyngioma, pituitary adenoma, etc.), and a single informed consent for each surgical approach, instead of for each pathology, has been proposed.31 Informed consent should indicate the distinctions between postoperative complications that are divided into common (with an incidence rate higher than 5%): infections of the surgical site, bleeding, adenohypophysis dysfunction, CSF leak, and incomplete removal of the tumor; uncommon (with an incidence rate between 1 and 5%): myocardial infarction, cerebral ischemic stroke, temporal or permanent visual disturbance, meningitis, infection of abdominal autologous fat; rare (incidence rate<1%): uncontrolled epistaxis and death. Thanks to a precise and detailed form, including explicative pictures, the communicative and informative process could be useful, particularly in grey areas (big but asymptomatic cysts or minimal alterations in instrumental results where visual or endocrine deficit do not occur), where the recommendations are not shared and the benefit-risk evaluation given by the conversation between doctor and patient could lead to the best decision and the establishment of a relationship of trust between doctor and patient.
The second issue raised by our retrospective study is the indication for surgery. Although there are no Guidelines of reference, our study confirms the recommendation of the affiliation to the current management, consisting in the operability of cysts with a diameter greater than 10mm, or that display symptoms (recurrent cephalalgia, visual field defects and hormonal deficit of the pituitary–hypothalamic axis). The acceptance of those indications should allow doctors to decrease risks associated with the development of postoperative complications leading to lawsuits, also from a medical-legal point of view. However, the best treatment for big but asymptomatic lesions is still a subject of discussion: if a clinical and instrumental follow up should take place (every 3 months) or the patient should undergo surgery to avoid the growth of the lesion and the onset of permanent pathologies.
ConclusionMedical liability has become a fact of life in the physician's modern practice and each malpractice claim gives rise to a scientific challenge.32–36
Measuring the consequences of medical care on patient outcomes a differentiate between “non-error” and “error-related” complications is an important prerequisite for creating a “culture of learning from our mistakes”. A proper and comprehensive reflection is required, made on a case by case basis, regarding the risks and benefits of the resection of Rathke cleft cyst, in order to establish the best management for that patient, in the context of the new concept of the medicine of the third millennium, to be understood as “personalised medicine”.
The implementation of the International Guidelines on Malpractice and Medical Liability in all specialities of medicine will bring improvements in claims handling practice and will ensure data for research for this field, which should represent a step towards prevention and patient safety.9,37 A better understanding of the medical liability, especially in rare or uncommon medical conditions, may help liability insurance system in covering optimally and effectively potential defects of medical praxis, and in promoting improvements in clinical safety and help preventing the situation of “malpractice crisis” reported in abroad.38
Ethical approvalThis article does not involve any procedure with human participants or animals performed by any of the authors and ethical principles were respected throughout the claims’ analysis.
FundingNo funding was received for this research.
Conflict of interestThe authors declare that there is no conflict of interest.