Chronic intestinal pseudo-obstruction is a rare but severe disease. Often passes unrecognized for long time.
Case Report75-year-old Hispanic male with a history of Parkinson ¿s disease, Diabetes Mellitus Type 2 and Chronic Arterial Hypertension. He came to the ER with a 5 day progressive evolution of abdominal pain, distension, hyporexia and obstipation. A laparotomy was performed where we found a distended colon. We proceeded with a total colectomy and ileostomy. The specimen was 222x14x14cm with a thin muscularis propria and present lymphatic cells. Post-operative course was unremarkable. The patient was sent home 48hr after the surgery tolerating soft diet.
DiscussionThe main causes are idiopathic, diseases of central autonomic and enteric nervous systems, immune, collagen and metabolic diseases. Surgery is intended when there is multiple organ failure, important distention or failure of the medical treatment.
ConclusionThis case report highlights the importance of differential diagnosis and treatment of non-mechanical intestinal obstruction secondary to the effects of anti-parkinsonians, metabolic or idiopathic nature. With good surgical technique a positive outcome is likely.
La pseudo-obstrucción intestinal crónica es una enfermedad rara y severa. Muchas veces pasa desapercibido o tratado con diagnósticos incorrectos.
Caso clínicoMasculino de 75 años con antecedentes de Parkinson, Diabetes Mellitus tipo 2 e Hipertensión Arterial Sistémica. Inicia 5 días previos con dolor abdominal, hiporexia, constipación, obstipación, astenia, adinamia y nausea. Presenta distensión abdominal, aperistalsis, dolor y timpanismo. En las radiografías muestra distensión de colon generalizado. Se decide realizar Laparotomía Exploradora encontrando colon dilatado en su totalidad, sin obstrucción mecánica. Se realiza colectomía total e ileostomía. El paciente evoluciona de forma favorable sin complicaciones. El resultado histopatológico: espécimen de 222x14x14cm con adelgazamiento de la muscular propia y células ganglionares presentes.
DiscusiónLas principales causas son idiopático, enfermedad del sistema nervioso autonómico, enfermedades de la colágena o metabólicas. El cuadro clínico son episodios recurrentes de dolor abdominal, distensión, constipación y obstipación. Se considera la cirugía cuando existe falla orgánica múltiple, distensión importante o falla del tratamiento médico.
ConclusiónEste caso debuta con un cuadro obstrucción intestinal no mecánica que pudiera ser de origen idiopático, secundaria a fármacos o metabólico. La colectomía con ileostomía es una alternativa quirúrgica aceptable y segura.
Chronic intestinal pseudo-obstruction (CIPO) is a rare and severe disease characterized by the failure of the small bowel or colon to propel the contents of the intestinal tract simulating mechanical occlusion1–3. It is one of the most important causes of chronic intestinal failure affecting both pediatric population (15%) and adults (20%). The ultimate result is an important nutritional deficiency. Often overlooked or misdiagnosed until complications or clinical symptoms1 appeared. Constipation on the other hand, is one of the most common diseases with an incidence of 5-20%4.
Case ReportA 75 years old male who was admitted to our hospital due to abdominal pain and distention. It started five days before admission, with colic generalized abdominal pain, after food ingestion, intensity 4 out of 10, with partial improvement with Acetaminophen. Associate with anorexia, constipation and progressive obstipation. One day prior to admission, the patient refers fatigue, weakness and nausea without vomiting. He was treated with enemas and antibiotics without changes, so he decided to attend to our hospital. On admission, physical examination highlights tachycardia, dehydration, major abdominal distention, absence of bowel sounds, pain on superficial and deep palpation, negative sign of peritoneal irritation, generalized bloating, consistent with bowel obstruction. Laboratory findings highlight pre-renal failure, hyperglycemia, hypokalemia, hypocalcemia and metabolic acidosis. Blood count and liver function tests were within normal parameters. The patient has a 10 year history of Parkinson's disease treated with amantadine 100mg every 8hours, levodopa / carbidopa 250mg / 25mg every 8hours. Also, Diabetes Mellitus treated with metformin and systemic hypertension in treatment with felodipine 5mg every 12hours. Surgical history of transurethral prostatic resection 10 years ago.
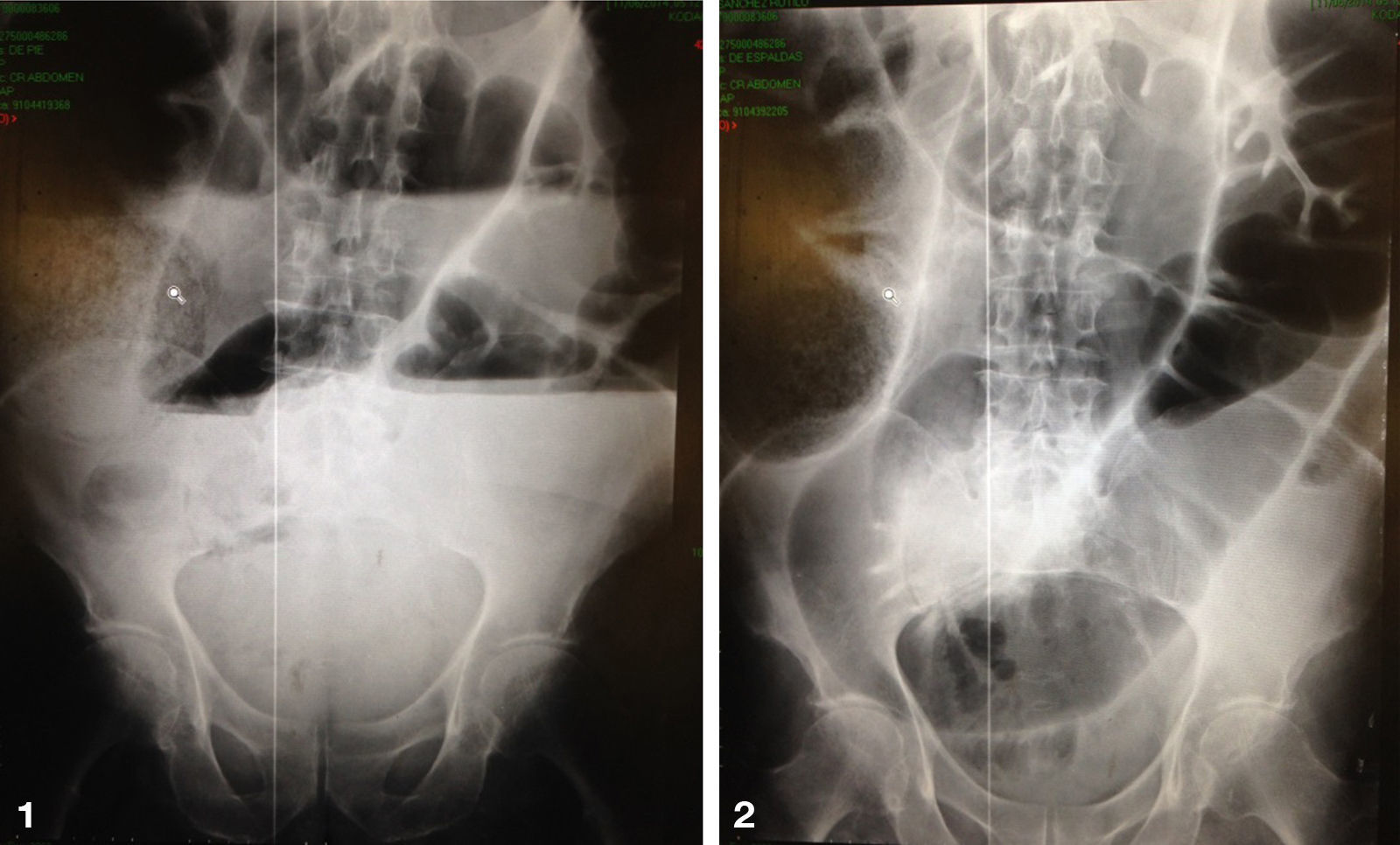
The initial treatment was electrolyte management, nasogastric decompression, Foley and central venous catheter. Plain abdominal radiographs in two positions showed distended colon, with a cecum over 14cm in diameter, and a redundant transverse colon and sigmoid (Figure 1 and 2).
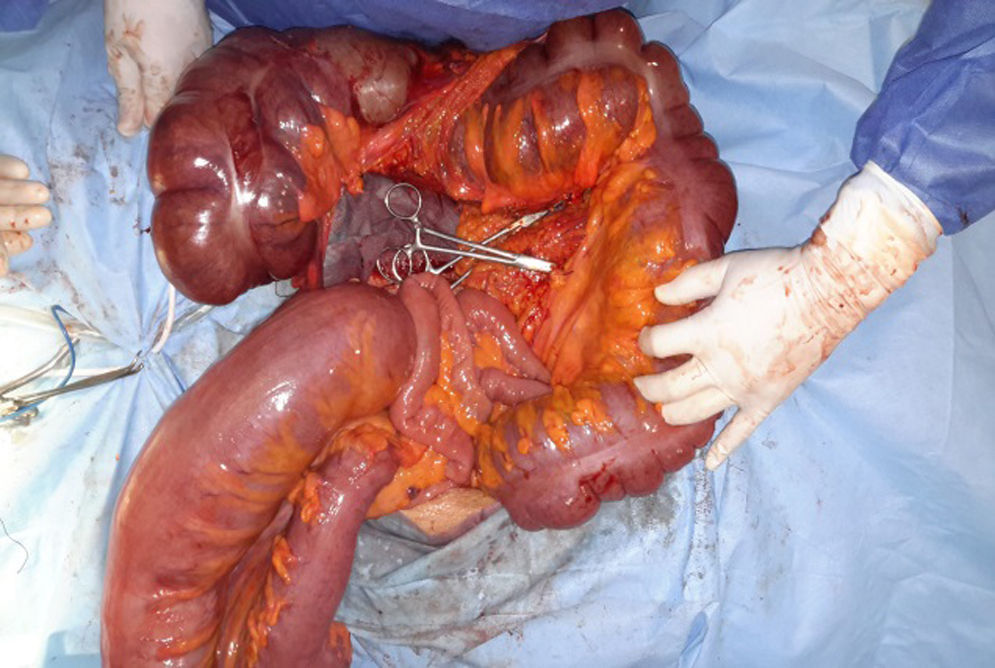
We decided to perform an exploratory laparotomy and it was found a fully dilated colon, cecum 18cm in diameter, transverse colon 12cm in diameter, descending and sigmoid colon 15cm in diameter; without macroscopic evidence of mechanical obstruction anywhere (Image 3 and 4). The small intestine macroscopically normal. We perform a total colectomy, closure of the rectum with Hartmann's procedure and ileostomy. The posoperative outcome of the patient was favorable, tolerated oral diet 12hrs after surgery, and a functional ileostomy 24hrs after surgery. His family requested to take home the patient 48hrs postoperatively for economic reasons, however, stable. Phone monitoring is done a week of discharge, referring asymptomatic, functional ileostomy with approximately 500cc a day.
The pathology reports a specimen macroscopically of 222x14x14cm with congestive surface, ileum 8cm long and appendix of 9x0.6x0.6cm; flattened mucosa, light brown and slightly congestive (Figure 5). In histological sections of the muscularis, they observed present ganglion cells without dysplasia. The histopathological diagnosis reports mild nonspecific colitis consistent with chronic idiopathic intestinal pseudo-obstruction and acute peritonitis.
DiscussionThe main causes of intestinal pseudo-obstruction can be divided into: 1) idiopathic (Ogilvie syndrome), 2) both enteric disease or central autonomic nervous system (stroke, encephalitis, basal ganglia calcification, orthostatic hypotension, Von Recklinghausen disease, Hirshsprung disease), 3) collagen diseases (paraneoplasic, scleroderma, dermatomyositis, amyloidosis, Ehlers-Danlos syndrome, lupus, among others), 4) endocrine and metabolic diseases (diabetes mellitus, hypothyroidism, hyperparathyroidism, pheochromocytoma), 5) drugs (clonidine phenothiazines, antidepressants, antiparkinsonian, antineoplastic, bronchodilators, anthraquinone), and 6) other (iatrogenic, yeyunal diverticula and Chagas disease) (1,3). The autonomic etiology is the most comun patology, specifically in the colon4,6.
The typical clinical features are recurrent episodes of abdominal pain, bloating, constipation and obstipation, with or without nausea, vomiting, dysphagia and weight loss1,3,5. Only 25% of patients presents an acute episode, where radiographical findings are dilated bowel loops and air-fluid levels. Entero-CT can be done to rule out mechanical occlusion1,2. The natural course of the disease is usually progressive deterioration and chronically malnutrition. The most frequent causes of death are related to the parenteral nutrition, transplant or post-surgical complications due to septic shock which is observed in 50% pf patients 5 years from treatment1.
The initial treatment during the acute episode is intravenous fluids and electrolytes, abdominal decompression with a nasogastric or rectal tube, colonoscopy or cecostomy; tegaserod, cisapride, erythromycin, somatostatin or octreotide and / or neostigmine (1.5). The pucalopride can also improve the chronic state (6).
The diagnosis is made with full thickness biopsies. Surgery is considered when signs of multiple organ failure appeared, important abdominal distension or failure of medical treatment, which occurs in 58% of patients1,2,7. Indications of medical treatment failure are younger age, chronic disease, bloating as the main symptom and major cecum distention2.
Current Surgical treatment for megacolon7:
Colon Procedures:
- •
Subtotal colectomy: 71% therapeutic success (75% ileo-sigmoid anastomoses, 77% ileo-rectal anastomoses, 50% ceco-rectal anastomoses). Mortality up to 14%,complication rate of 25% secondary to anastomotic complications, recurrent intestinal obstruction (14.5%), and fecal incontinence (20%).
- •
Segmental colectomy: 48.4% therapeutic success, mortality and morbidity of 2.3% to 13% with reoperation rate of 23.8%.
Rectal Procedures:
- •
Anterior rectal resection: there is only one study reporting a success of 75% with a 50% of complication rate.
- •
Proctectomy: treatment success of 71%, mortality 6.5%, morbidity 6.5% and 9.7% reoperation for recurrent constipation (14-17%).
- •
endorectal pull-through: only one study was performed in 4 patients with 25% mortality, 75% morbidity, reoperation 50% pelvic abscess.
- •
Duhamel procedure: therapeutic success. 87%, 3% mortality, 60% morbidity (rectovaginal fistula or bowel, pelvic abscess, anastomotic stricture), recurrent constipation 7%.
- •
Vertical rectoplastia: new procedure, only one study reported in the therapeutic success of 83%, 17% morbidity (fistula) and no mortality.
- •
Restorative proctocolectomy: 73% treatment success, mortality 0%, 0-40% morbidity (anastomotic leakage, nocturnal fecal incontinence).
Pelvic Floor Procedure:
- •
Internal Sphincterotomy: as beneficial in 33% and 40% secondary procedure when it is primary.
- •
Division puborectalis: No evidence of being a functional procedure for this condition.
Stoma: 40-100% treatment success, mortality 0%, morbidity 17%.
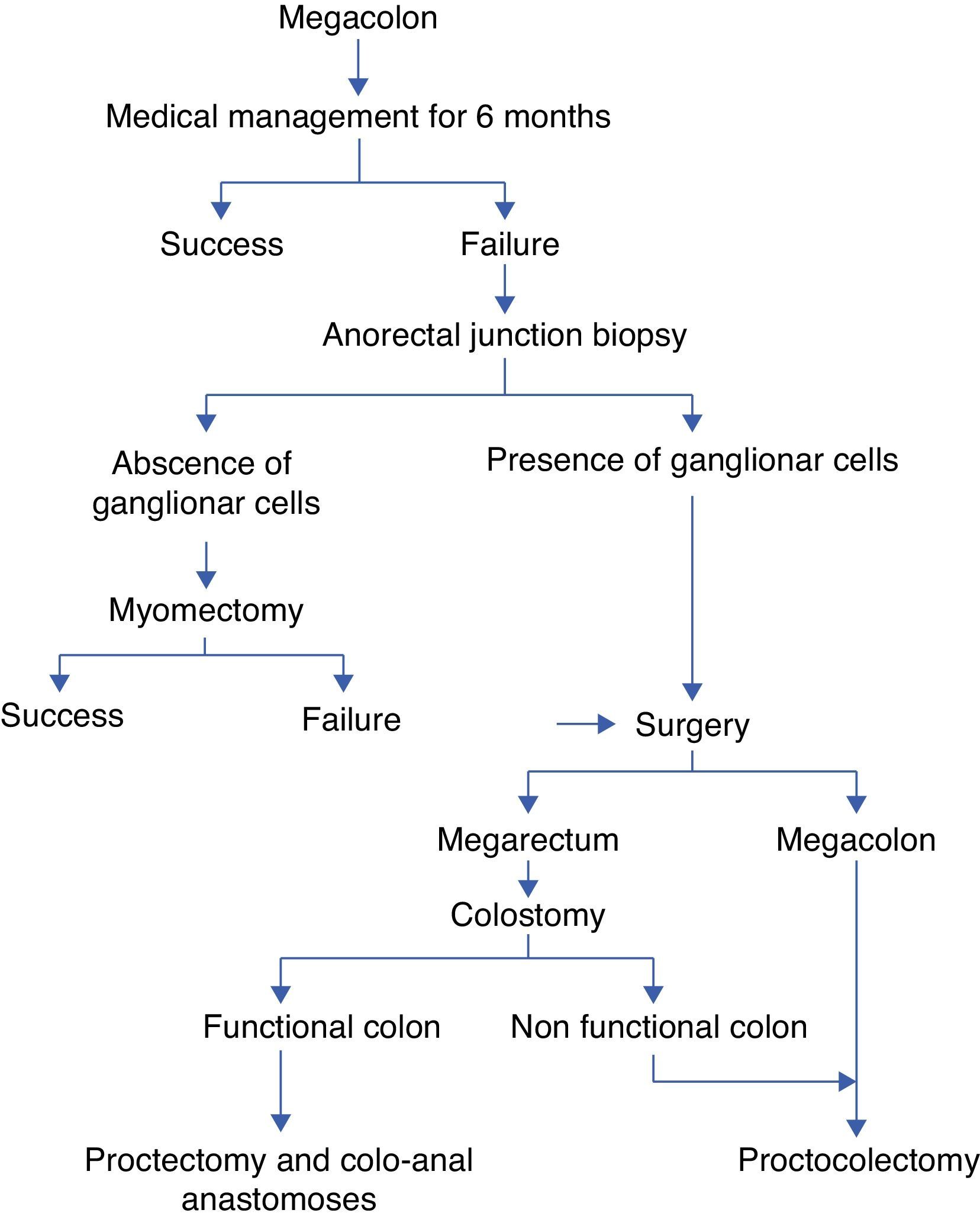
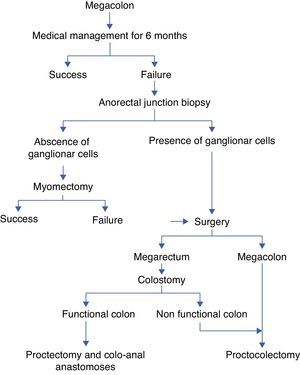
CB Ó Súilleabháin8 proposes the following treatment scheme megacolon (Fig. 6).
Eon Han Chul4 in a study of 33 patients with colonic pseudo-obstruction, postoperative complications reported in 22% of patients with the most frequent surgical wound infection, followed by ileus, intra-abdominal abscess and diarrhea.
ConclusionIn the case of our patient, presented clinical data of no mechanical bowel obstruction that may be idiopathic or secondary to drugs, especially anti-Parkinson. He presented a favorable postoperative evolution with possible intestinal reconnection in 3-6 months. We decided not to perform the anastomosis in the same surgical procedure by not having an accurate diagnosis and information about the absence of ganglion cells or commitment anorectal complex, however, based on the good performance, we propose the combination of colectomy with ileostomy in patients managed as a surgical emergency, although further studies are requiered to determine the usefulness of this therapeutic approach.