In recent years, there has been an increase in claims against doctors for alleged malpractice. Our objective was to retrospectively analyze complaints of medical liability in the courts of Barcelona between 2004 and 2009, evaluated at the Institute of Legal Medicine and Forensic Sciences of Catalonia.
Material and methodWe used 3 databases: the first, the 283 forensic reports prepared by forensic doctors during those years; the second, the judicial computer programme TEMIS-2; and the third, a review of judicial sentences.
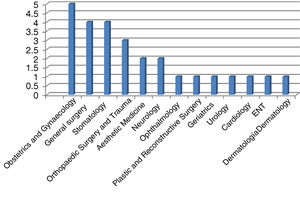
ResultsIn 257 cases (90.81%) the claim was criminal, 18 (6.36%) contentious-administrative proceedings, 5 civil (1.77%) and 3 Prosecutor's Office claims (1.06%). The average age was 48.38 years (SD±19.39), in 62.77% the injured party was a woman, and they suffered more sequelae. In 88.34% the claim was against a doctor, a poor therapeutic outcome being the most common (32.86%). The most reported specialties were traumatology, obstetrics and gynaecology, and general surgery. There were more complaints in private healthcare. In 72.41% of the cases that came to trial the sentence was acquittal, and of the 8 convictions, only one was imprisoned. The median time to sentencing was 1602 days.
ConclusionsThe criminal route is the most frequent. Women claim more and suffer more consequences. Surgical specialties are the most reported. In 27.59% of the cases that came to trial there were convictions, and only one resulted in deprivation of liberty.
En los últimos años ha habido un incremento de reclamaciones contra médicos por presunta mala praxis. Nuestro objetivo ha sido analizar retrospectivamente las denuncias por responsabilidad médica en los juzgados de Barcelona durante los años 2004-2009, evaluadas en el Instituto de Medicina Legal y Ciencias Forenses de Cataluña.
Material y métodoSe realizó a partir de 3 bases de datos: la primera, las 283 periciales elaboradas por los médicos forenses durante estos años; la segunda, el programa informático judicial TEMIS-2; y la tercera, revisión de sentencias judiciales.
ResultadosEn 257 casos (90,81%) la reclamación fue penal, 18 (6,36%) procedimientos contencioso-administrativos, 5 civiles (1,77%) y 3 de Fiscalía (1,06%). La edad media fue de 48,38 años (DE±19,39), en el 62,77% la perjudicada fue una mujer, siendo estas las que sufrieron más secuelas. En el 88,34% la reclamación era contra un médico, siendo la más habitual el mal resultado terapéutico (32,86%). Las especialidades más denunciadas fueron la traumatología, obstetricia y ginecología y cirugía general. Hubo más reclamaciones en la sanidad privada. En el 72,41% de los casos que llegaron a juicio la sentencia fue absolutoria y de los 8 que fueron condenados, solo en uno hubo prisión. La mediana del tiempo hasta la sentencia fue de 1.602 días.
ConclusionesLa vía penal es la más frecuente. Las mujeres reclaman más y sufren más secuelas. Las especialidades quirúrgicas son las más denunciadas. En el 27,59% de los casos que llegaron a juicio hubo sentencias condenatorias y solo en uno privación de libertad.
In 1923, Lucas-Championnière stated that the problem of medical liability is becoming more serious and distressing every day, and it worries all doctors. He added that “if we do not want to end the charitable initiative that can cure the sick, it is very important to protect the honest and conscientious doctor from unjust persecution”. These remarks remain pertinent, given the growing number of medical claims.1 The protection of health is a right; whereas doctors used to be “sanctified” they are now considered “guilty” in frustrating aspects of life that cannot be solved: illness and death.2
Different countries have witnessed a progressive increase in the number of claims against doctors for alleged malpractice. Some of the factors that could explain this situation include the tendency of people nowadays to attempt to increase their safety by seeking causes and liabilities for an event that has generated damage3; the technification and massification of medicine; patients do not deal directly with their own doctor but rather a team that forms part of an anonymous health institution from which they demand responsibility3,4; the high demand for services resulting in less time spent with patients, along with the practice of more sophisticated and aggressive techniques that increase the risk of adverse effects. Some authors consider that civil liability insurance could be financial motivation that is increasing the risk of claims in certain circumstances.2 Studdert et al. summarise the causes of the increase in claims as there being greater public awareness of medical errors and less confidence in the health system, technological advances and innovation, and increased medical activity.5
Patient safety is a new dimension of healthcare quality which has become very relevant in recent years, since without it the likelihood will increase that other aspects such as effectiveness or patient satisfaction will be negatively affected.6 It can be defined as reducing the risk of causing unnecessary harm while delivering healthcare.7 An adverse effect or event is defined as any incident that causes harm to the patient and is associated with the care process.7,8 Current trends indicate that patient safety must be the foundation for good quality healthcare and that it must be based on prevention as well as information, analysis and reporting by health professionals of incidents that occur during the care process.9
The safety culture that predominates in our country's organisations is characterised by a tendency to hide errors, individualism and identifying a culprit as the end solution.10 Our aim is to improve the quality of care, seek avoidability in order to implement policies that improve patient safety in health systems.8 The objective is to develop strategies to control adverse events. Frequency, severity, impact and avoidability are the keys to guiding organisations in the design of more effective strategies for improving patient safety. According to the study conducted by Aranaz-Andrés et al. in Spanish hospitals, out of a sample of 5624 patients, 112 died, 23 as a result of an adverse event.8 The incidence of death in patients with adverse reactions was 4.4%. In 15 of the patients who died, there were associations between the adverse event and death, and in 7 it was considered the direct cause of death. Among the adverse events related to death, half were considered avoidable.8
Traditionally, it is the professional practitioner who is blamed as triggering the error. The new systems theory assumes that errors are the result of system failures and that it is therefore necessary to analyse and learn from them, to identify them, look for the causes of the system that has caused them and redesign them according to the results of analyses.9,11
The main objective of this study was to analyse, quantitatively and qualitatively, the claims filed for alleged medical liability in the city of Barcelona during the years 2004–2009, using data from the archive of the Clinico-Medical Legal Service of the Institute of Legal Medicine and Forensic Sciences of Catalonia. Secondary objectives were to study the most frequent reasons for claims, to determine the medical specialties with the greatest risk of having a case brought against them, to evaluate the health area against which the most complaints are made and to analyse the judgments in the available cases.
Material and methodDataThis study was conducted from 3 databases:
The first, obtained from expert reports drawn up by the medico-legal doctors of Barcelona during the years 2004–2009. From this, a total of 283 expert reports were obtained which comprised the total sample and from which the main variables studied were extracted. With regard to the claimed-against medical specialties, it should be noted that the claims made in emergency department visits were grouped under “general medicine”, since the specific specialty of emergency medicine does not yet exist.
The second, obtained through access to TEMIS-2, the Justice Department's computer programme, thanks to the authorisation of the Commission for the Organisation and Modernisation of the General Council of the Judiciary. It should be noted that only 161 cases are available in this database, since the Administration of Justice in Catalonia was computerised in 2005.
Finally, thanks to access to the TEMIS-2 programme, it was possible to locate some of the judgments from which the corresponding variables were extracted for analysis.
Statistical methodsA univariate descriptive statistical analysis was performed for each of the variables in the database. For the quantitative variables, the descriptive statistics were calculated: mean, median, standard deviation (SD), minimum and maximum. For the qualitative variables, tables of absolute and relative frequencies were calculated, and the analysis was completed with bar graphs.
A bivariate analysis was carried out to assess the association between some both quantitative and qualitative variables. To analyse the relationship between 2 qualitative variables, contingency tables between the variables were prepared with the corresponding bar charts. The χ2 test or the likelihood ratio was used to determine whether the association was statistically significant, according to the case.
When the quantitative variable “age” was involved in the analyses, the non-parametric Kruskal–Wallis test was used if the covariate had more than 2 categories and the non-parametric Wilcoxon test if the covariate had 2 categories.
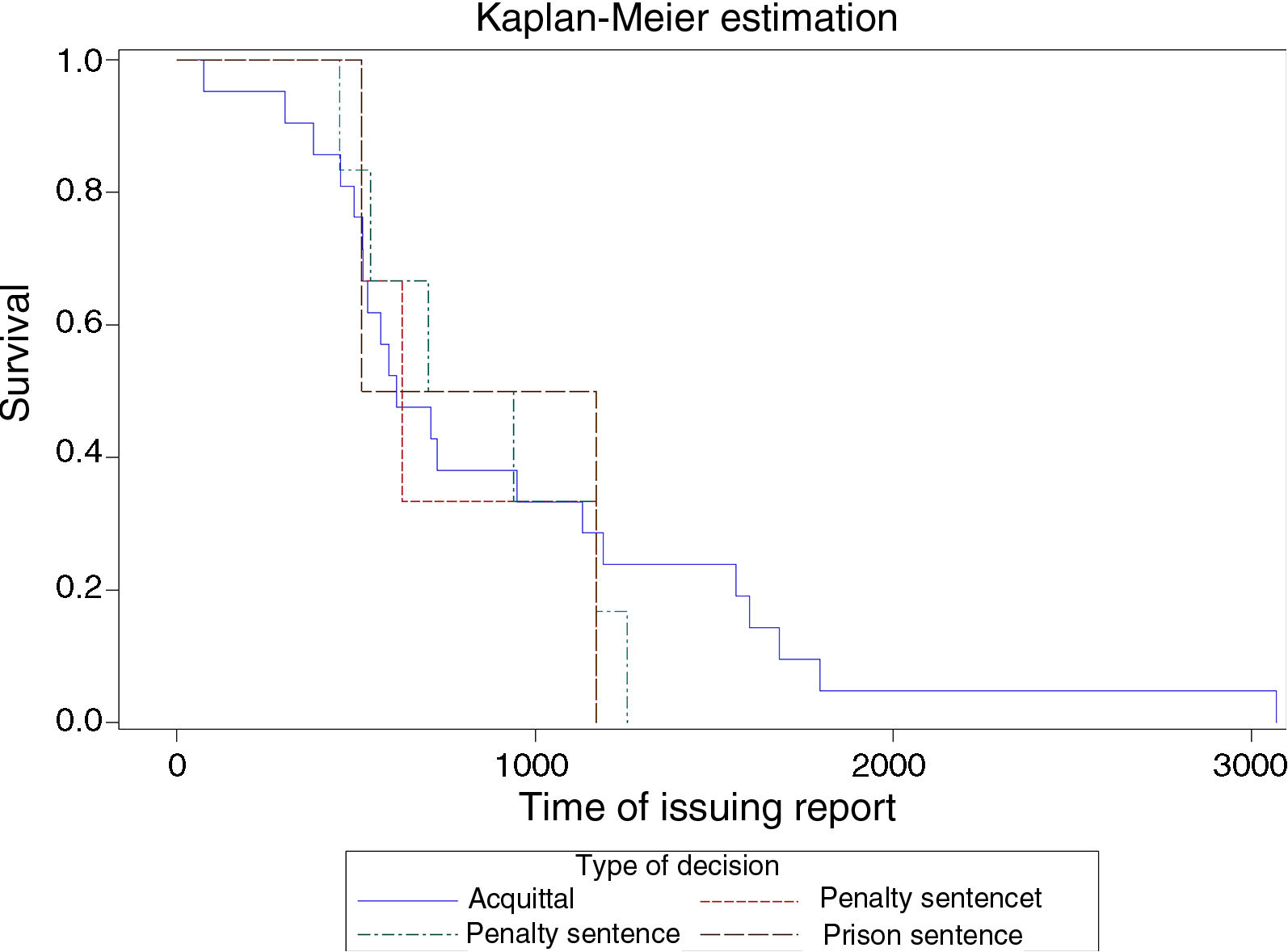
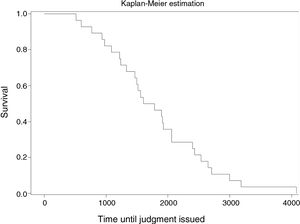
For the variable “time”, a survival analysis was carried out. This area of statistics aims to analyse the time until the occurrence of a well-defined event. In this study the following were calculated:
Time to issue of report=date of the events up until the date of issuing the report
Time until the judgment=date of the events until the date of the judgment
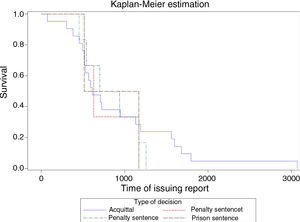
In the analysis of the time until the report was issued, the median in days with its 95% confidence interval (95% CI) was calculated as well as the non-parametric estimate of the survival function using Kaplan–Meier curves. The Log-Rank test was also used to determine whether there were statistically significant differences between the survival curves of the different groups.
All the results were obtained using SAS 9.2 software (SAS Institute Inc, Cary, NC, USA). The significance level was set at .10 or .05 depending on the test.
ResultsAnalysis of general variablesLegal route for initiating the claimIn 257 cases (90.81%), the claim was initiated via the criminal route, of which in 130 (50.58%) the proceedings were initiated through a claim. In 52 cases (20.23%) through a complaint and in 75 cases (29.19%) it was a criminal procedure of which the route of initiation was unknown. The remaining 18 (6.36%) were contentious-administrative proceedings, 5 (1.77%) civil proceedings and 3 (1.06%) Prosecutor's Office claims.
SexOf the 283 cases, in 177 (62.77%) the injured party was a woman. In all the years studied, except 2009, women were the most affected. Likewise, women suffered the most sequelae and more women died due to healthcare complications.
AgeThe ages of the injured parties were a minimum of 0 years (corresponding to a foetus) and a maximum of 90. The mean age was 48.38 years (SD±19.39), in the men 51.92 years (SD±19.7) (0–88 years) and in the women 46.66 years (SD±19) (1–90 years).
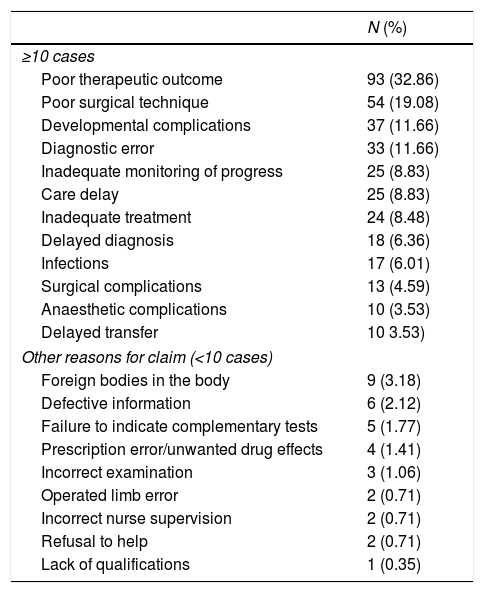
Reason for the claimThe most common claim was made by the patient when there was a poor therapeutic outcome, either because of the existence of sequelae or due to death (Table 1).
Reasons for claim.
| N (%) | |
|---|---|
| ≥10 cases | |
| Poor therapeutic outcome | 93 (32.86) |
| Poor surgical technique | 54 (19.08) |
| Developmental complications | 37 (11.66) |
| Diagnostic error | 33 (11.66) |
| Inadequate monitoring of progress | 25 (8.83) |
| Care delay | 25 (8.83) |
| Inadequate treatment | 24 (8.48) |
| Delayed diagnosis | 18 (6.36) |
| Infections | 17 (6.01) |
| Surgical complications | 13 (4.59) |
| Anaesthetic complications | 10 (3.53) |
| Delayed transfer | 10 3.53) |
| Other reasons for claim (<10 cases) | |
| Foreign bodies in the body | 9 (3.18) |
| Defective information | 6 (2.12) |
| Failure to indicate complementary tests | 5 (1.77) |
| Prescription error/unwanted drug effects | 4 (1.41) |
| Incorrect examination | 3 (1.06) |
| Operated limb error | 2 (0.71) |
| Incorrect nurse supervision | 2 (0.71) |
| Refusal to help | 2 (0.71) |
| Lack of qualifications | 1 (0.35) |
In 250 of the 283 cases (88.34%) the claim was against a doctor, in 5 cases (1.77%) against a nurse and in 12 (4.24%) the claim was brought against both. In 6 (2.12%) the claim was against an administrative officer, in 5 cases (1.77%) against a combination of the former and in 5 (1.77%) unknown.
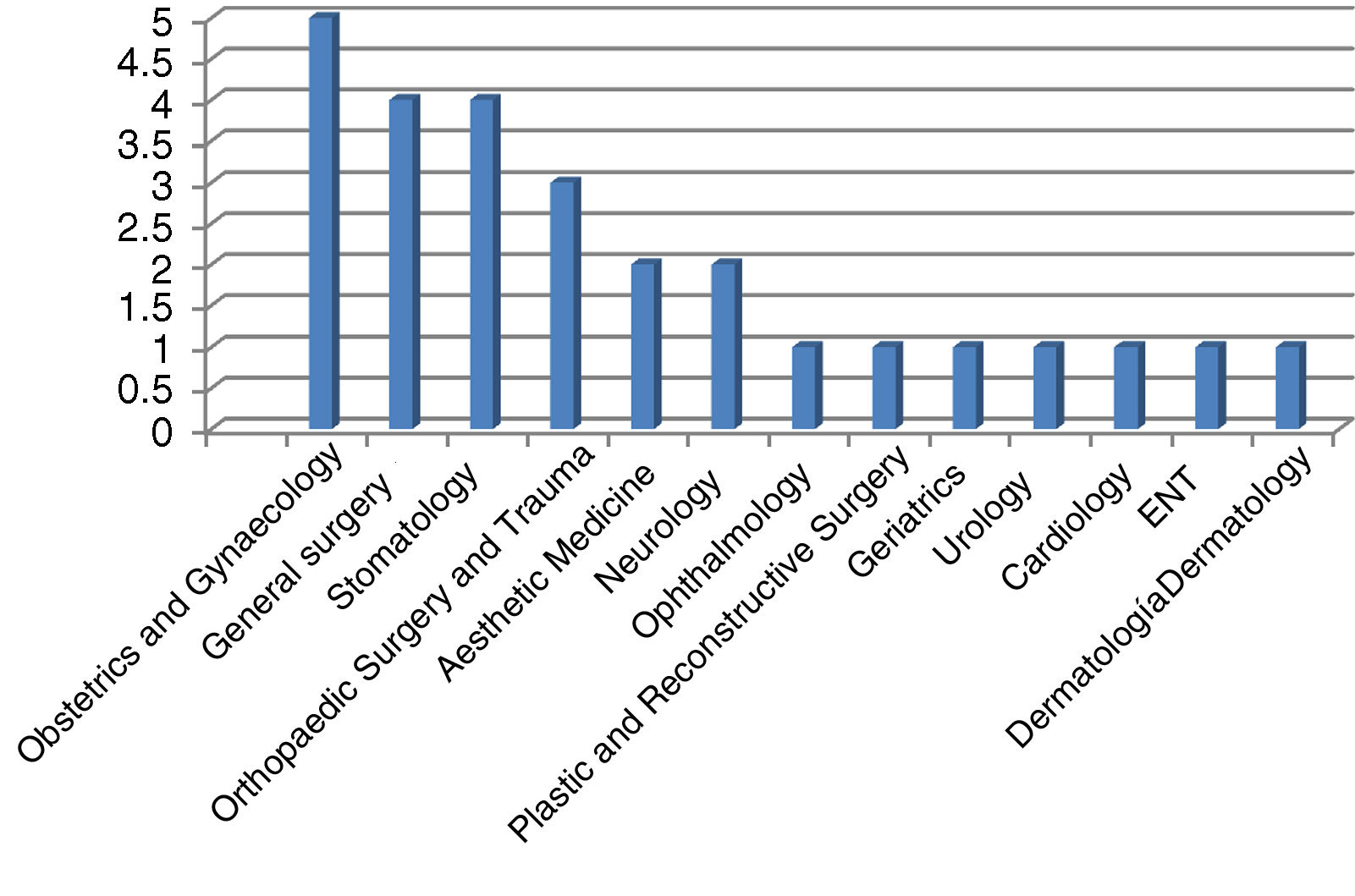
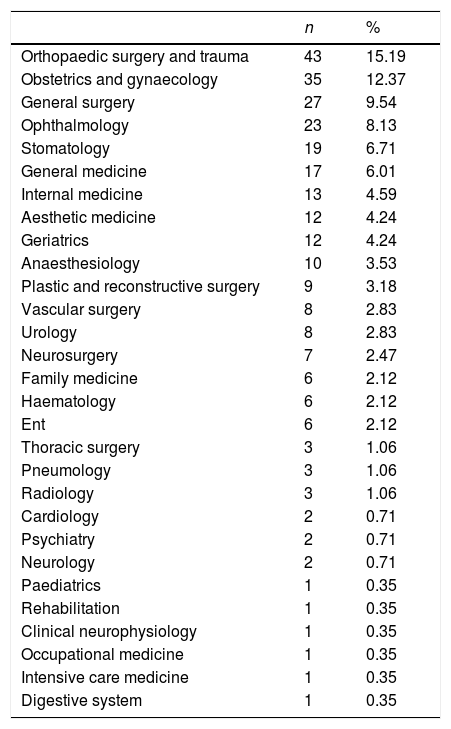
SpecialtyThe 3 most claimed-against specialties were Orthopaedic Surgery and Trauma (OST), Obstetrics and Gynaecology, and General Surgery. The total number of specialties that faced claims does not coincide with the total number of the sample. This is due to the fact that a claim could be directed against several specialties and different professionals (Table 2). In the specialties facing the most claims, it was observed that in OST poor therapeutic outcome was the most frequent reason for the claim. In Obstetrics and Gynaecology, it was the presence of foreign bodies in the body followed by poor monitoring of progress. However, if we assess the specialty of Obstetrics separately from Gynaecology, the most frequent reasons for making a claim would be: foetal death in 8 cases (32%), sequelae in the foetus in 7 cases (28%), maternal sequelae in 3 cases (12%), maternal death in one case (4%), delayed diagnosis in one case (4%) and developmental complications in one case (4%), as the most relevant data. In General Surgery, the most relevant data were developmental complications throughout the care process. By contrast, poor therapeutic outcome was a common reason for making a claim against Ophthalmology, Aesthetic Medicine and Stomatology. In Anaesthesiology, it was anaesthetic complications, whereas in Geriatrics it was poor monitoring of progress, as with Internal Medicine, a specialty where claims were also made for delayed care, diagnostic error and poor outcomes. In the case of Emergency Medicine, claims were for delay in transfer to a healthcare centre.
Claimed-against specialties.
| n | % | |
|---|---|---|
| Orthopaedic surgery and trauma | 43 | 15.19 |
| Obstetrics and gynaecology | 35 | 12.37 |
| General surgery | 27 | 9.54 |
| Ophthalmology | 23 | 8.13 |
| Stomatology | 19 | 6.71 |
| General medicine | 17 | 6.01 |
| Internal medicine | 13 | 4.59 |
| Aesthetic medicine | 12 | 4.24 |
| Geriatrics | 12 | 4.24 |
| Anaesthesiology | 10 | 3.53 |
| Plastic and reconstructive surgery | 9 | 3.18 |
| Vascular surgery | 8 | 2.83 |
| Urology | 8 | 2.83 |
| Neurosurgery | 7 | 2.47 |
| Family medicine | 6 | 2.12 |
| Haematology | 6 | 2.12 |
| Ent | 6 | 2.12 |
| Thoracic surgery | 3 | 1.06 |
| Pneumology | 3 | 1.06 |
| Radiology | 3 | 1.06 |
| Cardiology | 2 | 0.71 |
| Psychiatry | 2 | 0.71 |
| Neurology | 2 | 0.71 |
| Paediatrics | 1 | 0.35 |
| Rehabilitation | 1 | 0.35 |
| Clinical neurophysiology | 1 | 0.35 |
| Occupational medicine | 1 | 0.35 |
| Intensive care medicine | 1 | 0.35 |
| Digestive system | 1 | 0.35 |
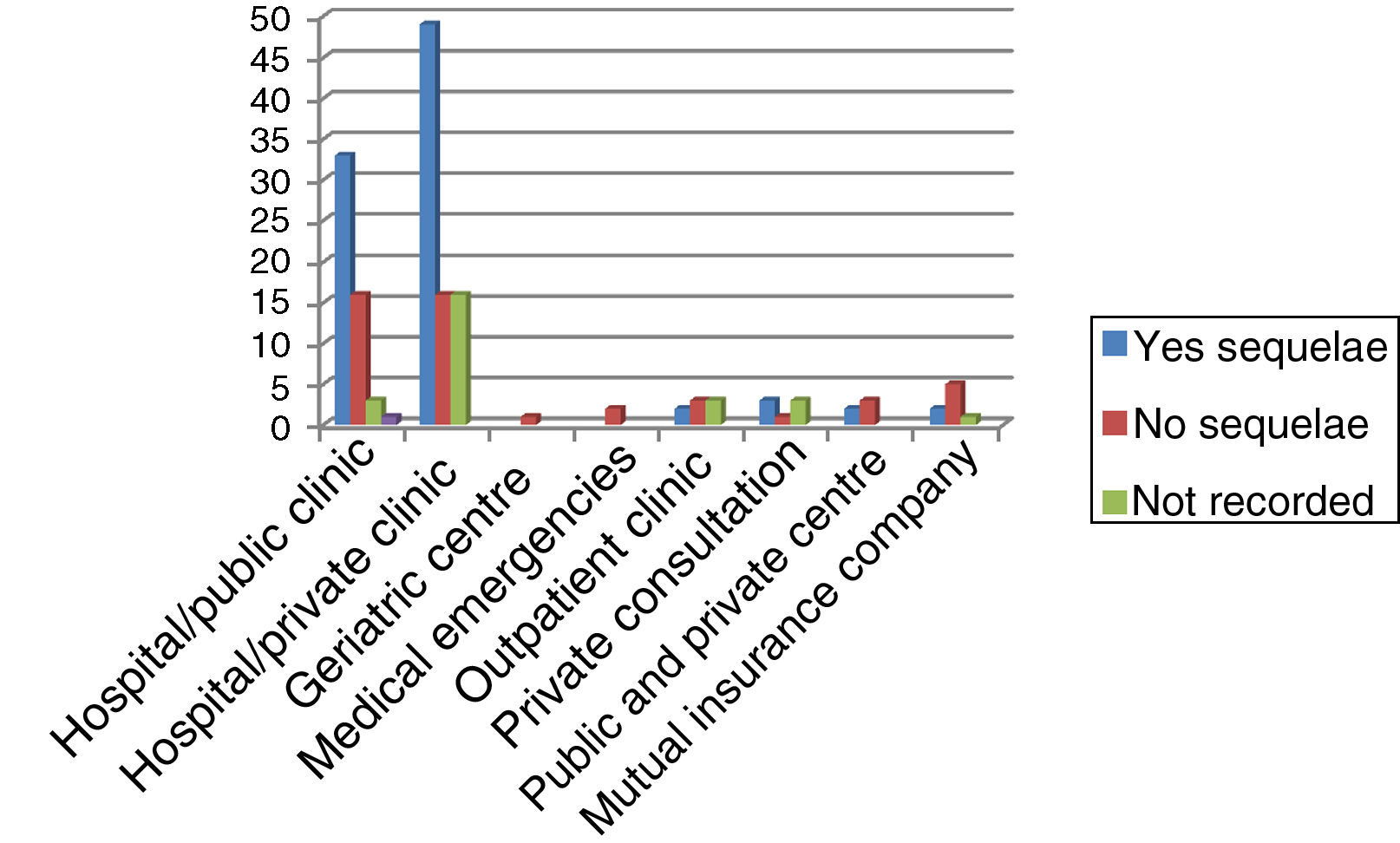
In 114 cases (40.28%), the complaints were directed against private care centres, either hospitals or clinics. In 81 (28.62%), the health centre was a hospital or clinic belonging to the public network. The rest were other centres or medical practices.
Situation of the patient at the time of the events leading to the claimIn 107 cases (37.81%) the patient was an inpatient in the care centre. In 54 (19.08%) the event occurred after the patient had been discharged from hospital and in 54 cases (19.08%) during outpatient follow-up. In 29 (10.25%) the patient was in the emergency department and in 18 cases (6.36%) at home. In 9 (3.18%) their disease had persistently progressed, and they had had multiple hospital admissions. In 8 cases (2.83%) the complication was secondary to outpatient surgery. Three corresponded to other circumstances (1.06%) and in one case, it was unknown (.35%).
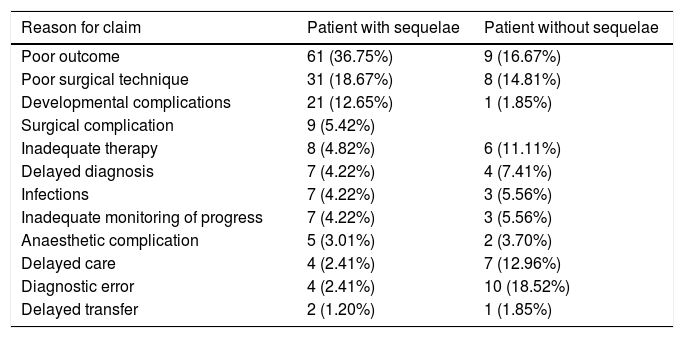
Patient with sequelae and most frequent reason for making a claimWhen the patient had sequelae, the most common reason for making a claim was poor outcome (36.75%). If there were no sequelae, it was diagnostic error (18.52%). There were more reasons for claims than the number of patients, since the same patient could have more than one reason for making a claim (Table 3).
Most frequent reason for a claim by patients with or without sequelae.a
| Reason for claim | Patient with sequelae | Patient without sequelae |
|---|---|---|
| Poor outcome | 61 (36.75%) | 9 (16.67%) |
| Poor surgical technique | 31 (18.67%) | 8 (14.81%) |
| Developmental complications | 21 (12.65%) | 1 (1.85%) |
| Surgical complication | 9 (5.42%) | |
| Inadequate therapy | 8 (4.82%) | 6 (11.11%) |
| Delayed diagnosis | 7 (4.22%) | 4 (7.41%) |
| Infections | 7 (4.22%) | 3 (5.56%) |
| Inadequate monitoring of progress | 7 (4.22%) | 3 (5.56%) |
| Anaesthetic complication | 5 (3.01%) | 2 (3.70%) |
| Delayed care | 4 (2.41%) | 7 (12.96%) |
| Diagnostic error | 4 (2.41%) | 10 (18.52%) |
| Delayed transfer | 2 (1.20%) | 1 (1.85%) |
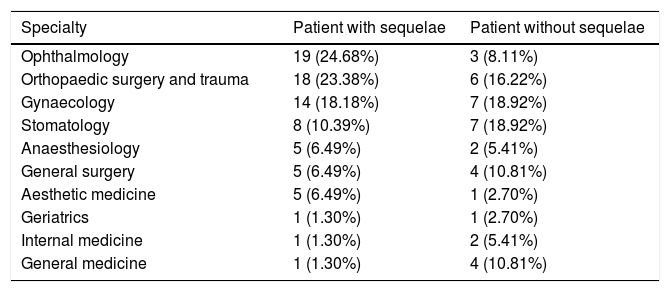
Among the most claimed-against specialties (that is, with more than 10 claims), those facing most claims due to sequelae were: ophthalmology (24.68%), OST (23.38%) and gynaecology (18.18%) (Table 4).
Medical specialties with most sequelae.a
| Specialty | Patient with sequelae | Patient without sequelae |
|---|---|---|
| Ophthalmology | 19 (24.68%) | 3 (8.11%) |
| Orthopaedic surgery and trauma | 18 (23.38%) | 6 (16.22%) |
| Gynaecology | 14 (18.18%) | 7 (18.92%) |
| Stomatology | 8 (10.39%) | 7 (18.92%) |
| Anaesthesiology | 5 (6.49%) | 2 (5.41%) |
| General surgery | 5 (6.49%) | 4 (10.81%) |
| Aesthetic medicine | 5 (6.49%) | 1 (2.70%) |
| Geriatrics | 1 (1.30%) | 1 (2.70%) |
| Internal medicine | 1 (1.30%) | 2 (5.41%) |
| General medicine | 1 (1.30%) | 4 (10.81%) |
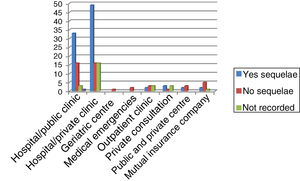
There were more claims from patients with sequelae in the private centres (Fig. 1).
Deceased patientsOf the sample studied, the patient died in 91 cases (32.16%).
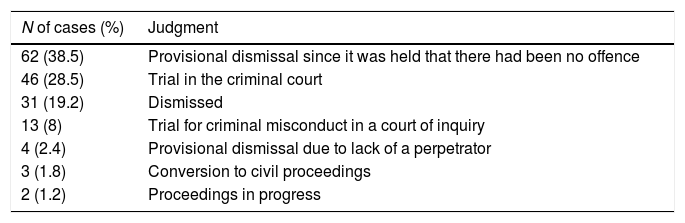
Analysis of the outcomes of legal proceedingsTable 5 shows the outcomes of the 161 cases that were located through the legal computer programme TEMIS-2.
Development of the legal proceedings.
| N of cases (%) | Judgment |
|---|---|
| 62 (38.5) | Provisional dismissal since it was held that there had been no offence |
| 46 (28.5) | Trial in the criminal court |
| 31 (19.2) | Dismissed |
| 13 (8) | Trial for criminal misconduct in a court of inquiry |
| 4 (2.4) | Provisional dismissal due to lack of a perpetrator |
| 3 (1.8) | Conversion to civil proceedings |
| 2 (1.2) | Proceedings in progress |
In 48.28% of the cases where the patient had sequelae, the proceedings were transferred to a criminal court for oral proceedings. When the patient had no sequelae, only 25% of the cases were tried in the criminal court.
Deceased patient and outcome of court proceedings according to the TEMIS-2 computer programmeIn 19.78% of cases where the patient had died, the court proceedings were dismissed since it was held that there had been no offence, while in 17.58% the investigation continued until oral proceedings were held in the criminal court. In 8.79% the proceedings were dismissed, in 3.30% proceedings for a misdemeanour were held in the courts of inquiry. At the time of the study 2.20% were in progress. The remaining cases were either dismissed due to lack of a perpetrator, or the situation was not known.
General analysis of the variables obtained from the judgmentsA total of 29 judgments were obtained of which the following most relevant variables were assessed.
SpecialtyThe most claimed-against medical specialty that most frequently came to trial was Obstetrics and Gynaecology (17.24%), followed by General Surgery and Stomatology (both at 13.79%) (Fig. 2).
Classification by the public prosecutor's officeIn 17 cases the position of the public prosecutor's office was to charge (58.62%), in 10 it did not charge (34.48%) and the charge was withdrawn in 2 cases during the trial (6.90%).
Assessment of the medico-legal doctor's expert actionIn 55.55% of cases, the judges assessed the quality of the medico-legal doctor's intervention positively, considering the values of objectivity and impartiality brought by public service. In 6 cases (16.67%) no reference was made in the judgment to the quality of the expert witness. In 3 cases (8.33%) the performance of the medico-legal doctor was not well assessed. In 7 cases (19.44%), there was no medico-legal expert.
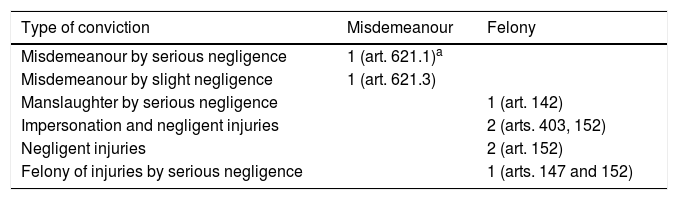
Judgment and type of criminal convictionIn 21 cases (72.41%) the judgment was acquittal and in 8 (27.59%), conviction. This case includes a sentence as sought by the prosecution. The articles of the Penal Code applied in the case of conviction are shown in Table 6.
Type of conviction in 8 cases.
| Type of conviction | Misdemeanour | Felony |
|---|---|---|
| Misdemeanour by serious negligence | 1 (art. 621.1)a | |
| Misdemeanour by slight negligence | 1 (art. 621.3) | |
| Manslaughter by serious negligence | 1 (art. 142) | |
| Impersonation and negligent injuries | 2 (arts. 403, 152) | |
| Negligent injuries | 2 (art. 152) | |
| Felony of injuries by serious negligence | 1 (arts. 147 and 152) |
In the cases where there was a conviction, this consisted of: 5 cases of a penalty (29.41%), 2 cases of professional disqualification (11.76%) and only one case of prison sentence (5.88%).
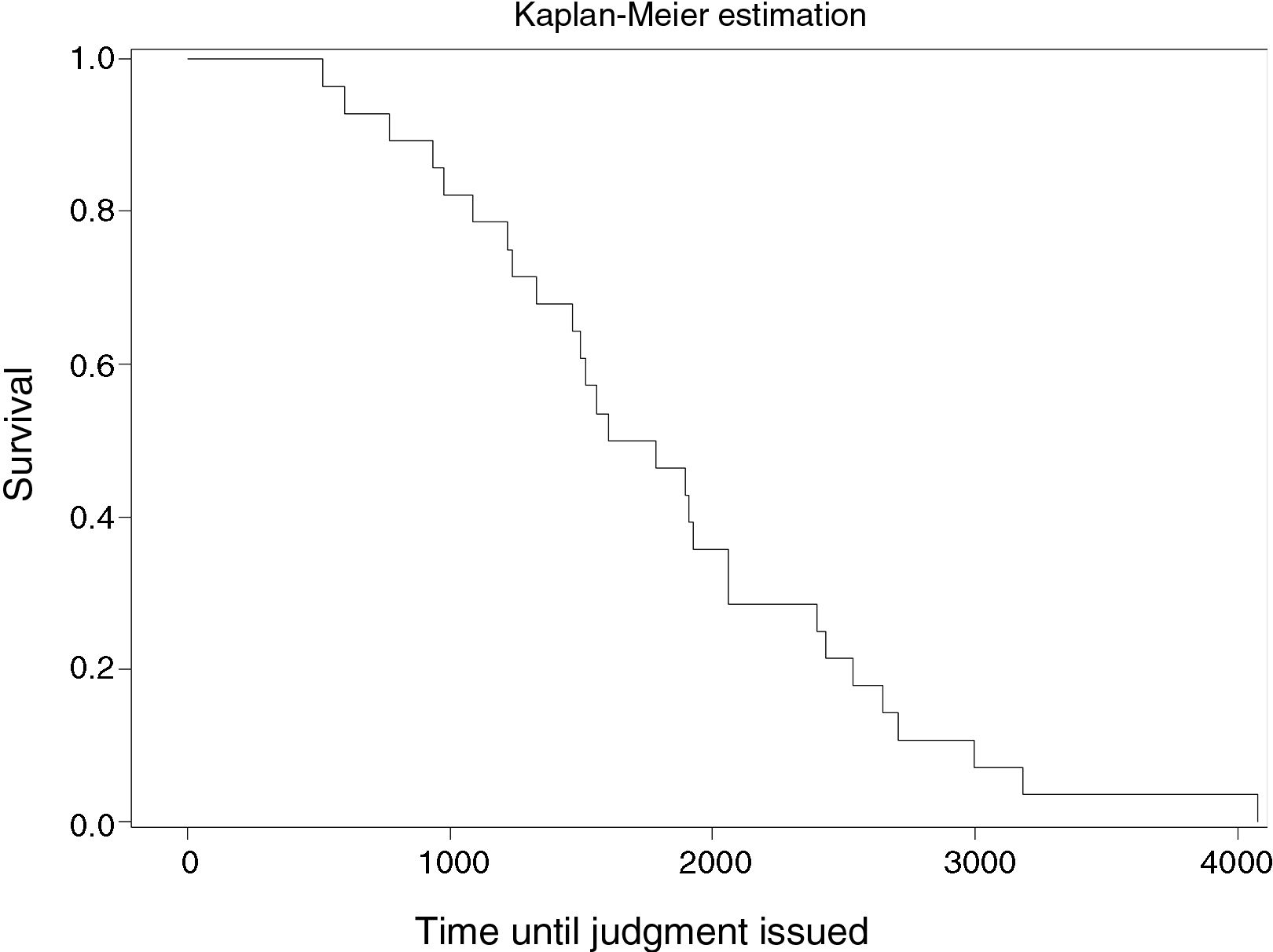
Duration of the legal proceedingsIn the sample of the 29 sentences obtained, the time was evaluated from the date of the events until judgment was issued: the median time until the judgment was 1602 days (95%CI=1329–2061) (Fig. 3).
Time from issuing the medico-legal report until the judgmentThe estimated median of the time from issuing the medico-legal report in the case of acquittal was 614 days with a CI95%=519–1132; in the case of a disqualification order, the estimated median was 630 with a 95%CI=516–1171; for a penalty conviction, the estimated median was 821 days with 95%CI=454–1257 and for a prison conviction, the estimated median of the time was 843.5 days, with a 95%CI=516–1171 (Fig. 4).
DiscussionThe results show that in our study, criminal prosecution is the most common way to initiate a claim for alleged malpractice (89.05% of cases). This data coincides with the work published by authors such as Rodríguez Hornillo et al.12 or Pujol Robinat and Puig Bausili.13 However, in our case this result could be partially biased since the database was made up of medico-legal experts and the intervention of the medico-legal doctor is more frequently initiated through the courts of inquiry.
In contrast, according to the report published by the Professional Liability Service of the Barcelona Medical Association (which includes both judicial and extra-judicial complaints) for 2016, the number of complaints for possible malpractice decreased by 3%, and extra-judicial complaints at 60% continue to be the most frequent type of complaint. This continues a trend that began in 2008 of a decrease in litigation, especially claims.14
Our study shows that although the most frequent route to initiate a legal claim in the area of medical liability is criminal, a study of the judgments analysed shows that 72.41% of these were acquittals, and therefore we believe that other alternatives to the criminal justice system should be sought to manage medical liability and, where necessary, to make good the damage caused without court intervention. These data coincide with those of the Professional Liability Service of the Barcelona Medical Association, where it is recorded that during 2016, 89% of criminal cases were resolved with dismissal or acquittal, and convictions arising from civil proceedings only represented 29%.14
Engel and Livingston report that the statistics show that a conviction for malpractice is rare, with a prevalence of 1%, and therefore they propose modifying the legal system to reduce costs and reduce defensive medicine.15
We note that most complaints are made by people in the age range 44–56 years. This could be because socially this age range is considered to be when a stage of maturity and even physical and occupational fulfilment has been reached and, therefore, neither disabilities nor death are as accepted as they are in the advanced stages of life. At younger ages, it is possible that the demand for care is not as frequent or that survival is higher. Most of the authors consulted, such as Somville et al. and Hammami et al.16,17 coincide in these data.
With regard to the sex of the claimants, women are most affected and this coincides with Madea et al.18, Hernández Gil2 and Studdert et al.19 Perhaps this could be explained by the fact that women may require more medical visits throughout their lives or because when they request care they are in a worse state of health and the consequences are also worse.
A relevant aspect is to establish the reason for the patient's claim. Knowing about the user's complaint is a fundamental element to be able to correct possible care dysfunctions, practice preventive legal medicine, and above all, improve patient safety.
In our series, the most frequent reason for making a claim was poor therapeutic outcome (32.86%); followed by poor surgical technique (19.08%); thirdly, developmental complications during the care process (13.7%); and fourthly, diagnostic error (11.66%). Sanz Martín and Sanz Hospital coincide in these data.20
The surgical specialties (66.78%) face more complaints than the medical specialties (30.04%), this data coincides with that of other authors.21,22
The most controversial specialties are (from the most to the least): Orthopaedic Surgery and Trauma, Obstetrics and Gynaecology, General Surgery and Ophthalmology. Internal Medicine is in seventh place. These data coincide with those published by Anupam et al.21 This could be explained by the fact that, in general, surgical specialties perform more aggressive and complex procedures than medical specialities, and therefore there may be a greater risk of complications, sequelae and death of the patient. This would be confirmed in our case by the fact that the surgical specialties (87%) had a higher percentage of sequelae than the medical specialties (20%). By contrast, the percentage of deaths was the same in the medical and the surgical specialties. Nunno et al. conducted a study on a sample of 364 cases and established a proportion of claimed-against surgical specialties of 52% versus 41% of medical specialties.22
When analysing the different specialties, diagnostic error and delay, and failure to monitor progress are the most common reasons for claims made against medical specialties. While anaesthetic complication, poor outcome and developmental complications affect the surgical specialties more.
In the United States there is the “hospitalist” model, which already exists in Spain (Navarra, Madrid, etc.) and is characterised by teamwork and interdisciplinary cooperation of both physicians and nurses: the “hospitalist” physician acts as coordinator of the healthcare process, and is a specialist in internal medicine, and the physician of the corresponding specialty, with the support of specialist nursing staff, a pharmacist, a radiologist and a clinical microbiologist.23 The “hospitalist” doctor acts as coordinator of the care process. This multidisciplinary model means improved patient care, greater protection, and in fact, studies corroborate that a reduction in mortality of 11% has been observed. At the same time, it improves the training of resident doctors.23 The article published by Somville et al. and that of Arimany-Manso and Martín-Fumadó agree that communication and collaboration between professionals can reduce technical errors during the care process, especially in surgical patients or those with high comorbidity.16,24
In our series we observed that private healthcare (clinics or hospitals) faces more claims for possible malpractice than public centres. This does not coincide with the article published by Alvarez González et al.,25 where there is some balance between complaints faced by public and private health care.
With respect to the situation of the patient at the time the complaint is made, in 37.81% of cases the patient is an inpatient. This data coincides with the work of Martínez Mondéjar et al. (87% of cases of adverse effects in the patient occur during hospitalisation). In second place are the complications following discharge from hospital, thirdly those during follow-up and finally those in the emergency department.6
According to Hernández Gil and Tudela et al., the care areas that generate most conflict are, in this order: the emergency department, the operating theatre, outpatients, the hospital wards and finally the delivery room.2,26
By contrast, Madea and Preub, in their paper on a series of patients who died during the care process, consider that the greatest number of claims occur during hospital admission, in the emergency departments in second place, and third place against physicians from private care centres,27 coinciding with Cohen and Hughes.28
Of the 283 cases in the sample, in 207 (73.14%) the medico-legal doctor concluded that there was no professional liability. When the patient had sequelae, the expert evaluation concluded that in 70% of the cases the practice was correct. Even when the patient had died, the expert assessment concluded in 71.43% of cases that there had been no malpractice. These data reflect the current situation with regard to allegations of malpractice. A criminal claim in the face of a poor outcome would not be the most appropriate course of action.
A judicial follow-up of the files shows that 16.25% of the cases went through criminal summary proceedings and 4.59% were maintained as misdemeanour trials. The court rulings obtained confirm that the surgical specialties are more conflictive than the medical, obstetrics and gynaecology in particular. Likewise, there are more judgments coming from the private healthcare sector than from the public sector.
It is important to note that the assessment of medical care practice by the medico-legal doctor coincides with the results of the judgments, since in the cases in which the medico-legal doctor concluded that there was no malpractice, 100% of the judgments were acquittals.
In the analysis of the time taken to resolve legal proceedings of this nature, there is an average of 4.38 years from the date of the events constituting the claim to issuance of the judgment.
Therefore, a new perspective is required in the analysis of medical liability, in relation to the health and hospital management as well as the legal and expert management of claims.
Current strategies focus on improving patient safety at the healthcare level and on the out-of-court management of claims. We must admit that error is inherent to professional activity. Adverse events that may cause the patient harm can be detected and prevented. The correct management of error allows us to improve patient safety and quality of care, as well as to reduce the social and health costs involved.11,29,30 The concept of professional liability is now closely linked to that of clinical safety.24
Transparency must be the driving force behind new strategies in patient safety: identify the error and learn. In the United States a new strategy for medical error has been implemented, which was proposed and promoted by Barack Obama and Hillary Clinton: “National Medical Error Disclosure and Compensation”. The aim of the programme is to strengthen communication between doctors and patients affected by an adverse event.31,32 According to the authors, acceptance of the error has led to fewer malpractice lawsuits and a reduction in administrative, legal and health costs.
The legal approach, especially the criminal approach to medical liability, must change. The results show that these conflicts are not best resolved through criminal law.
Firstly, it is slow. It is a cold route, without discretion or reserve and not very elastic according to Hernández Moreno et al.33 Legal action can be emotionally traumatic for both the patient and their family.4 It also involves the increase in defensive medicine which implies more health and social costs. This is indicated by authors such as Studdert et al. or Wong et al.34,35 Likewise, according to Arimany-Manso et al., after legal proceedings some professionals develop the so-called “clinical-judicial syndrome” with anxiety, isolation, loss of self-esteem and great emotional impact.36 These reflections have led many authors to start considering the out-of-court route and arbitration courts as the best option for resolving these conflicts, with a fairer compensation system.17,19,37,38
This paper has limitations: loss of sample. Our analysis was based on the data contained in the expert reports issued by the medico-legal doctors of Barcelona during the years 2004–2009. The final sample does not correspond to all the files processed, since as this is a retrospective study some of the cases dealt with are missing.
Difficulty in accessing data from the Department of Justice. It was only possible to obtain a total of 29 judgments for the 283 cases contained in the sample. It is difficult to follow up on legal proceedings. On the one hand, because not all the data are recorded in the computer programme, and on the other, because the continuous changes in numbering of the proceedings make them difficult to trace.
The long duration of the legal proceedings means that many of the judgments made at the time of the study were not final and therefore it is very difficult to establish the definitive result of the proceedings analysed.
We conclude therefore that the criminal route is taken most frequently to initiate a claim for alleged malpractice. Women claim more and suffer more sequelae as a consequence of a healthcare procedure. Claims affect surgical specialties more than medical specialties. More complaints are made in the field of private health care than in public health care. Most claims are made due to complications during hospitalisation. In the criminal area, only 27.59% of the cases that came to trial resulted in convictions, and only in one case was there a prison sentence.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all our fellow medico-legal doctors in Barcelona for their collaboration and facilities in carrying out this study. We would also like to thank the Organisation and Modernisation Commission of the General Council of the Judiciary for facilitating access to the Justice Department's computer programme. Finally, our thanks to the management of the Institute of Legal Medicine and Forensic Sciences of Catalonia who provided technical support and facilitated the completion of this paper.
Please cite this article as: Giménez Pérez D, Pujol-Robinat A, Castellá García J, Espinal Berenguer A, Vázquez Fariñas A, Medallo Muñiz J. Denuncias por responsabilidad profesional médica en Barcelona (2004-2009). Análisis médico-forense. Rev Esp Med Legal. 2020;46:56–65.