The traumatic injuries in Chile are the third cause of death in the general population and the first in young people. Their epidemiology varies around the world, and is linked to demographic and sociocultural differences, with few studies in Latin America.
ObjectiveTo determine epidemiological profile of the jaw bone fractures in the Traumatology Institute (IT) of Santiago, Chile.
Material and methodRetrospective descriptive and quantitative study was conducted in the Maxillofacial Surgery Department of the IT, developed by recording data from a review of clinical records of patients with surgically treated jaw fractures. Data were collected between January-2001 and December-2010 using Microsoft Access 2007© and then tabulated and plotted using Microsoft Excel 2007©.
ResultsOut of a total of 783 facial fractures, 240 clinical files of surgically treated jaw fractures were available for analysis. The male:female ratio was 5.9:1, and the most affected age group was between 20 and 29 years old. The most frequent cause of the fracture was aggressions. Most patients were treated in an average of 8.6 days from admission. In conclusion, these results are consistent with the literature, except for the associations between the affected anatomical site and aetiology.
Los traumatismos en Chile son la tercera causa de muerte en la población general y la primera entre jóvenes. Se ha reportado una epidemiología variable alrededor del mundo asociada a diferencias demográficas y socioculturales, con escasos estudios en Latinoamérica.
ObjetivoConocer la epidemiología de las fracturas mandibulares en el Instituto Traumatológico de Santiago, Chile.
Material y métodoEstudio retrospectivo descriptivo de tipo cuantitativo en el Servicio de Cirugía Maxilofacial del IT, consistente en la recolección de datos mediante revisión de fichas clínicas de pacientes operados por fracturas mandibulares entre enero de 2001 y diciembre de 2010. Los datos fueron recopilados utilizando una base de datos Microsoft Access 2007 y luego tabulados y graficados con Microsoft Excel 2007.
ResultadosDe un universo de 783 fracturas faciales, 240 fichas de fracturas mandibulares operadas estuvieron disponibles para su análisis. La proporción hombres:mujeres fue de 5,9:1 y el grupo etario más afectado fue aquel entre 20 y 29 años. Las agresiones por terceros fueron su causa más frecuente. La mayoría de los pacientes fueron tratados en un promedio de 8,6 días desde su ingreso. En conclusión, estos resultados en general son concordantes con la literatura, salvo asociaciones entre sitio anatómico afectado y etiología.
In Chile, traumas are the third cause of death in the general population, ascending to the first place in the case of young people.1
In the last years, due to the magnitude and exposed position of the head, associated also with several sociocultural factors, there has been an increase in the prevalence and complexity of facial traumas,2,3 being their most common aetiology traffic accidents, aggressions by third parties, sport and work-related accidents and falls.4 The jaw, in particular, in spite of being the heaviest and strongest bone in the face, due to its shape and position is the common spot for maxillofacial fractures, which are not unperceived due to its mobility and the variety of functions in which it is involved.5
The importance of maxillofacial traumas lies mainly in its consequences, since they are associated with a great morbidity, loss of function, aesthetic sequelae and high financial costs, since most of the patients require hospitalisation and the use of resources that impose a great burden on the healthcare system,6,7 as well as a loss for the economy in terms of the days of work missed by those affected.3 Moreover, facial traumas are many times associated with concomitant injuries in other parts of the body, like injuries in the spine, brain, abdomen, thorax and limbs.3,7 Specifically, traumatic lesions in the jaw are associated with the production of temporomandibular articulation disorders, malocclusion, chewing alterations, salivary disorders, obstructive sleep apnoea and chronic pain.2
Several studies carried out worldwide have reported the epidemiology of maxillofacial traumas in their respective populations, accounting for their variability in regards to the environment, geographic area, researched period and sociocultural aspects.3,8 However, there are few reports on this subject in South America.2,6 The objective of this study is to become acquainted with the epidemiology of mandibular fractures surgically treated at the Instituto Traumatológico de Santiago de Chile between the years 2001 and 2010.
Material and methodsA descriptive, cross-sectional study was carried out in the Maxillofacial Trauma and Surgery Service of the Instituto Traumatológico Dr. Teodoro Gebauer Weisser, in Santiago de Chile, between the years 2001 and 2010. Data collection was performed by reviewing the records from the Central Pavilion of the Instituto Traumatológico and further extracting data via clinical file cards, with prior authorisation from the institution management. For this last step, a Microsoft Access 2007® database, especially designed to record maxillofacial interventions, was used.
The study was carried out with the universe of population constituted by all the patients with mandibular fractures who were operated under general anaesthesia by the Maxillofacial Surgery Team at the central pavilion of the Instituto Traumatológico, from January 2001 to December 2010. Patients with diagnoses different from traumatic fractures, treated by non-surgical means, operated for surgical sterilisation purposes or for correction of previous trauma sequelae, and patients whose records were lost, incomplete or illegible were excluded. Thus, the final number of patients included was 240, out of a total of 353 mandibular fractures.
The data extracted from the clinical file card included the patient's gender, age, date of admission to the hospital, and surgical intervention date, aetiology, anatomical site and side of the fracture. Data were finally collected on a Microsoft Excel 2007® spreadsheet, using, for data analysis, statistics such as average and range for the quantitative variables, and absolute and relative frequencies for the qualitative variables.
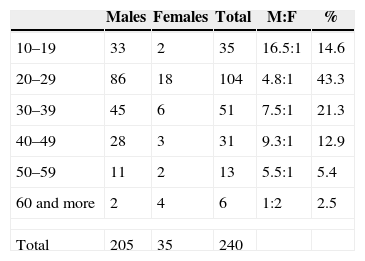
ResultsIn this study, the average age of the patients was 30.3 years, being the most compromised age range the one from 20 to 29 years. In regards to the sex variable, 85.4% of the patients were of the male sex, while 14.6% were of the female sex, thus generating an approximate ratio of 6:1. In almost all age groups, the male predominance is maintained, being the greatest difference between 10 and 19 years, where the proportion of men in respect to women reached 16.5:1; and, on the contrary, in the oldest age range (60 years and more) the ratio is inverted, being women doubly affected in comparison with men (Table 1).
Distribution of patients affected by mandibular fracture sorted by age range and gender between 2001 and 2010.
| Males | Females | Total | M:F | % | |
|---|---|---|---|---|---|
| 10–19 | 33 | 2 | 35 | 16.5:1 | 14.6 |
| 20–29 | 86 | 18 | 104 | 4.8:1 | 43.3 |
| 30–39 | 45 | 6 | 51 | 7.5:1 | 21.3 |
| 40–49 | 28 | 3 | 31 | 9.3:1 | 12.9 |
| 50–59 | 11 | 2 | 13 | 5.5:1 | 5.4 |
| 60 and more | 2 | 4 | 6 | 1:2 | 2.5 |
| Total | 205 | 35 | 240 | ||
M:F: ratio males:females.
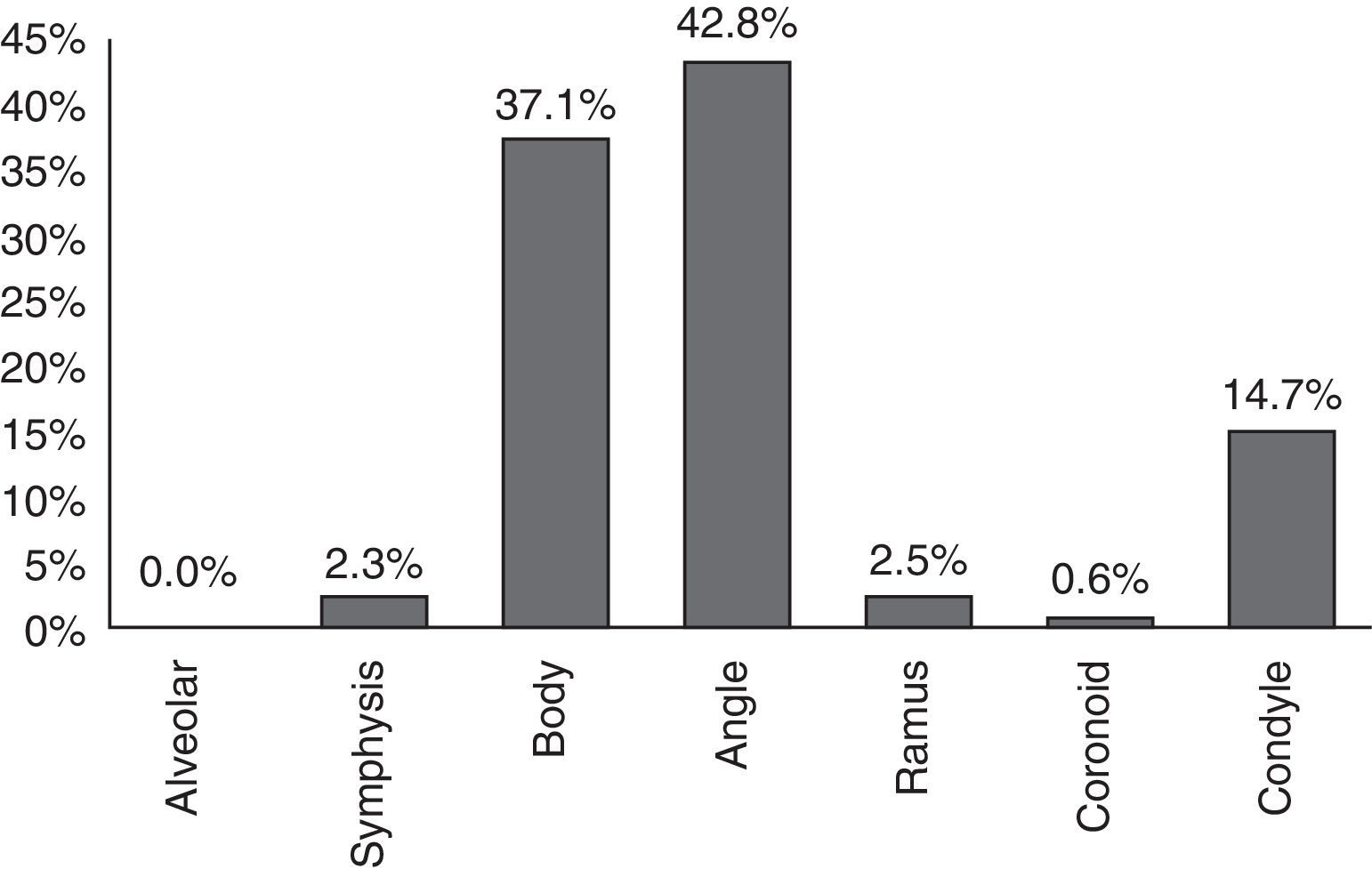
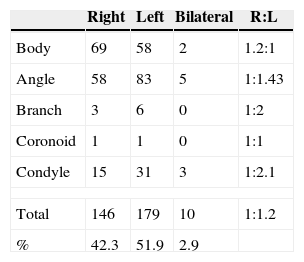
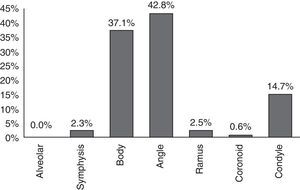
Out of the total (353) of mandibular fractures surgically intervened between the years 2001 and 2010, the most frequently compromised anatomical site (42.8%) was the mandibular angle, followed by mandibular body fractures (37.1%) and the mandibular condyle (14.7%) (Fig. 1). In regards to the side of the jaw affected, in this sample, the left side was slightly more affected than the right one, with 51.9% of the fractures versus 42.3% on the right side, the left side being 1.2 times more affected (Table 2).
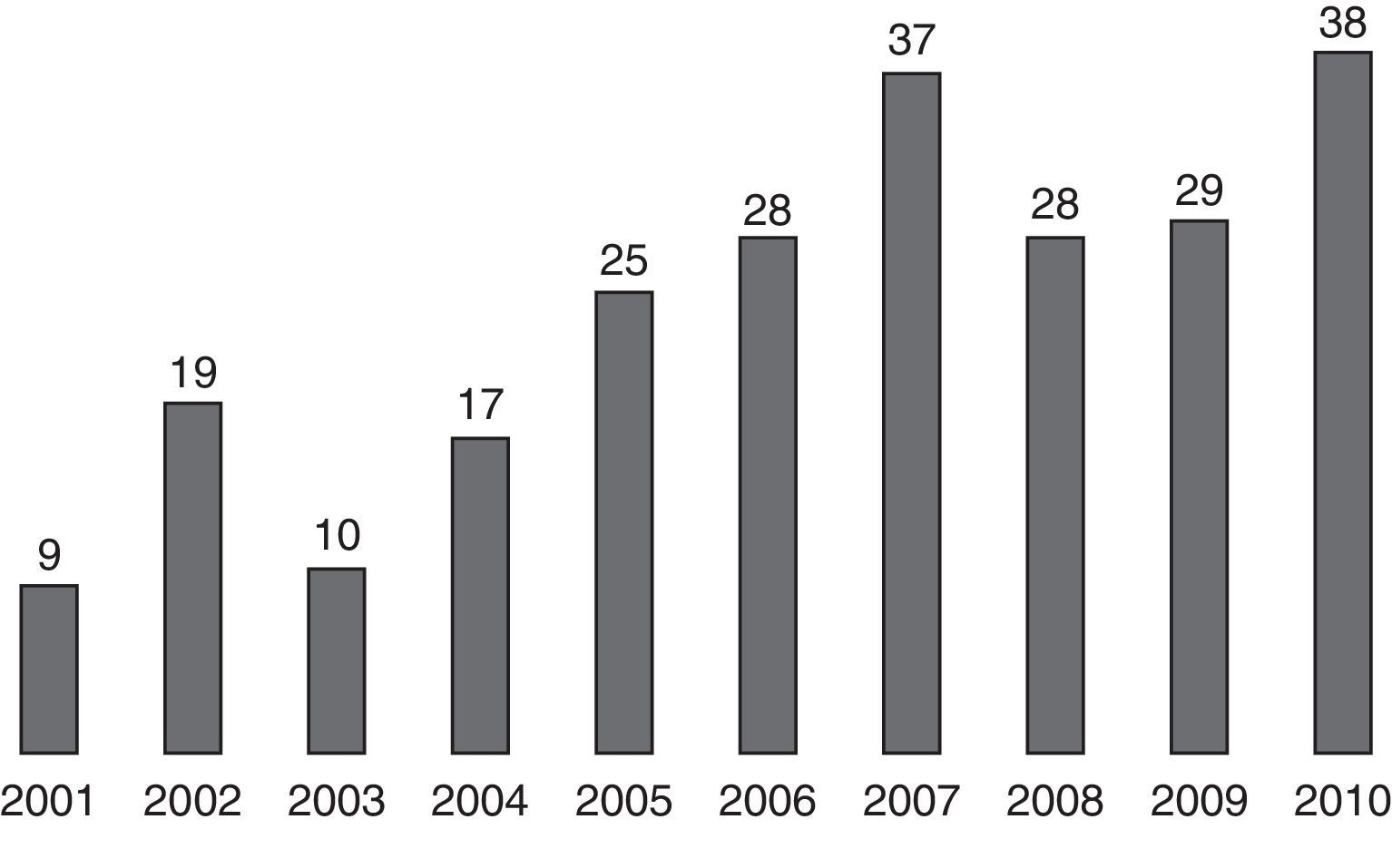
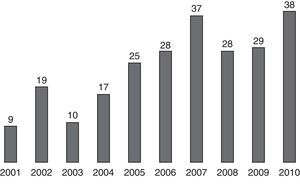
Within the 10 years included in this study, 2010 was the year in which the highest number of surgical reductions of mandibular fractures was performed. In the period comprised between 2001 and 2004, the number of surgeries did not exceed 20, whereas between 2005 and 2010, the number was maintained within a range between 25 and 38, with an average of 30 surgeries per year (Fig. 2).
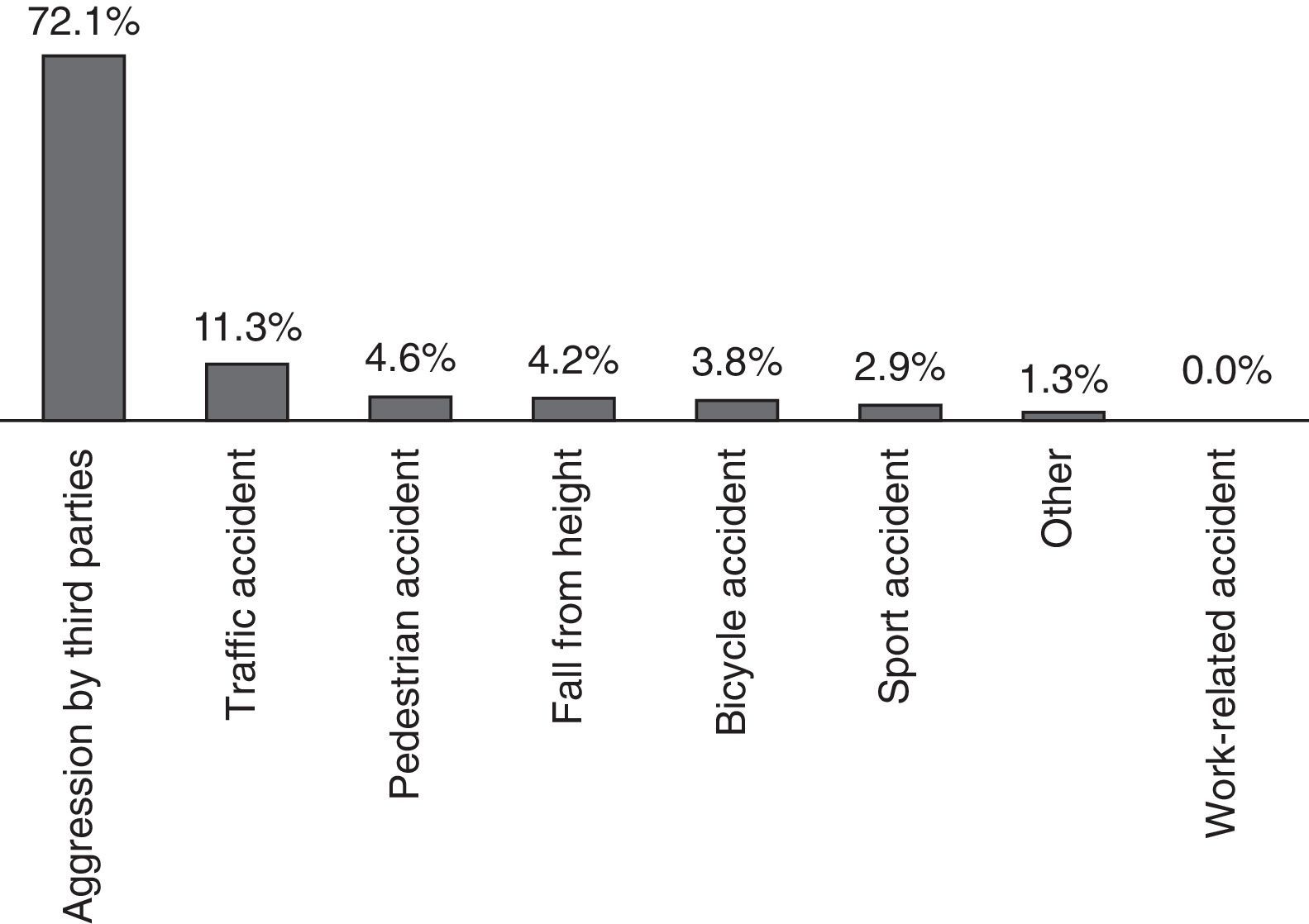
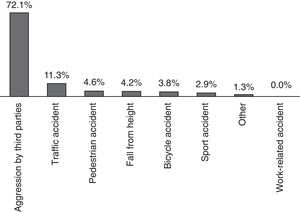
In regards to the causes of mandibular fractures in this study, the main aetiology corresponded to aggressions by third parties (72.1%), followed by traffic accidents (11.3%), which do not include bicycle accidents (3.8%). The rest of the fractures were caused by falls, sport accidents and other causes, none of which exceeded 4.6% of the fractures intervened in the studied period (Fig. 3). Now, if we also take into account the gender within this variable, the male sex exceeds the female in all the aetiologies, except for pedestrian accidents (or falls to same level), whereas in the case of sport accidents, women are not affected by them in this sample, and in the aggressions by third parties, they showed a ratio of men respect to women of 9.2:1. In regards to the relation between aetiology and age range, a predominance of aggressions by third parties was found in all age ranges, except for people over 60 years of age, where pedestrian accidents prevailed. Lastly, aggressions by third parties constitute the main cause of all types of fractures found in this study, expect for coronoid fractures.
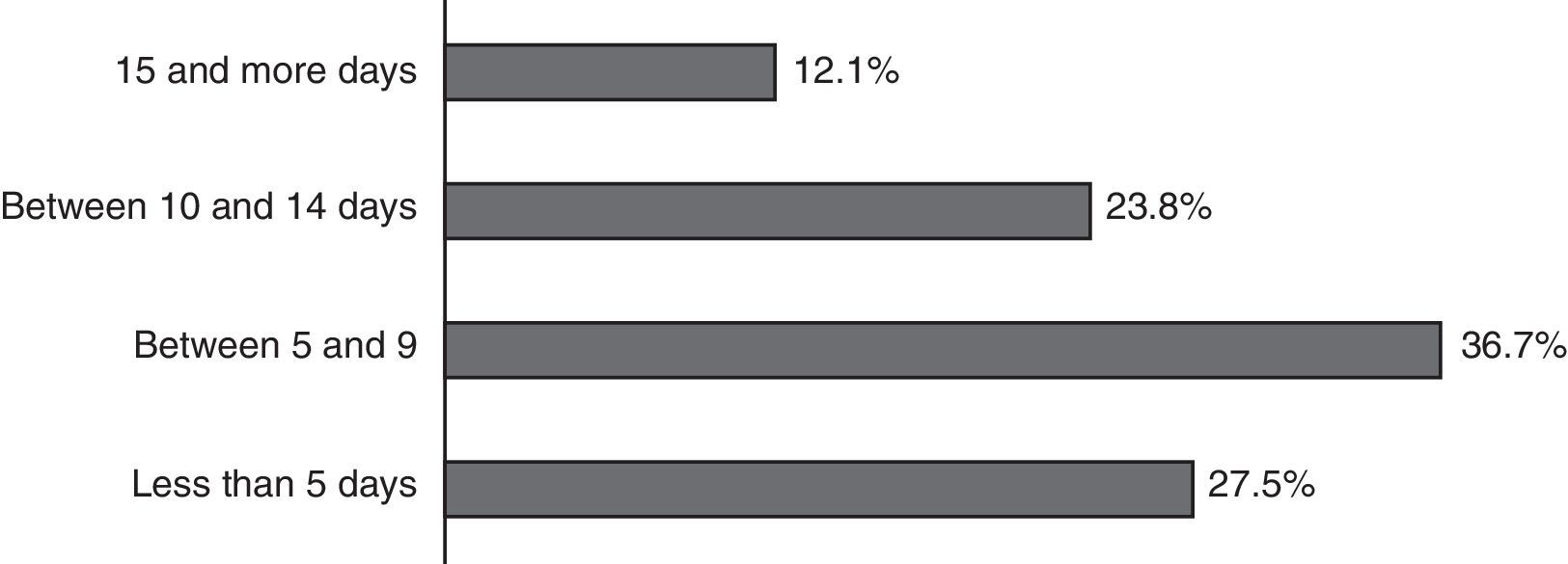
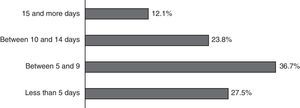
Finally, patients admitted with a diagnosis of mandibular fracture to the Maxillofacial Surgery Service of the Instituto Traumatológico were operated in an average of 8.64 days, with a range between 1 and 48 days, 64% of them being intervened before 10 days after their admission (Fig. 4).
DiscussionThe Instituto Traumatológico Dr. Teodoro Gebauer Weisser is part of a national referral centre for healthcare that mainly treats patients referred from several institutions belonging to the Servicio de Salud Metropolitano Occidente, which includes 15 municipalities of the Metropolitan Region of Chile, with a population of approximately 1,160,000 people.
Results show that between the years 2001 and 2004, there was a low proportion of surgeries due to mandibular fractures, which did not exceed 20 per year. This result is reverted in the following period, in which almost 40 mandibular fractures were operated on in 2010. If we take into account that the study was performed in a healthcare referral centre, where surgeries are scheduled permanently in 2 fixed days of the week, we could attribute the low number of surgeries in the first years of the contemplated period to the fact that the means available did not allow the massive treatment of this type of fractures with open reduction and osteosynthesis with titanium plates, favouring the closed reduction of the fractures and the stabilisation through intermaxillary blockage.
In line with other investigations, such as the one presented by Zúñiga et al. in 2011,9 the present study did not show a monthly or seasonal distribution pattern. In regards to this subject, since it is not an emergency department, and since for the examination of this variable the surgery date was taken into account, the plausibility of any assertion in this regards is limited, since in order to assess this parameter, it would be necessary to carry out the same study in the emergency departments from where the patients are referred, so the exact date of the trauma should be taken into account.
In related studies worldwide, the tendency is that maxillofacial traumas mainly affect men at a ratio from 1.5:1 to 4:1,3,6,9 although there are publications, such as the one carried out by Ahmed et al.,8 that report a ratio of 11.1:1, which may be attributed to population differences, since in the United Arab Emirates, the mainly domestic role of the woman entails a lower exposure to experience events that may lead to facial trauma, as opposed to our society, in which their role is more active. Particularly in regards to mandibular fractures, greater ratios between men and women that go from 4.1:1 to 9.6:12,10,11 have been published, which coincides with this study, where 205 men versus 35 women affected by mandibular fractures were found, resulting in a ratio of 5.9:1.
If we observe the age ranges of the patients in relation with gender, we will find that in practically all of them there is a predominance of the male gender over the female one. However, when reaching 60 years of age, the ratio is inverted, and women are doubly affected in relation with men. This is in agreement with related studies, except for the fact that, in them, the inversion occurs as of the 70 years of age.3,9,12 In Chile, according to the National Statistics Institute, as of the age of 65 years, the number of women becomes noticeably higher than the number of men, which could contribute to the fact that they may have a more active role in comparison with men, which would expose them in a higher degree to experience facial traumas.
In this study, the age of patients who had surgery for mandibular fractures was presented within a range between 14 and 72 years, with an average of 30.3, the most affected age range being the one that comprised the third decade of life, from 20 to 29 years, with 43.3% of the sample total. This coincides with previous international2,8,10,11 and national1,9,13 studies. This is attributed to the fact that this age range is more proactive and prone to reckless attitudes that may generate violent attitudes, vehicle accidents and the practice of dangerous sports and exercises.6 As described in the study by Chrcanovic et al.,2 the prevalence of mandibular fractures in this sample has its peak in the third decade of life, and from there a gradual frequency decrease is produced, from 21.3% in the fourth decade to 2.5% in the range from the sixth decade on.
Chile, according to the World Bank, is one of the 30 developing countries in Latin America. However, aggressions by third parties were responsible for 72.1% of the mandibular fractures of this sample, becoming the main aetiological factor, which is related to, in accordance with literature, developed countries,4,6 whereas traffic accidents are related to developing countries, which coincides with the data published by Henning et al. in 200114 in a hospital in the region of Valdivia. This may be explained by the fact that the Instituto Traumatológico does not have an intensive care unit, essential for the treatment of poly-traumatised patients, which are usually related to high-energy vehicle accidents, and also by the sustained increase of legislative measures for the improvement of road safety in our country, such as the use of seatbelt, higher controls and requirements for vehicles that have been incorporated to the automotive park, etc. In the period contemplated by this study, in accordance with the Ministry of Transportation of Chile, this has contributed to lower mortality and accident rates than in the previous decade, in spite of the sustained increase in the number of cars.
If we observe the relationship between the trauma aetiology and the gender of the patients affected by mandibular fractures in this sample, we find that, except for pedestrian accidents, men prevail over women, and even in sport accidents only men were affected, which is similar to what was observed in other studies,2,6,15 which may be explained because women generally prefer sports in which the degree of physical contact is not such as to allow the occurrence of a mandibular fracture. Accidents on foot or falls to same level are the only aetiological factor in which there is a female predominance, and they are also the main cause of mandibular fractures in people above 60 years, which coincides with the literature published.2,16 This fact could be attributed to intrinsic factors, such as neuromuscular and cognitive disabilities, besides the higher incidence that this gender and age group have in relation to osteoporosis.16
The waiting period of the patients operated for mandibular fractures was 8.64 days in average from the time of formal admission, with complete physical exam, until de day of the surgery per se, most of them (64.2%) being operated within the first 10 days from that date. However, we should add around 10 days more from the time the trauma was produced, which involves initial assistance at an emergency department, immediate referral to the Instituto Traumatológico and the performance of all the supplementary tests needed to perform the surgical intervention. Thus, if we consider approximately 20 days from the time when the fracture is produced until intervention in the pavilion, they would be found at a stage of fibrous or cartilage callous indirect bone healing.17,18 This would be the case whenever there are appropriate stabilisation measures, such as intermaxillary blockage and/or bland diet, so the intentional intraoperative separation of fracture ends would not be necessary to achieve a proper anatomical reduction of the mandibular bone. However, even though it is an adequate period of time for resolution of a mandibular fracture, it is above what has been published by Matos et al. in 2010,11 with an average waiting period of 5.4 day for treatment since the bone lesion occurs.
Out of the total of surgeries performed during the studied period in the Maxillofacial Surgery Service of the Instituto Traumatológico, 31.5% corresponded to mandibular fractures, either isolated or associated with fractures of the rest of the craniofacial region, which gives us information about the high prevalence of this type of fractures, if we take into account that the entire lower third section of the region corresponds only to this bone and the rest is composed by more than 8 bone pieces. This coincides with national and international studies reviewed, that establish a range of 13.3% to 51%.3,6–8,13,14
In this sample, there was an average of 1.47 fractures per patient, which coincides with the literature.1,2 However, the main affected area was the mandibular angle with 42.8% of the sample, followed by the body (37.1%) and the condyle (14.7%,) which differs from international2,6,11 and national2 studies reviewed, where the condylar portion resulted more affected. Such studies contemplate the revision of patients in the emergency department, whereas this study focuses on patients surgically intervened for mandibular fractures, so the proportion of condylar fractures may be underestimated, since there are subtypes of them for which non-surgical treatment is indicated, through a combination of intermaxillary fixation, bland diet and exercises.19,20 In regards to the affected side, the left side was slightly more affected than the right side, being 1.2 times more frequent, a minimum difference that coincides with the literature in this regards.2,4
In 90.4% of the patients operated for mandibular fracture, this was the only bone lesion of the facial skeleton. However, 23 patients (9.6%) also presented 40 fractures of the middle third of the face, 50% of which corresponded to the zygomatic complex, followed by Le Fort (i, ii and iii) fractures, which covered 20% of the fractures associated with the middle third, coinciding with previous publications.2,11
In 2004, Ahmed et al.8 analysed the existing relation between the type of mandibular fracture and the mechanism or aetiology that caused it. The result was that automobile accidents mostly generated condyle fractures, whereas in the case of assaults, the mandibular angle would be the most affected site, which coincides with what was observed in this sample, where 45.7% of the total of mandibular fractures due to aggressions of third parties corresponded to the angle area. However, in this case, aggressions not only corresponded to assaults, but also to domestic violence and fights in public and private places, which limits the comparison. On the other hand, traffic accidents are mainly responsible for fractures of the mandibular body (39.4%), then angle ones (28.9%) and, in the third place, condyle fractures (23.6%), which is related to what has previously been described about the type of treatment that involves patients of this sample.
In 2007, Medina et al.21 exposed a conclusion related to the importance of this type of studies for the prevention, and thus the improvement in the quality of life of the general population, as well as for cost saving by the State. This conclusion states that epidemiology has identified that accidents are not accidental, and there are several conditions that increase the likelihood of experiencing an event, which come from people, the environment and sociocultural circumstances. This explains the permanent or temporary existence of people repeating accidents, which depends on the existence of personalities that do not perceive or give credit to well-known risk factors. The identification of the latter is important to reduce the incidence of these “accidents”.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that there are no conflicts of interest.
To the directives and officers of the Instituto Traumatológico of Santiago de Chile for allowing and facilitating the performance of this study.
Please cite this article as: Zapata S, Pacheco C, Núñez C, Gazitúa G, Cerda P. Epidemiología de las fracturas mandibulares tratadas quirúrgicamente en el Instituto Traumatológico de Santiago (Chile): 10 años de revisión. Rev Esp Cir Oral Maxilofac. 2015;37:138–143.