Breast radiology: New horizons in times of pandemics
More infoAdenomyoepithelioma of the breast (AB) is an uncommon tumor that is characterized by the biphasic proliferation of epithelial and myoepithelial cells. The radiologic findings for AB have been scantly reported. This paper aims to analyze the characteristic findings for AB on ultrasonography (US) and mammography. This retrospective descriptive study used the Breast Imaging-Reporting and Data System (BI-RADS) to analyze the US and mammography findings for histologically confirmed AB in patients attended at our institution between 2007 and 2019. We identified a total of 13 AB in 13 women. All patients underwent US. On US, 12 lesions were seen as oval nodules, and the remaining lesion was irregular-shaped; 8 lesions had circumscribed margins, 3 had angled margins, and 2 had microlobulated margins. Regarding the echo pattern, 8 lesions were hypoechoic and 5 were complex (solid-cystic). On color Doppler, 11 lesions were vascularized nodules and 2 were avascular nodules. In conclusion, we present the imaging characteristics for a series of cases of AB. It is unlikely that this lesion can be suspected solely on the basis of the imaging findings; nevertheless, it is important for radiologists to be familiar with AB to carry out a good radiopathologic correlation.
El adenomioepitelioma mamario (AME) es un tumor poco frecuente que se caracteriza por la proliferación bifásica de células epiteliales y mioepiteliales. Los hallazgos radiológicos de los AME se encuentran escasamente descritos en la literatura científica. El objetivo de nuestro estudio es evaluar las características de imagen del adenomioepitelioma de mama con un enfoque en la apariencia ecográfica y mamográfica. Se realizó un estudio retrospectivo y descriptivo a partir de las biopsias realizadas en nuestra institución entre 2007 y 2019. Se analizaron retrospectivamente los hallazgos en mamografía y ultrasonido, de acuerdo con el léxico del sistema de informes y datos de imágenes mamarias (BI-RADS), de aquellas lesiones que resultaron con histología positiva para adenomioepitelioma. En el período de estudio se encontraron 13 AME en 13 mujeres. Se realizó ecografía a todas las pacientes; 12 lesiones se presentaron como nódulos ovalados y en un caso con forma irregular. Los márgenes fueron circunscritos (n = 8), angulados (n = 3) o microlobulados (n = 2), el patrón de eco fue hipoecoico (n = 8) y complejo sólido-quístico (n = 5). En cuanto a la vascularización, 11 fueron nódulos vascularizados en Doppler color y 2 resultaron avasculares. En conclusión, presentamos las características imagenológicas de una serie de casos de AME. Es poco probable sospechar esta lesión exclusivamente en función de los hallazgos por imagen; sin embargo, es importante conocer esta lesión para realizar una buena correlación radiopatológica.
The term adenomyoepithelioma was first used by Hamperl in 1970.1 Adenomyoepithelioma (AME) of the breast is a rare tumour characterised by biphasic proliferation of epithelial and myoepithelial cells.2 Most of these tumours are benign, but malignant degeneration can also occur, which is why it has been classified as a lesion of “low malignant potential”.3
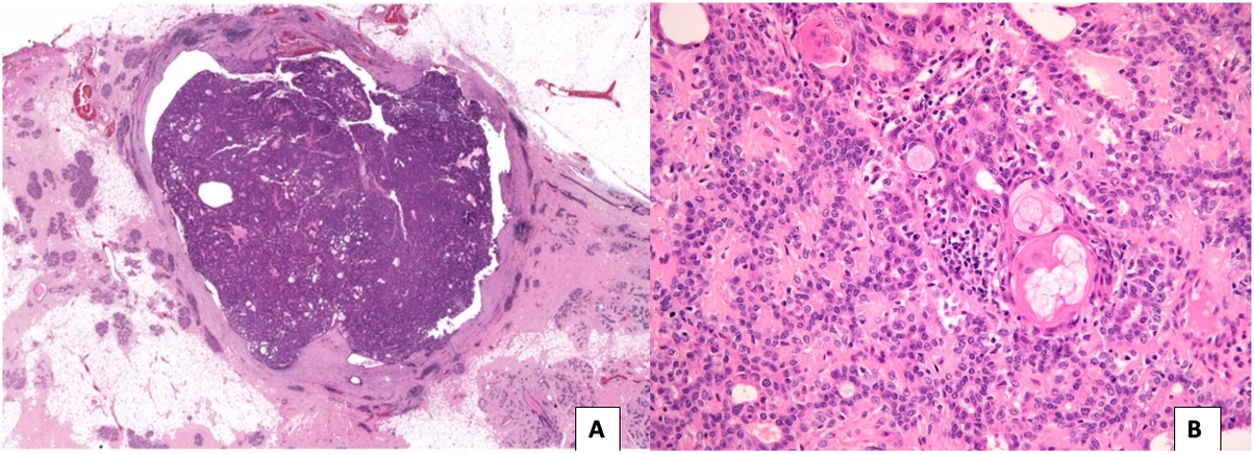
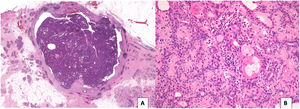
The typical histological appearance of a benign AME consists of acinar structures, composed of an inner layer of epithelial cells with eosinophilic cytoplasm and a prominent peripheral layer of myoepithelial cells. The epithelial component may present hyperplasia and papillomatosis, and foci of apocrine, sweat gland and squamous metaplasia (Fig. 1). The myoepithelial component is made up of polygonal and fusiform cells with clear cytoplasm, with immunoreactivity for p63, calponin, smooth muscle myosin heavy chain (SMMHC), S-100 and smooth muscle actin.4
A) Circumscribed tumour lesion, surrounded by a fibrous capsule, made up of ovoid and rounded glandular structures, densely grouped, with papillary patterned areas (H-E, 10x). B) Glandular structures, with prominent myoepithelial cells, of epithelioid appearance and foci of mature squamous metaplasia and sebaceous metaplasia (H-E 200x).
Malignant transformation may involve only one cell element or both, with the epithelial component being more frequent.5
Regarding its clinical manifestation, patients generally present a solitary palpable nodule. Pain or serous discharge from the nipple are rare.2 AMEs of the breast are more common after the age of fifty, but they are also observed occasionally in young women, and very rarely in men.3
Given their rarity, the radiological findings of AMEs of the breast have seldom been reported in the scientific literature. The objective of our study was to evaluate the mammographic and ultrasound characteristics of AME of the breast.
MethodsA retrospective descriptive study approved by the ethics committee was conducted, based on the biopsies performed at our centre between 2007 and 2019. We analysed the mammographic and ultrasound findings according to the lexicon of the breast imaging reporting and data system (BI-RADS, 5th edition) of those lesions histologically consistent with adenomyoepithelioma.
Patient demographic, clinical, imaging, treatment and follow-up data were collected.
The mammography system used was a Selenia Dimensions 3D (Hologic Inc., Marlborough, MA), while the ultrasound system was a Philips Epiq 7 (Philips Medical Systems, Bothell, WA) with linear transducers between 5 and 18 MHz.
Core biopsies were performed with a Bard Magnum automatic gun and 14 G needles. Between three and 10 samples were taken per lesion, with an average of five.
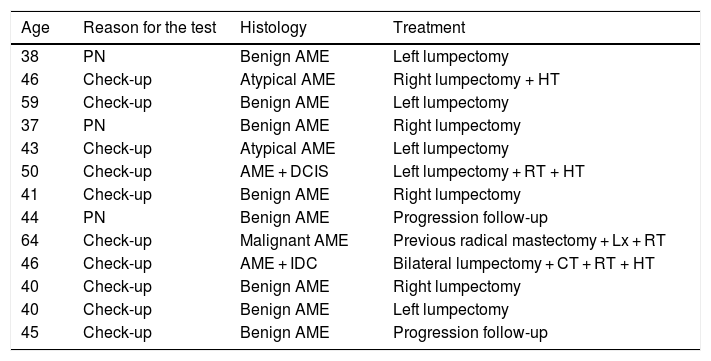
ResultsA total of 13 AMEs were identified in 13 women whose mean age was 45.6 years (range 37-64 years). Three patients consulted for a palpable nodule, while in the rest of the cases the finding was incidental in a routine check-up (Table 1).
Characterisation of the population and treatment.
| Age | Reason for the test | Histology | Treatment |
|---|---|---|---|
| 38 | PN | Benign AME | Left lumpectomy |
| 46 | Check-up | Atypical AME | Right lumpectomy + HT |
| 59 | Check-up | Benign AME | Left lumpectomy |
| 37 | PN | Benign AME | Right lumpectomy |
| 43 | Check-up | Atypical AME | Left lumpectomy |
| 50 | Check-up | AME + DCIS | Left lumpectomy + RT + HT |
| 41 | Check-up | Benign AME | Right lumpectomy |
| 44 | PN | Benign AME | Progression follow-up |
| 64 | Check-up | Malignant AME | Previous radical mastectomy + Lx + RT |
| 46 | Check-up | AME + IDC | Bilateral lumpectomy + CT + RT + HT |
| 40 | Check-up | Benign AME | Right lumpectomy |
| 40 | Check-up | Benign AME | Left lumpectomy |
| 45 | Check-up | Benign AME | Progression follow-up |
AME: adenomyoepithelioma; CT: chemotherapy; DCIS: ductal carcinoma in situ; HT: hormonal therapy; IDC: invasive ductal carcinoma; Lx: lumpectomy; PN: palpable nodule; RT: radiotherapy.
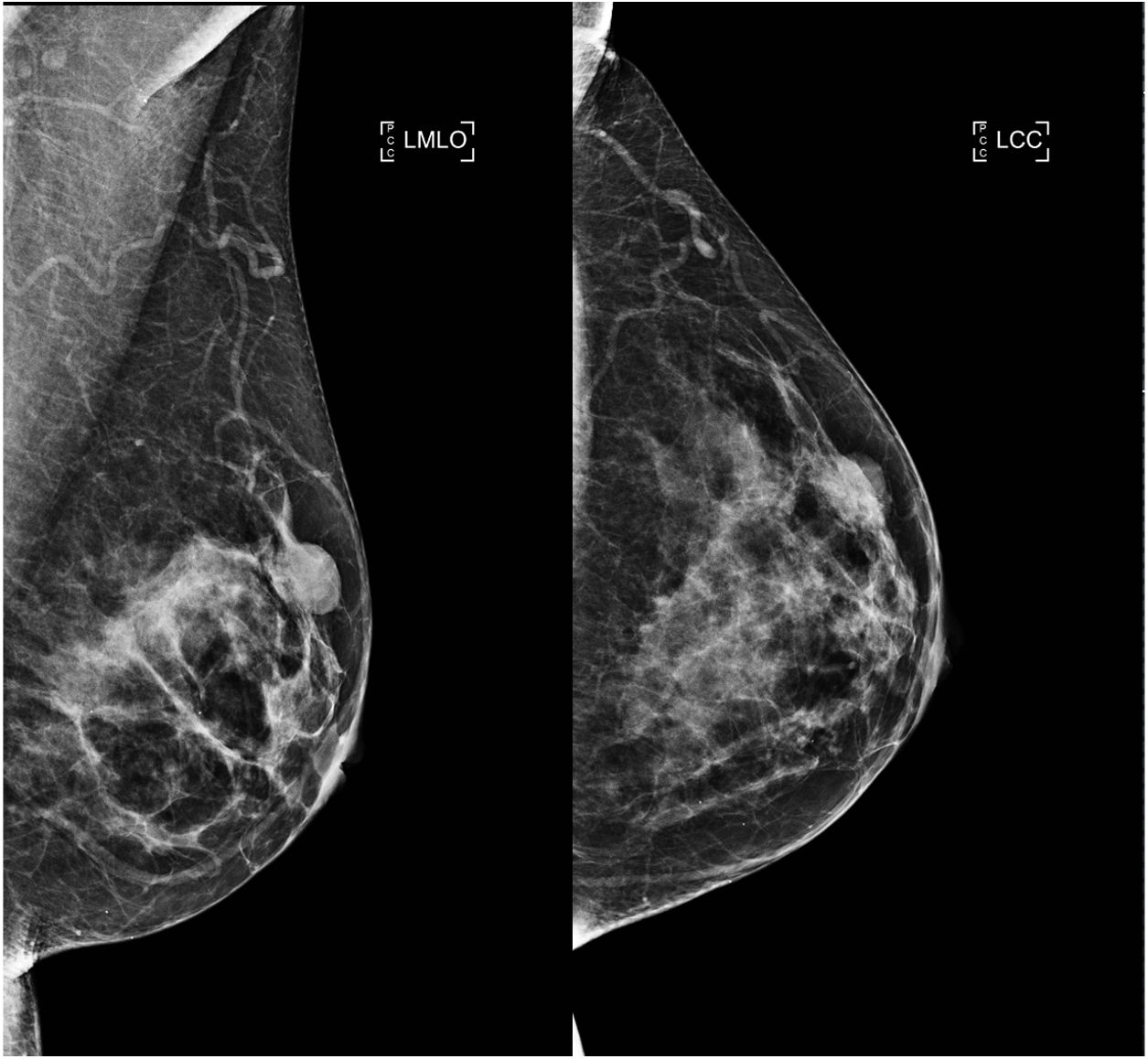
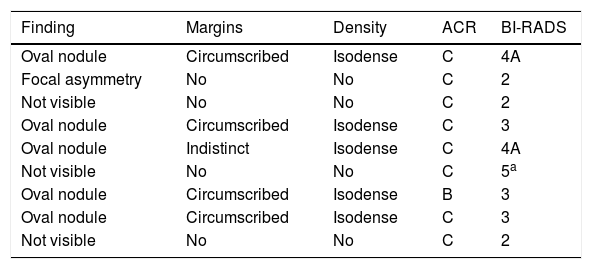
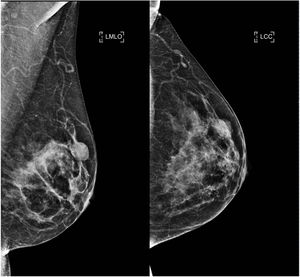
Mammography was performed in nine of the 13 patients studied, with the lesion being visible in six of them. The radiological presentations were: nodule (in five patients) and focal asymmetry (one patient). The nodules were oval, with circumscribed or indistinct and isodense margins, with a mean size of 1.4 cm (range 0.4-2.5). An ACR C (heterogeneously dense) breast density pattern was observed in eight patients. In the remainder, an ACR B pattern (scattered fibroglandular tissue) was observed (Table 2).
Characterisation of lesions on mammography.
| Finding | Margins | Density | ACR | BI-RADS |
|---|---|---|---|---|
| Oval nodule | Circumscribed | Isodense | C | 4A |
| Focal asymmetry | No | No | C | 2 |
| Not visible | No | No | C | 2 |
| Oval nodule | Circumscribed | Isodense | C | 3 |
| Oval nodule | Indistinct | Isodense | C | 4A |
| Not visible | No | No | C | 5a |
| Oval nodule | Circumscribed | Isodense | B | 3 |
| Oval nodule | Circumscribed | Isodense | C | 3 |
| Not visible | No | No | C | 2 |
Mammographic findings were classified as BI-RADS 2 in three cases, BI-RADS 3 in three cases, BI-RADS 4A in two cases and BI-RADS 5 in one case. In this last case, the classification was determined by a second suspicious lesion that did not correspond to the AME of the breast.
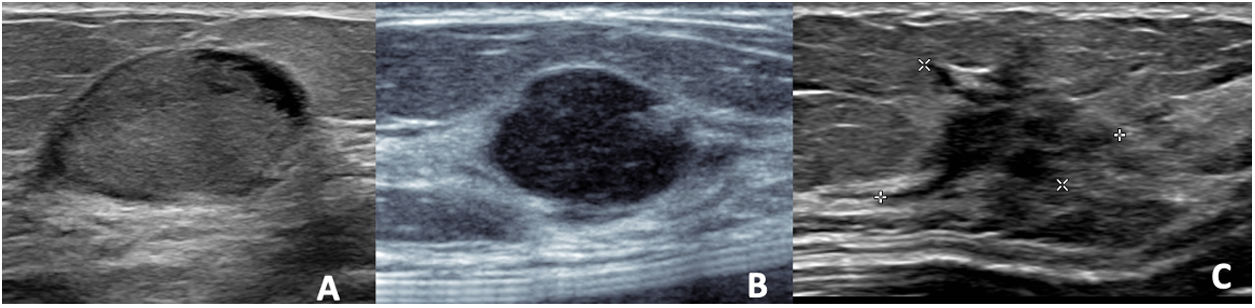
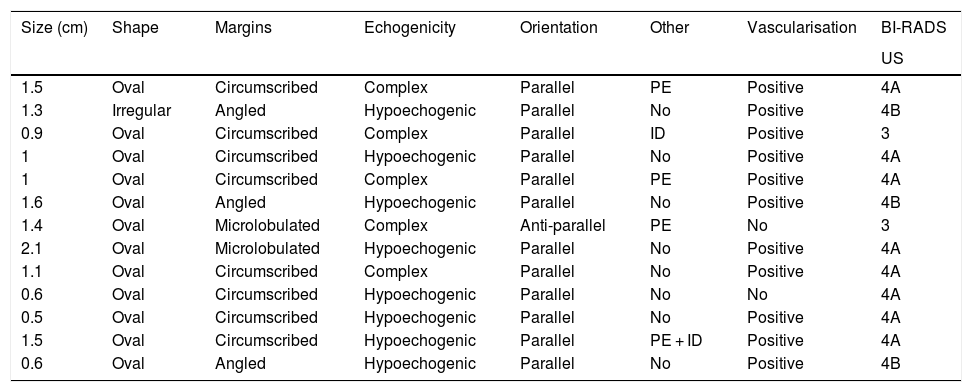
UltrasoundAll cases of AME were identified as nodules in the ultrasound study, all of them oval except for one that was an irregular shape (in correlation with the focal asymmetry seen on mammography).
The mean size of the nodules was 1.2 cm (range between 0.5 and 1.6 cm).
The margins were circumscribed (n = 8), angled (n = 3) or microlobulated (n = 2), while the observed ultrasound pattern was hypoechoic in eight cases (n = 8) and complex (solid-cystic) in five cases (n = 5).
Non-parallel orientation was observed in only one case. In four cases, the nodules exhibited posterior acoustic enhancement. The rest did not exhibit posterior acoustic findings. In two cases, the lesions had an intraductal appearance (Table 3).
Characterisation of lesions on ultrasound.
| Size (cm) | Shape | Margins | Echogenicity | Orientation | Other | Vascularisation | BI-RADS |
|---|---|---|---|---|---|---|---|
| US | |||||||
| 1.5 | Oval | Circumscribed | Complex | Parallel | PE | Positive | 4A |
| 1.3 | Irregular | Angled | Hypoechogenic | Parallel | No | Positive | 4B |
| 0.9 | Oval | Circumscribed | Complex | Parallel | ID | Positive | 3 |
| 1 | Oval | Circumscribed | Hypoechogenic | Parallel | No | Positive | 4A |
| 1 | Oval | Circumscribed | Complex | Parallel | PE | Positive | 4A |
| 1.6 | Oval | Angled | Hypoechogenic | Parallel | No | Positive | 4B |
| 1.4 | Oval | Microlobulated | Complex | Anti-parallel | PE | No | 3 |
| 2.1 | Oval | Microlobulated | Hypoechogenic | Parallel | No | Positive | 4A |
| 1.1 | Oval | Circumscribed | Complex | Parallel | No | Positive | 4A |
| 0.6 | Oval | Circumscribed | Hypoechogenic | Parallel | No | No | 4A |
| 0.5 | Oval | Circumscribed | Hypoechogenic | Parallel | No | Positive | 4A |
| 1.5 | Oval | Circumscribed | Hypoechogenic | Parallel | PE + ID | Positive | 4A |
| 0.6 | Oval | Angled | Hypoechogenic | Parallel | No | Positive | 4B |
Complex: solid-cystic nodules; ID: intraductal; PE: posterior enhancement.
Lesions were classified as BI-RADS 3 in two cases, 4 A in eight cases and 4 B in three cases.
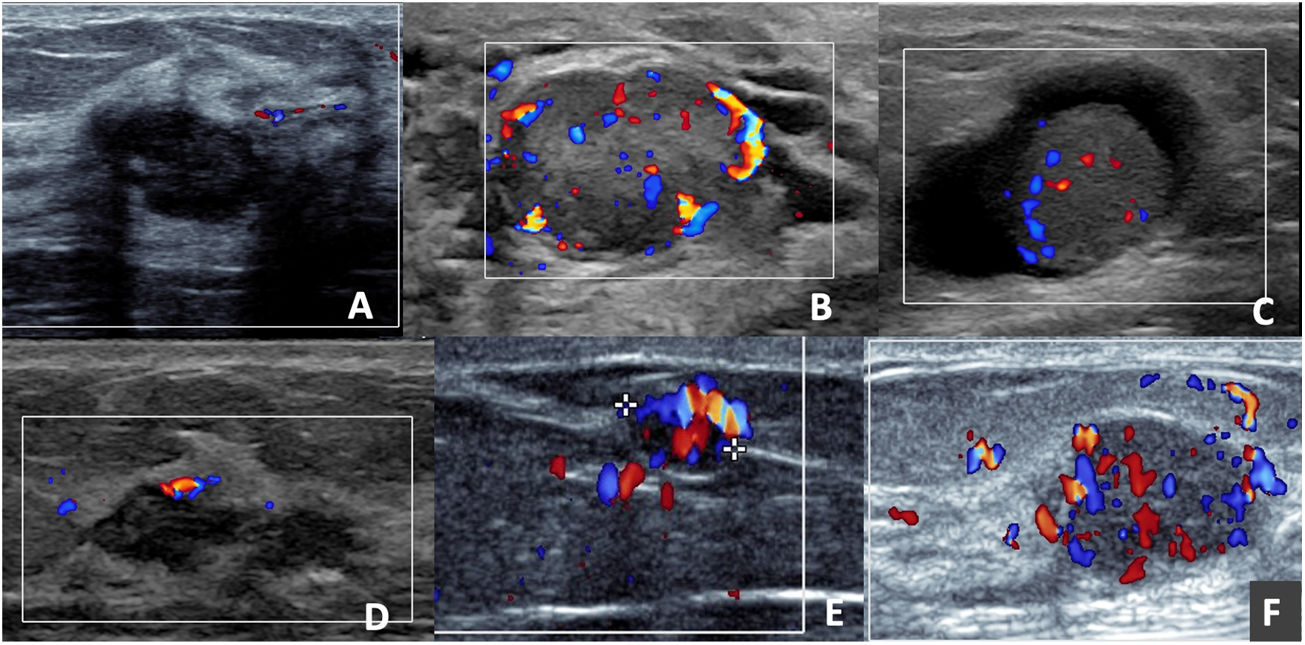
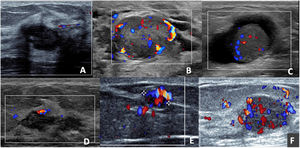
When analysing the AMEs with colour Doppler, the vast majority (11 of 13) presented discharge, the type of vascularisation was internal and peripheral (8 of 11) and with multiple pedicles (7 of 11) (Fig. 2), which led to a preference for biopsy versus short-term follow-up.
Adenomyoepitheliomas in colour Doppler mode. A) Oval, hypoechoic, circumscribed and non-vascularised nodule. B) Oval, hypoechoic, circumscribed nodule, presenting perinodular and intranodular vascularisation. C) Solid-cystic, oval nodule with intranodular vascularisation in the solid portion. D) Nodule with exclusively capsular vascularisation. E) Oval nodule, with marked vascularisation; the presence of a single pedicle leading to the nodule can be observed. F) Oval, hypoechoic nodule, with marked nodular and capsular vascularisation with the presence of multiple tortuous pedicles entering the nodule.
Histopathological analyses revealed one case of malignant AME (it corresponded to a recurrence of a malignant AME operated on two years earlier), an atypical lesion in two cases (in one case it was a recurrence of a malignant AME operated on five years before), coexistence of AME and ductal carcinoma in situ (DCIS) in one case, and invasive ductal carcinoma (IDC) in another case. The rest were benign adenomyoepitheliomas.
The malignant AME of the breast appeared in the area of the scar as a subcutaneous, solid, hypoechoic nodule with irregular margins, measuring 1 cm, and on colour Doppler with multiple vessels in its periphery and some vessels inside.
TreatmentIn our series, 10 of 13 cases were treated with lumpectomy. The only case of malignant AME corresponded to a recurrence in the radical mastectomy site; a lumpectomy was performed and the treatment was supplemented with radiotherapy. The two cases of AME associated with cancer were treated according to the dominant malignant disease; bilateral lumpectomy combined with chemotherapy, radiotherapy and hormonal therapy for AME and IDC, lumpectomy combined with radiotherapy and hormonal therapy for AME and DCIS (Table 1).
Follow-upFollow-up data were available for nine patients, with a range of eight months to 11 years. A recurrence in the surgical scar was identified in two patients. The remaining cases did not have recurrence in the follow-up period.
DiscussionAMEs of the breast are rare tumours characterised by a proliferation of epithelial and myoepithelial elements. Clinically, they are usually detected as palpable nodules, of firm consistency, 1 to 7 cm in size. In our series, most of the cases were asymptomatic, detected in routine annual check-ups. The mean size was 1.2 cm on ultrasound, similar to that described in other series. The average age at the time of diagnosis of an AME of the breast identified in other series is 56.7 years, older than the mean age of 45 years seen in our study.6 This is probably explained by the increase and greater availability of conventional techniques for the early detection of breast lesions in recent years.
On mammography, AME has been described as a dense, generally circumscribed, round or lobulated mass, sometimes with partially defined margins. Calcifications are not typical findings,2 which is consistent with our series, where most of the lesions were circumscribed nodules and there was only one case of focal asymmetry (Fig. 3). It is important to note that the AME was not visible on mammography in three cases, probably due to tissue overlap in the context of dense breasts.
On ultrasound, benign AMEs usually manifest as hypoechoic, circumscribed nodules that may have posterior enhancement, whereas malignant AMEs may appear with non-circumscribed margins and posterior acoustic shadow.7 However, it is not uncommon for benign lesions to look suspicious on ultrasound. In this series of cases, most of the lesions were categorised as BI-RADS 4, but no distinctive characteristics were identified between benign and atypical or malignant AMEs (Fig. 4).
Lee et al. reported five benign AMEs of the breast, two of which presented as complex lesions with a cystic portion and three were solid lesions with ductal dilation, which suggests that AME should be considered in the differential diagnosis of solid-cystic lesions with dilated milk ducts.7 This is similar to our results, since, in our series, five lesions corresponded to complex nodules and in two cases to lesions of intraductal appearance.
In the scientific literature, the type of vascularisation of these lesions has not been systematically described. However, in our series, the role of colour Doppler is important, which facilitated better characterisation of the nodules, since 11 of 13 exhibited discharge and in the vast majority (8 of 11), the vessels were visible both in the periphery and within the lesion and with multiple pedicles (7 of 11) (Fig. 2). These findings differ from the Young Mi Park series, where most of the nodules only exhibited peripheral vascularisation.8 A study by Gkali et al. highlights the role of elastography in the diagnosis of AME of the breast.9 Elastography values were not included in our study, as they were not used routinely at our centre.
Regarding other functional imaging modalities such as magnetic resonance imaging, some clinical case reports have shown variable findings, describing AMEs as oval and smooth masses with a persistent pattern in the kinetic curve; others as spiculated, irregular lesions with a plateau curve.7,10 Magnetic resonance imaging was not performed on any of our patients, since it is not usually part of the imaging protocol for studying visible lesions on ultrasound at our centre.
In pathology, AMEs are mostly solid tumours, well circumscribed, often with a multilobulated contour.7 They may sometimes have a focal cystic component, some being predominantly cystic and others having papillomatous components.5 This variability of presentations is similar to the findings described in this study.
Some publications have concluded that regardless of the characteristics of the lesion, once the histological diagnosis of AME has been confirmed, all those nodules larger than 2 cm should be treated as malignant AMEs of the breast.11
The malignant AME case reported in our series was not metastatic. Metastases have been described in the lung, brain, bone, thyroid, liver, chest wall and axillary lymph nodes.12 The scientific evidence suggests that haematogenous spread is more common than lymphatic spread. The prognosis for AME of the breast associated with distant metastatic carcinoma is poor.
The treatment of choice for AME is surgical, with a wide margin, since local recurrence is not uncommon.13 Therefore, if an AME is diagnosed by core biopsy, total removal of the lesion is recommended, with a wide margin. In our series, the majority of cases were treated with lumpectomy (10 of 13). In the malignant AME case, which corresponded to a recurrence and had been initially treated with radical mastectomy, it was decided to perform a lumpectomy at the site of the scar and supplement with radiotherapy. The two cases of AME of the breast associated with IDC and DCIS were treated according to the dominant malignant disease. Finally, two patients refused surgery and were later lost to follow-up.
The differential diagnosis of AME of the breast covers a wide spectrum of conditions, including papillary pathology, fibroadenoma, phyllodes tumour, tubular adenoma and carcinoma, microglandular adenosis, adenoid cystic carcinoma, pleomorphic adenoma and mesenchymal stromal proliferations of the breast. In most cases, the images will be nonspecific and it will be the histology and immunohistochemical findings that will establish the definitive diagnosis.
The limitations of this study are its retrospective analysis and that we only evaluated mammography and ultrasound as imaging techniques. It would be interesting to know the functional behaviour of these lesions on, for example, magnetic resonance imaging or contrast-enhanced mammography.
ConclusionWe have presented one of the most extensive case series of AME of the breast, describing its mammographic and ultrasound characteristics.
On sonography, AMEs more commonly present as oval, hypoechoic or solid-cystic nodules, where colour Doppler plays a relevant role, since a significant proportion of the nodules are internally and peripherally vascularised.
Given its low frequency and indeterminate findings, AME is unlikely to be suspected exclusively based on imaging findings, but it is important to know about these lesions in order to conduct a good radio-pathological correlation.
Authorship- 1
Responsible for study integrity: MU.
- 2
Study conception: MU, MÁP.
- 3
Study design: MU, CG.
- 4
Data collection: CG, DH.
- 5
Data analysis and interpretation: MU, CG.
- 6
Statistical processing: MU, CG.
- 7
Literature search: MU, CG, DH.
- 8
Drafting of the article: MU, CG, DH.
- 9
Critical review of the manuscript with intellectually relevant contributions: MU, MÁP.
- 10
Approval of the final version: MU.
This study received no specific grants from public agencies, the commercial sector or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Uchida M, Gatica C, Hasson D, Gallegos M, Pinochet MÁ. Adenomioepitelioma de la mama desde una perspectiva radiológica. Radiología. 2022;64:37–43.