Suplement “"Advances in Thoracic Radiology”
More infoMesothelioma is an infrequent neoplasm with a poor prognosis that is related to exposure to asbestos and whose peak incidence in Europe is estimated from 2020. Its diagnosis is complex; imaging techniques and the performance of invasive pleural techniques being essential for pathological confirmation. The different diagnostic yields of these invasive techniques are collected in the medical literature. The present work consisted of reviewing how the definitive diagnosis of mesothelioma cases in our centre was reached to check if there was concordance with the data in the bibliography.
Materials and methodsRetrospective review of patients with a diagnosis of pleural mesothelioma in the period 2019–2021, analysing demographic data and exposure to asbestos, the semiology of the radiological findings and the invasive techniques performed to reach the diagnosis.
ResultsTwenty-six mesothelioma cases were reviewed. 22 men and 4 women. Median age 74 years. 9 patients had a history of asbestos exposure. Moderate-severe pleural effusion was the most frequent radiological finding (23/26). The sensitivity of the invasive techniques was as follows: Cytology 13%, biopsy without image guidance 11%, image-guided biopsy 93%, surgical biopsy 67%.
ConclusionsIn our review, pleural biopsy performed with image guidance was the test that had the highest diagnostic yield, so it should be considered as the initial invasive test for the study of mesothelioma.
El mesotelioma es una neoplasia poco frecuente y con mal pronóstico que se relaciona con la exposición al asbesto y cuyo pico de incidencia en Europa se estima a partir del 2020. Su diagnóstico es complejo, siendo fundamentales las técnicas de imagen y la realización de técnicas invasivas pleurales para la confirmación anatomopatológica. En la bibliografía médica se recogen las distintas rentabilidades diagnósticas de estas técnicas invasivas. El presente trabajo consistió en revisar cómo se llegó al diagnóstico definitivo de casos de mesotelioma de nuestro centro para comprobar si existía concordancia con los datos de la bibliografía.
Materiales y métodosRevisión retrospectiva de pacientes con diagnóstico de mesotelioma pleural en el periodo 2019–2021 analizando los datos demográficos y de exposición a asbesto, la semiología de los hallazgos radiológicos y las técnicas invasivas realizadas para llegar al diagnóstico.
ResultadosSe revisaron 26 casos de mesotelioma. 22 hombres y 4 mujeres. Edad media de 74 años. 9 pacientes tenían antecedentes de exposición al asbesto. El derrame pleural moderado-importante fue el hallazgo radiológico más frecuente (23/26). La sensibilidad de las técnicas invasivas fue de un 13% para la citología, de un 11% para la biopsia sin guía de imagen, de un 93% para la biopsia guiada por técnicas de imagen y de un 67% para la biopsia quirúrgica.
ConclusionesEn nuestra revisión la biopsia pleural guiada con técnicas de imagen fue la prueba que tuvo mayor rentabilidad diagnóstica por lo que habría que considerarla como la prueba invasiva inicial para el estudio de mesotelioma.
Mesotheliomas are the most common primary neoplasm in the pleura, and 80% of cases are related to exposure to asbestos, a material used until the mid-20th century by a wide range of professions in the Western world, especially in the construction and automobile industries. In Spain, its use has been banned since 2002.
It is a rare neoplasm with a poor prognosis. In Europe, the incidence rate is estimated at 20 cases/million per year.1 Due to the long latency period between exposure and disease onset, it is estimated that peak incidence in Europe will occur from 2020 onwards. In developing countries, where asbestos is still used, this incidence may rise in the future.
Diagnosis is based on pathological findings showing atypical mesothelial proliferation and immunohistochemical results consistent with mesothelioma. To reach a diagnosis, it is usually necessary to perform several invasive techniques, such as thoracentesis, image-guided and non-image-guided percutaneous pleural biopsies, and surgical biopsies. Computed tomography (CT) is essential in the study of mesothelioma, and in some cases, PET-CT is used. Treatment consists of chemotherapy and immunotherapy while surgical treatment may be considered for certain patients.
The aim of this paper is to describe the different techniques used in the pathological confirmation of mesothelioma and analyse their diagnostic performances with cases from our centre.
Materials and methodsWe conducted a retrospective review of mesothelioma cases diagnosed in our centre from 2019 to 2021. The required data were extracted from the patients’ medical records. The characteristics of the study were such that we requested a waiver of informed consent for access to the patients’ data, with the agreement of the centre’s Clinical Research Ethics Committee.
Consecutive sampling was used to include all patients with a pathological diagnosis of pleural mesothelioma from 2019 to 2021 who had undergone a chest CT scan.
Epidemiological data were collected: age, sex and history of asbestos exposure. We reviewed the imaging tests (CT) analysing the following findings: pleural effusion, measurement of pleural thickening, mediastinal and fissural thickening, existence of pleural plaques in locations typically associated with asbestos exposure (most common in lung bases, sparing the costophrenic angles and the apices), enlarged nodes or distant metastasis and the existence of interstitial lung disease. Pleural thickening was measured by assessing the largest diameter perpendicular to the pleura in the mediastinal window. For this study, pleural effusion was considered to be minimal if the thickness of the pleural cavity measured less than 1 cm, and moderate to significant if it was greater than 1 cm.
The CT scans were analysed by two radiologists from the thoracic radiology department of our centre, both with more than 10 years of experience. The helical multislice technique with intravenous contrast was used for all CT studies of the lung bases in the arterial phase and portal venous phase. They also reviewed PET/CT images where it was performed as a complementary technique.
In addition, we analysed the invasive techniques that were necessary to reach a definitive pathological diagnosis: pleural fluid cytology obtained through thoracentesis, image-guided (ultrasound or CT) or non-image-guided percutaneous biopsy, surgical biopsy and others.
Non-image-guided pleural biopsy was performed with a 13G Abrams needle. The image-guided biopsy was performed with a semi-automatic 18G needle without an introducer needle. Endoscopic sampling was performed in endobronchial ultrasound (EBUS) and endoscopic ultrasound (EUS) with 22G needles.
We used Stata 17 to analyse the data and perform a sensitivity analysis for each technique.
ResultsOur consecutive sampling identified 28 patients in the 2019–2022 period. In two cases, despite highly suggestive imaging findings, there was no pathological diagnosis, so the final number of cases to be analysed was 26.
The mean age of the patients was 74 years (SD: 8.5). There were 22 men and 4 women. Nine had been exposed to asbestos.
In terms of imaging findings: 23 had moderate to significant pleural effusion, two had minimal pleural effusion, and one had no effusion. Twenty-three patients had pleural thickening (thickness > 1 cm: 13; thickness < 1 cm: 10) and three patients had no pleural thickening. In 20 cases there was mediastinal thickening, and in seven cases there was fissural thickening. Four patients had enlarged mediastinal lymph nodes. Only three patients presented with plaques typical of asbestos contact (one of them had no history of exposure) and only one case reported radiological signs of interstitial involvement suggestive of asbestosis.
Nine patients underwent a PET/CT scan as a complementary study.
The invasive tests performed to investigate the pleural pathology included thoracentesis in 23 cases; in the remaining three cases, thoracentesis was not performed because there was no pleural fluid or only minimal effusion. Pleural biopsy was performed without imaging guidance in nine cases. Image-guided biopsy was performed on 14 patients (13 with CT, one with ultrasound). Surgical biopsy was performed via thoracoscopy in 12 cases. Other invasive techniques were used on two patients: in one case EBUS was performed to assess mediastinal lymph nodes and in another case EUS was carried out on a paramediastinal pleural thickening that was accessed for biopsy from the oesophagus.
The pathological confirmation of mesothelioma was carried out with the following invasive techniques and respective sensitivities (S): 3/23 cytology (S: 13%), non-image-guided biopsy 1/9 (S: 11%), image-guided biopsy 13/14 (S: 93%), surgical biopsy 8/12 (S: 67%) and other biopsies (EBUS and EUS) 1/2 (S: 50%).
The definitive pathological result was malignant mesothelioma in all cases. In 10 cases the histological variant could not be specified. Of the others, eight were epithelioid mesotheliomas, five were sarcomatoid and three were biphasic.
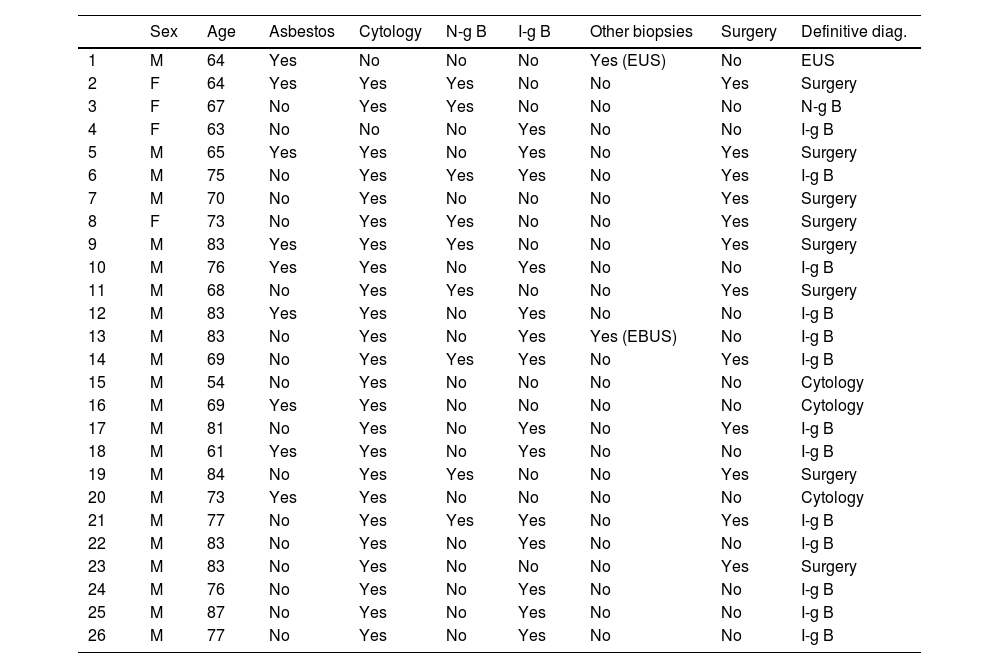
Table 1 provides a detailed description of the demographic data, the history of asbestos exposure, the invasive techniques used and the technique by which the definitive diagnosis was made.
Patient demographics, history of asbestos exposure and description of the pleural invasive techniques performed in each case and the technique by which the definitive diagnosis was obtained.
| Sex | Age | Asbestos | Cytology | N-g B | I-g B | Other biopsies | Surgery | Definitive diag. | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 64 | Yes | No | No | No | Yes (EUS) | No | EUS |
| 2 | F | 64 | Yes | Yes | Yes | No | No | Yes | Surgery |
| 3 | F | 67 | No | Yes | Yes | No | No | No | N-g B |
| 4 | F | 63 | No | No | No | Yes | No | No | I-g B |
| 5 | M | 65 | Yes | Yes | No | Yes | No | Yes | Surgery |
| 6 | M | 75 | No | Yes | Yes | Yes | No | Yes | I-g B |
| 7 | M | 70 | No | Yes | No | No | No | Yes | Surgery |
| 8 | F | 73 | No | Yes | Yes | No | No | Yes | Surgery |
| 9 | M | 83 | Yes | Yes | Yes | No | No | Yes | Surgery |
| 10 | M | 76 | Yes | Yes | No | Yes | No | No | I-g B |
| 11 | M | 68 | No | Yes | Yes | No | No | Yes | Surgery |
| 12 | M | 83 | Yes | Yes | No | Yes | No | No | I-g B |
| 13 | M | 83 | No | Yes | No | Yes | Yes (EBUS) | No | I-g B |
| 14 | M | 69 | No | Yes | Yes | Yes | No | Yes | I-g B |
| 15 | M | 54 | No | Yes | No | No | No | No | Cytology |
| 16 | M | 69 | Yes | Yes | No | No | No | No | Cytology |
| 17 | M | 81 | No | Yes | No | Yes | No | Yes | I-g B |
| 18 | M | 61 | Yes | Yes | No | Yes | No | No | I-g B |
| 19 | M | 84 | No | Yes | Yes | No | No | Yes | Surgery |
| 20 | M | 73 | Yes | Yes | No | No | No | No | Cytology |
| 21 | M | 77 | No | Yes | Yes | Yes | No | Yes | I-g B |
| 22 | M | 83 | No | Yes | No | Yes | No | No | I-g B |
| 23 | M | 83 | No | Yes | No | No | No | Yes | Surgery |
| 24 | M | 76 | No | Yes | No | Yes | No | No | I-g B |
| 25 | M | 87 | No | Yes | No | Yes | No | No | I-g B |
| 26 | M | 77 | No | Yes | No | Yes | No | No | I-g B |
N-g B: non-image-guided biopsy; I-g B: image-guided biopsy; EBUS: endobronchial ultrasound; EUS: endoscopic ultrasound; F: female; M: male.
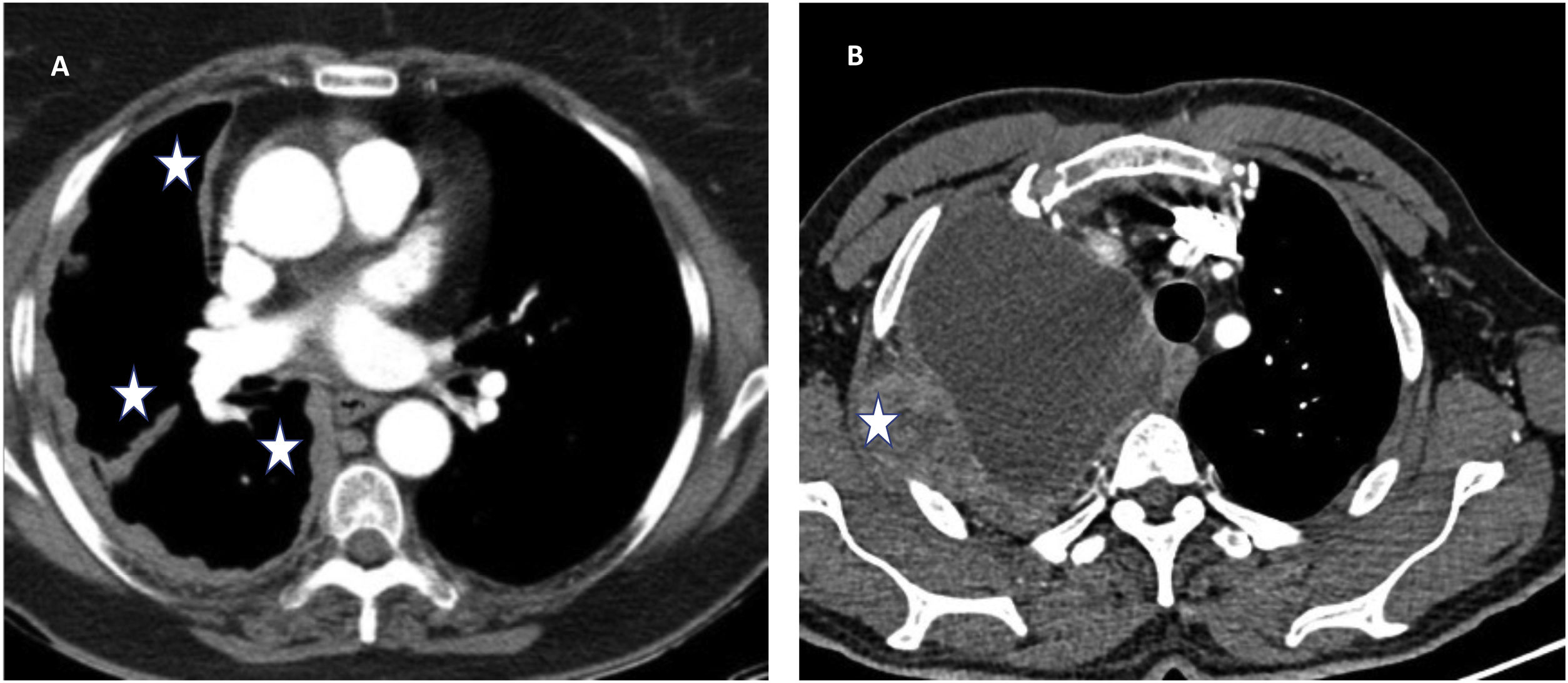
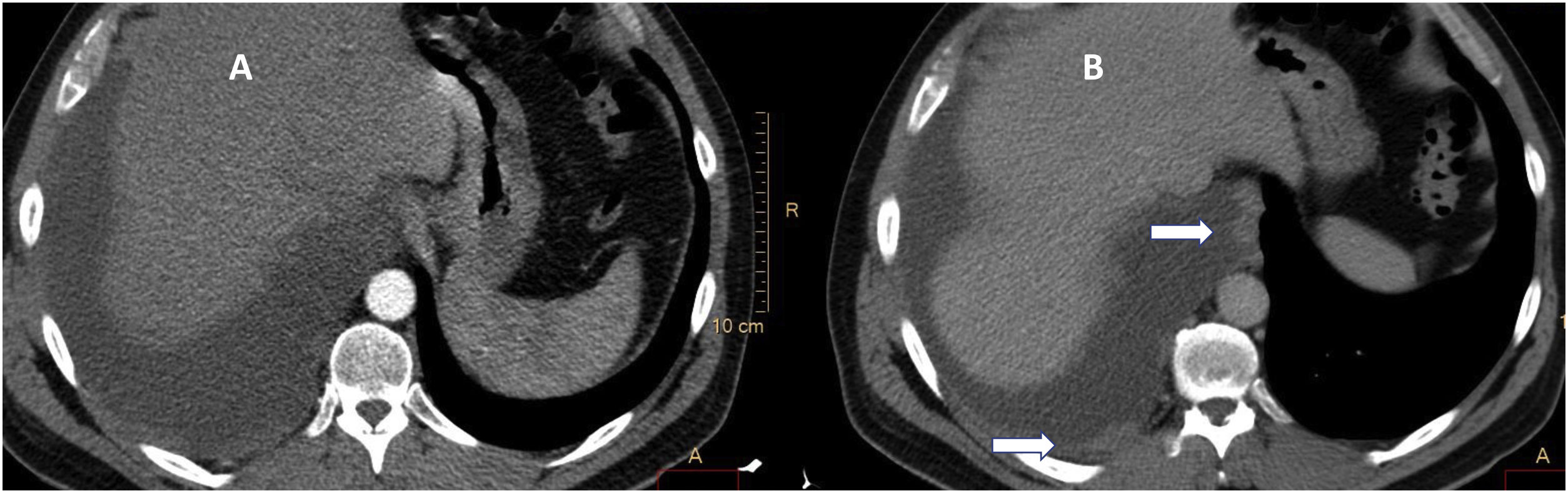
Pleural effusion is the most frequent manifestation of pleural mesothelioma, and may be associated with nodular thickening which would support the diagnosis of malignant pleural disease, mainly in the mediastinal, fissural or diaphragmatic pleura2–4 (Fig. 1). These findings are best visualised on late or portal phase contrast-enhanced CT studies5 (Fig. 2).
Radiological signs of malignant pleural effusion A) Nodular pleural thickenings (in some areas greater than 1 cm) with involvement of the mediastinal and fissural pleura (stars) typical of malignant pleural disease. There is also evidence of volume loss in the right hemithorax. B) Pleural effusion with malignant pleural thickening greater than 1 cm that has spread to the chest wall (star).
Solid pleural implants were better visualised with contrast enhancement in the venous phase. Image A, arterial phase, little evidence of a solid implant in the posterior pleura. The same study in the portal venous phase (B) enables the visualisation of solid implants indicating a suspected malignant effusion in the pleura of the azygo-oesophageal recess and in the posterior pleura (arrows).
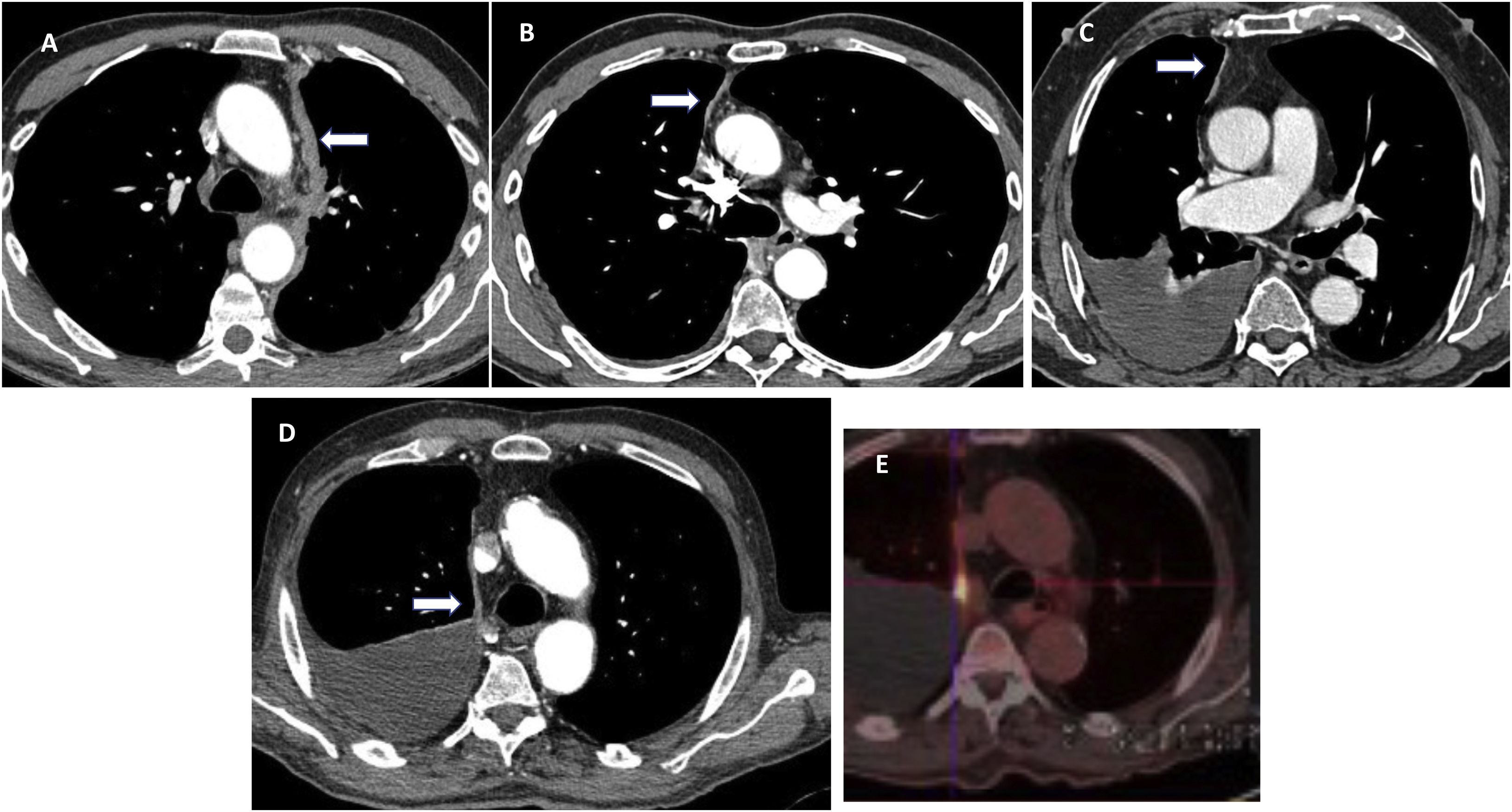
The key differential diagnosis is carried out with metastatic pleural diseases.6 In our series, the high incidence of mediastinal pleural thickening, in some cases very subtle, is striking (20 out of 26 cases) (Fig. 3). This finding has already been described as a general sign of malignant pleural disease. However, it could be more indicative of mesothelioma and comparative studies with a larger number of cases are needed to confirm this.
CT scan of mesothelioma cases in which, as a sign of pleural tumour involvement, there is concentric thickening and involvement of the mediastinal pleura (arrows), in some cases subtle and with or without effusion. In figures A, B and C there is also a loss of volume in the hemithorax. Image D shows subtle thickening of the mediastinal pleura and its correlation with PET uptake (E).
Thoracentesis is the initial invasive test used to assess pleural effusion, although it performs poorly in the diagnosis of mesothelioma. In a recent meta-analysis, the sensitivity of pleural fluid cytology obtained through thoracentesis for the diagnosis of pleural mesothelioma was 28.9%.7 Cytology may be considered sufficient for the diagnosis of mesothelioma in some cases, for example, if there is atypical mesothelial proliferation, compatible immunohistochemical evidence, nodular thickening on imaging and no evidence of an extrapleural tumour.8 There is also evidence that homozygous deletion of P16 by FISH (fluorescence in situ hybridisation)9 techniques could differentiate between malignant mesothelioma and reactive mesothelial proliferations. This technique, when applied to thoracentesis samples, can improve the value of cytology in centres where it is available.
Another invasive test is pleural biopsy. This technique was performed ‘blind’, without guided imaging for a long time, with poor diagnostic outcomes, between 21 and 43%.10 Pleural effusion must be present to perform both thoracentesis and non-image-guided biopsies.
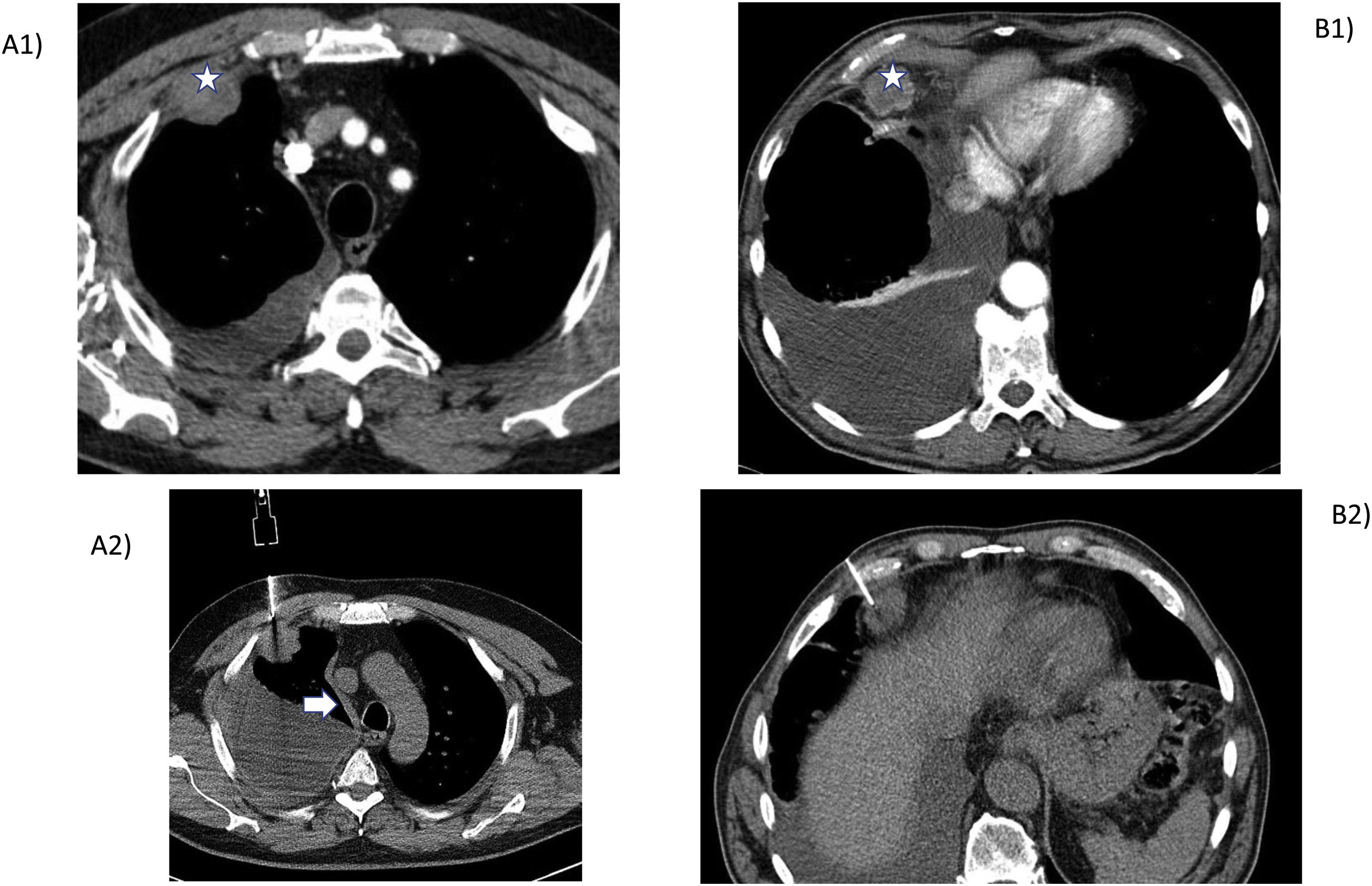
As the use of imaging techniques, mainly CT, has become more widespread, studies have begun to report the increased benefits of image-guided biopsies,10–12 due to the advantage of being able to direct the biopsy to the area where the solid lesion is located (Fig. 4). This emphasises the importance of estimating the size of pleural thickening prior to the procedure, although acceptable performance even with millimetric thickening has also been reported. In our series, out of 13 cases diagnosed by image-guided biopsy, pleural thickness was > 1 cm in 11 cases and < 1 cm in 2 cases.
CT-guided biopsies with pathological finding of mesothelioma. A1) Pleural effusion and focal nodular thickening of anterior location (star) on which the image-guided biopsy was directed (A2). Arrow in A2): thickening of mediastinal pleura. B1) Pleural effusion and enlarged lymph nodes (star) in the fat of the cardiophrenic angle on which the image-guided puncture was performed (B2) as the cytology of the fluid was non-diagnostic.
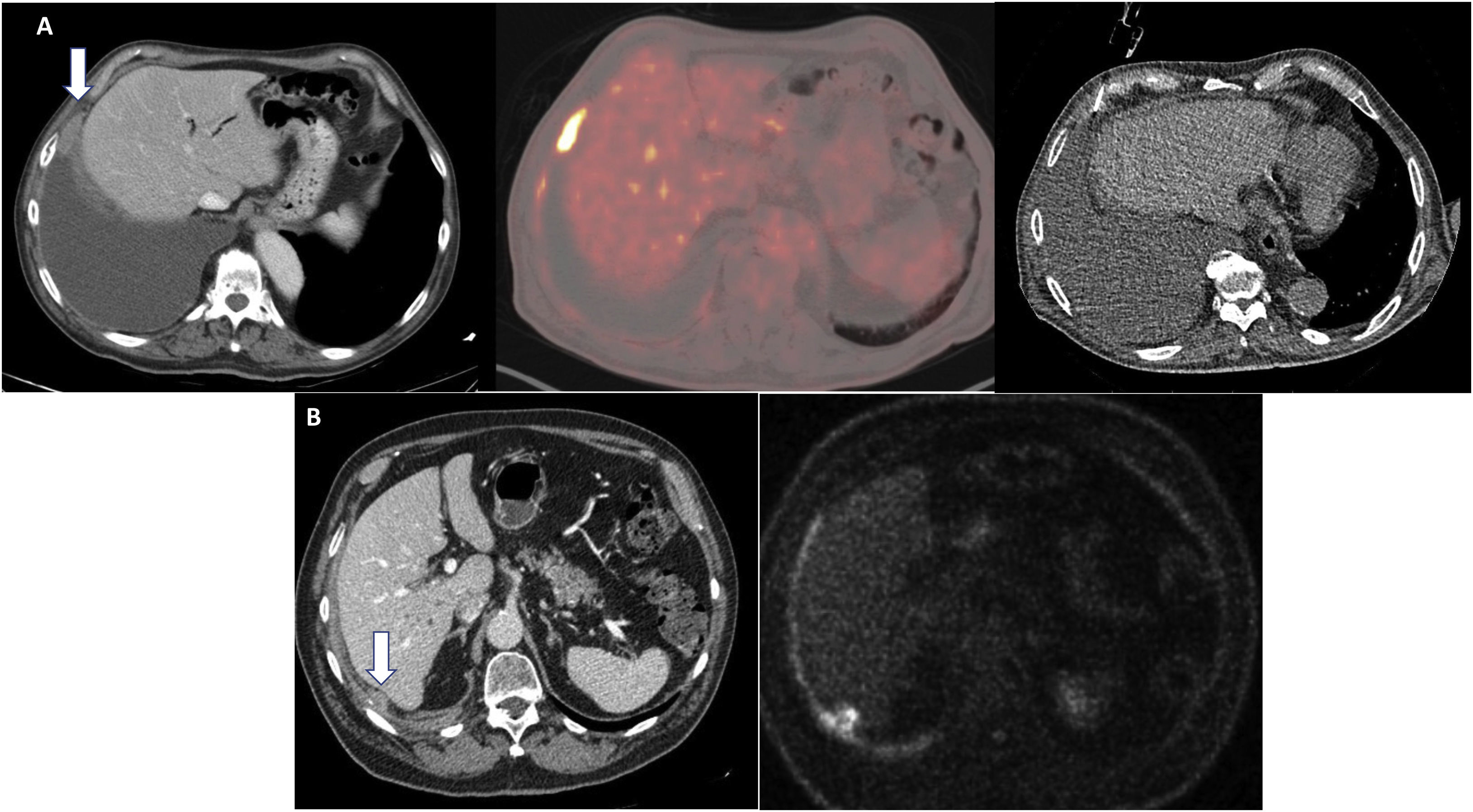
Other techniques, such as PET, can also help direct the biopsy.1,13 In our cases, the PET findings in four patients helped to select the region for biopsy (Fig. 5), which confirms that this technique can be a useful complement to CT for improving accuracy in locating the most metabolically active and accessible pleural region for sampling.
Utility of PET in the assessment of pleural solid implants in cases of mesothelioma prior to image-guided biopsy. A) contrast-enhanced CT scan in portal phase. Significant right pleural effusion with isolated focal pleural thickening in the lateral costophrenic recess (arrow). Hyperenhancement of pleural solid thickening on PET image. On non-contrast CT, no pleural thickening was seen on biopsy; the biopsy was directed by the findings on contrast CT and PET. B) Focal perihepatic pleural thickening barely visible on CT (arrow) and with hyperenhancement on PET, on which diagnostic image-guided biopsy was performed.
Being able to make the diagnosis with minimally invasive percutaneous biopsy techniques on an outpatient basis with few complications reduces the need for surgery to confirm the diagnosis. Surgery, considered the gold standard and technique of choice for the diagnosis of pleural mesothelioma in some guidelines,14,15 can also produce false negatives and a sensitivity of 95% in some series. In cases where pleurodesis is required to treat the effusion, thoracoscopy is the technique of choice, as diagnosis and treatment can be performed in the same procedure.
In our series, surgical biopsy in four patients showed non-specific pleuritis, and due to the high suspicion of a tumour, an image-guided biopsy was subsequently performed and a definitive diagnosis of mesothelioma was made. After reviewing these cases, pleural thickening was less than 1 cm or patchy in all cases, and this may be the possible cause of the lower performance of surgery in our series. PET was useful in selecting the area to be biopsied for two of our patients.
Diagnosing mesothelioma is complex, and as our series shows, in many cases several invasive diagnostic tests are required, which can delay diagnosis. In our study only five patients required an invasive test for diagnosis, 10 patients required two tests, eight patients required three tests and three patients required four tests.
The main limitations of our study are the retrospective nature of the study and the limited number of cases analysed at a local level.
Our review suggests that, among the different minimally invasive/invasive techniques available to reach the pathological diagnosis of pleural mesothelioma, image-guided percutaneous pleural biopsy is a good option due to its high diagnostic performance compared to other available techniques.
FundingThis project has not received any funding.
Author contributionsHelena Gómez Herrero: Development of study concept and design. Data analysis and interpretation. Editing and approval of final version.
Begoña Álvarez Galván: Data analysis and interpretation.
Conflicts of interestThe authors declare that they have no conflicts of interest.