In 2008, stroke mortality, morbidity, and disability rates in Aragon were higher than the average in Spain. These data underscored the need to develop a stroke care programme (PAIA).
Materials and methodsWe present the dynamics of planning, implementation, evaluation, and improvement developed between 2009 and 2014 as well as the results of the PAIA after that 5-year period.
ResultsStructure, processes, and outcomes have improved with reference to the key indicators of healthcare (audit: 2008, 2010, 2012) among others: stroke rate in 2013 was 2.07 (2.36 in 2008); 78% of strokes were managed in stroke units in 2014 (30% in 2008); rate of fibrinolysis was 8.3% in 2014 (4.4% in 2010); fibrinolysis was administered in secondary hospitals (30% of the total); fibrinolysis was administered by Telestroke in 9%; stroke mortality decreased (38%); 67.7 years of potential life lost (YPLL) in 2013 (144 in 2008); nurse training; development of neurosonology; networking; sharing protocols and best practices between health sectors, etc.
ConclusionsIntegrated process management and multidisciplinary teams distributed and deployed over an entire territory with established protocols, references, evaluations, and continuous development, have been proven powerful tools to ensure both quality and equality. The PAIA is a good example of clinical governance and networking due to its dynamic and sustained improvement and cooperation between clinicians.
En 2008, Aragón tenía tasas de morbimortalidad y discapacidad por ictus superiores a las del conjunto de España. Se estableció la necesidad de desarrollar un Programa de Atención al Ictus (PAIA).
Material y métodosDamos a conocer la dinámica de planificación, implantación, evaluación y mejora que se ha desarrollado entre los años 2009-2014 y sus resultados a 5años.
ResultadosSe ha mejorado en la estructura, en los procesos y en los resultados, con mejoría en los indicadores clave de la asistencia (audit 2008-2010-2012) y otros: tasa ictus 2013: 2,07 (2008: 2,36); 78% ictus atendidos en áreas/unidades en 2014 (30%, 2008); tasa fibrinólisis 8,3% en 2014 (4,4%, 2010); fibrinólisis hospitales secundarios (30% total); fibrinólisis con teleictus 9%; descenso de la mortalidad por ictus, 38%; años de vida prematura perdidos 67,7 (2013)/144 (2008); capacitación de enfermería, desarrollo de la neurosonología, trabajo en red, con protocolos y buenas prácticas compartidos entre sectores sanitarios, etc.
ConclusionesLa gestión por procesos y equipos multidisciplinares desplegados en una distribución territorial integral, con protocolos y referencias establecidas y una dinámica de evaluación y mejora continua, ha demostrado ser una herramienta potente para garantizar la calidad y la equidad. El PAIA, por su dinámica de mejora sostenida y la implicación de los clínicos, es un buen ejemplo de gestión clínica y trabajo en red.
In the last 15 years, offering patients with stroke the best possible care has been one of the major organisational and clinical challenges. The advent of fibrinolytic treatment with recombinant tissue plasminogen activator (rTPA) in the late 1990s, the creation of stroke units with well-defined protocols and specially trained nurses, and the need to optimise response times immediately after stroke occurs have driven significant changes in terms of organisation and interactions with other professionals, and the role of neurologists.
Neurologists have had to lead the way in a change of mentality and in a huge administrative effort to implement code stroke and integrated care for these patients. The burden of this task will increase with the extension of neurointervention techniques to hyperacute stroke.
This has required neurologists to take on a vast amount of management work and liaise with numerous hospital professionals and prehospital services, in addition to performing their usual role as experts in cerebrovascular disease (CVD). Most importantly, neurologists have had to work towards agreements with hospital directors and regional government.
Decision-making power in this sector rests with the health service of each autonomous community, so work must be performed in collaboration with these bodies. Each neurology department and autonomous community has established a stroke management system with different response times, support, and outcomes.
The Spanish National Health System's 2008 Stroke Strategy1 and the national stroke care plan2 required a major push to put the disease on the political agenda and to unify the approach to stroke care to some extent.
Over the years, several autonomous communities have published stroke care plans, all founded on process-based management, integrating the work of all the actors and resources in the chain of care.3–7 However, few autonomous communities have evaluated these plans’ implementation and outcomes; fewer still have published the findings of such an assessment.8–11
This study reports the planning, implementation, evaluation, and improvement of the Aragon Stroke Care Programme (PAIA),12 developed from 2009 to 2014, and its 5-year outcomes.
We describe the key points of the strategy employed and present the outcomes.
Materials and methodsThe Aragonese health system serves the entire registered population of the region (1218342, according to 2008 data), which is divided into 8 healthcare districts, with each district having at least one general hospital. There is a neurology department at every general hospital in the network: Hospital Universitario Miguel Servet, Hospital Clínico Universitario Lozano Blesa, Hospital Royo Villanova, Hospital Ernest Lluch Martín, Hospital General San Jorge, Hospital de Barbastro, Hospital Obispo Polanco, and Hospital de Alcañiz. Furthermore, a specific department runs the 061 health emergencies telephone line, which covers the entire territory and has had an established code stroke protocol in place with both of the region's reference hospitals since 2002.
During preparation of the 2007-2011 Aragonese healthcare plan, stroke was shown to be the greatest cause of death and the second greatest cause of disability and dementia.13 This report also showed that Aragon's position had worsened relative to other autonomous communities in terms of incidence, total mortality, and, significantly, age-adjusted mortality and years of potential life lost (YPLL).
Healthcare planning in Aragon is influenced by 2 demographic characteristics: an ageing population (20.8% aged over 65; the region's population pyramid suggests that the ageing index will continue to increase) and the geographic dispersion of the population, with large areas of the territory having very low population density.14 This is a challenge for maintaining health equity, as hospitals vary greatly in terms of size and the services offered, and patient transfer times are long.
Since the programme's conception, it was decided that the PAIA should address care as a whole, connecting all links in the chain of care (integrated process management) and coordinating all healthcare resources. The programme was considered an opportunity to benefit from the growth and consolidation of healthcare information systems.
A working group (the PAIA Monitoring and Improvement Group) was created, including representatives of all neurologists and professionals involved in stroke care (Appendix 1) and regional government representatives. The group was responsible for drafting the initial programme document and for developing and monitoring the programme in the following years.
The general objective of the programme was to improve every stage of the stroke care process throughout the region of Aragon, with a view to decreasing the incidence, morbidity, and mortality of the condition and to improve survival rates and the quality of life of the people affected.
Programme development was based on the following structure:
- 1.
Initial situation analysis (2008). A report was drafted, covering:
- a)
Demographic characteristics (population ageing and dispersion) and forecasts, basic stroke epidemiology, disease burden, YPLL, admissions due to stroke (overall and by hospital), general and in-hospital mortality by stroke subtype, and average hospital stay duration.
- b)
A structural audit: technical and human resources available at each hospital, the emergency services telephone line, use and isochrone maps for code stroke (implemented in 2002), and the situations of the different hospitals’ emergency departments.
- c)
A clinical audit: care practices and procedures in the different hospitals. Data were obtained by auditing a representative sample of clinical histories from each hospital, according to size (380 cases). Audits were performed using a tool kindly provided by the Health Department of the Catalan regional government, developed for that department's Cerebrovascular Disease Master Plan, which led to the development and publication of a basic set of stroke care quality indicators based on expert consensus.15
- d)
An analysis of other strengths and weaknesses: the existence since the year 2000 of a strong, active patients’ association (the Aragon Stroke Association, with over 500 members and its own neurorehabilitation centre); the opportunity to design and develop information systems with telemedicine capabilities, unique electronic clinical histories, shared registries, nursing care modules, and electronic prescriptions; the design of indicators for data exploitation, and the region-wide implementation of a primary care case management programme, etc.
- 2.
Integrated process management. A multidisciplinary working group (Appendix 1) was created, with responsibility for:
- a)
Describing a process of comprehensive, integrated care, to be delivered by a multidisciplinary team and based on well-established guidelines and protocols and professionals’ expertise.
- b)
Setting quality targets, based on the expectations of hospital departments and the scientific/technical quality criteria defined. Formulating these targets as care quality indicators and establishing standards and objectives to be met.
- c)
Establishing a stroke care process team in each health district and hospital, to be led by the neurologist representing the centre on the PAIA Monitoring and Improvement Group and to include a representative of hospital management. Process teams are appointed by the management of each hospital and include all specialists involved in the chain of care. As a minimum, these teams must include representatives of: emergency departments, nursing staff, rehabilitation departments, primary care centres, and the emergency services telephone line. Teams from larger centres with stroke units include representatives of: primary care centres; the 061 line; hospitals’ emergency, neuroradiology, neurointervention, rehabilitation, cardiology, and vascular surgery departments; intensive care units; nursing staff; rehabilitation centres; and hospital management. Neurologists are responsible for running these teams and for giving annual reports with updates on issues identified, areas for improvement, and progress in programme implementation.
- 3.
Effective involvement of regional government, acting in the threefold capacity of legislature, executive, and supervisory body:
- a)
Coordinating resources and reference areas: establishing needs by area, referral criteria, referral between centres; enabling specialised training, etc.
- b)
Ensuring these commitments are reflected in the agendas of district managers, hospital directors, and healthcare professionals by including them in the programme contract and linking them to annual bonuses.
- c)
Committing as a government to convene meetings of the PAIA Monitoring and Improvement Group at least twice annually, and to produce: i) an annual report for the programme, covering the progress made and the health outcomes, and setting new objectives; and ii) a biennial audit with identical scope to the initial audit, enabling monitoring of improvements in the established care quality indicators.5
- d)
Committing as an administration to facilitate the use of the established information and data monitoring systems (exploitation of hospitalisation and mortality data from the minimum basic dataset; technical support for telestroke; electronic clinical histories with data recorded by emergency departments, the 061 service, and at hospitalisation, etc.; the availability of data on scales, protocols, and consent on each hospital's intranet; etc.).
- 4.
Commitment of one neurologist per health district and hospital to coordinate the work of the Stroke Care Process Team, leading the team and liaising with regional government and the PAIA Monitoring and Improvement Group.
We present the review of 5-year outcomes of PAIA implementation. Implementation of the programme has been very unequal between health districts, possibly due to differences in terms of support from each hospital's director/management and the motivation of the local process team. However, stroke care has improved significantly in all areas. The most significant changes can be summarised under 3 headings:
- 1.
Changing mentalities: proactive attitudes and clinical management
- 2.
Process outcomes
- 3.
Health outcomes
Changing mentalities regarding approaches to stroke care has been key to achieving real structural change and reorganisation of resources. However, we have also seen the importance of collaboration between management and clinicians, which has led to real changes for the health of our population.
Three main actors are involved in this new vision and increased awareness of the importance of CVDs:
- •
Firstly, government, represented by the Aragonese regional government's Department of Health and Consumer Affairs, recognised stroke as a legitimate public health issue. In 2008, 45.3% of patients with stroke in the region died, with CVDs representing the leading cause of death in women and the second most frequent in men.13 The Department of Health's involvement was a fundamental impetus for the development of the programme, with stroke being included as a priority in the 2007-2011 Healthcare Plan. This impetus, putting stroke on the political agenda, was made possible by the development of the 2008 National Stroke Plan,1 which led the Department's General Directorate for Planning and Assurance to resolve to create a stroke care programme which would include proposals made by health professionals.
- •
Secondly, all health professionals providing stroke care, particularly neurologists, were involved. Clinicians must become actors, rather than passive observers or victims of political decision-making. Neurologists have thus assumed the role of “disease managers,” being acknowledged by government and the media as local stroke experts and essential partners. Another essential change has been in the role of nurses, with the recognition of their importance and the need for specialised training. It was also important to address primary care professionals’ understanding of stroke, moving from the idea of “an unavoidable, untreatable accident” towards considering stroke both an emergency in which much can be done and a disease that can be prevented. Efforts were made in all health districts to raise awareness of the idea that “time is brain”; however, this task is far from complete, as reflected by hospital arrival times.
- •
Finally, these changes in mentality have taken place in society. Efforts were made to raise awareness of stroke through health campaigns, media presence, and the involvement of patients’ associations (particularly the Aragon Stroke Association and the Aragon Anticoagulated Patients’ Association). This helps to ensure that people are informed, take more responsibility over their health, and are more demanding of government to provide sufficient resources and work towards health equity across the region.
In 2009, the Monitoring and Improvement Group drafted and published the PAIA, detailing all subprocesses requiring action, the reorganisation of resources, and indicators for evaluation of the programme. The programme was updated in 201212 and is under review for a 2015 edition, which will include new developments, particularly regarding neurointervention (Fig. 1).
The fundamental elements of the programme are equity and sustainability of care, and the creation of a stroke care process team in each health district. The programme commits to a networked approach, resource sharing, and continuous, transparent documentation and evaluation.
Each health district's stroke care process team, led by a neurologist, is responsible for adapting the care process and each professional's responsibilities to the specific local situation, and works towards the real implementation of changes to the care provided. Each hospital establishes its own needs in terms of monitoring beds, nursing staff, coordination with the emergency department, etc. These teams’ achievements vary between hospitals and health districts, as mentioned, with governmental involvement through hospital management almost always being the critical factor.
The neurologist coordinating each health district's stroke care process team represents it at the PAIA Monitoring and Improvement Group, liaising with other process team representatives depending on the lines of work established each year. The technical group holds meetings to discuss progress in programme implementation, issues identified, how outcomes and issues should be raised with regional government, and what direction future action should take.
Audits are carried out biennially to evaluate the development and progression of the processes implemented. Annual updates are issued on organisational improvements, programme activity, in-hospital mortality, the percentage of patients receiving fibrinolysis, door-to-needle times, mean hospital stay duration, and patients’ modified Rankin Scale scores at 3 months. The audit reviewed the same indicators as the Catalan Cerebrovascular Disease Master Plan audit; these were defined by a collaborative Delphi study including researchers from 3 autonomous communities (Catalonia, the Balearic Islands, and Aragon).15
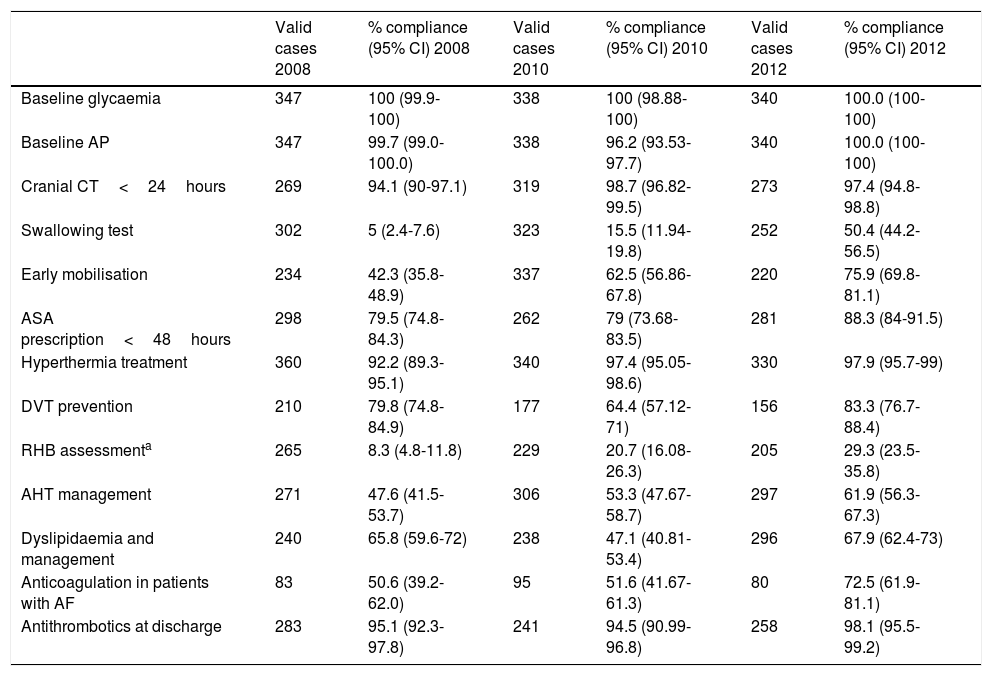
Table 1 shows findings for the main indicators (level of evidence A) in the 3 audits performed to date (2008, 2010, and 2012). The 2008 audit was performed prior to implementation of the strategy, and the other 2 were performed subsequently. A new assessment is being drafted for the 2014 data.
Top 13 outcomes. Audits conducted in 2008, 2010, and 2012.
| Valid cases 2008 | % compliance (95% CI) 2008 | Valid cases 2010 | % compliance (95% CI) 2010 | Valid cases 2012 | % compliance (95% CI) 2012 | |
|---|---|---|---|---|---|---|
| Baseline glycaemia | 347 | 100 (99.9-100) | 338 | 100 (98.88-100) | 340 | 100.0 (100-100) |
| Baseline AP | 347 | 99.7 (99.0-100.0) | 338 | 96.2 (93.53-97.7) | 340 | 100.0 (100-100) |
| Cranial CT<24hours | 269 | 94.1 (90-97.1) | 319 | 98.7 (96.82-99.5) | 273 | 97.4 (94.8-98.8) |
| Swallowing test | 302 | 5 (2.4-7.6) | 323 | 15.5 (11.94-19.8) | 252 | 50.4 (44.2-56.5) |
| Early mobilisation | 234 | 42.3 (35.8-48.9) | 337 | 62.5 (56.86-67.8) | 220 | 75.9 (69.8-81.1) |
| ASA prescription<48hours | 298 | 79.5 (74.8-84.3) | 262 | 79 (73.68-83.5) | 281 | 88.3 (84-91.5) |
| Hyperthermia treatment | 360 | 92.2 (89.3-95.1) | 340 | 97.4 (95.05-98.6) | 330 | 97.9 (95.7-99) |
| DVT prevention | 210 | 79.8 (74.8-84.9) | 177 | 64.4 (57.12-71) | 156 | 83.3 (76.7-88.4) |
| RHB assessmenta | 265 | 8.3 (4.8-11.8) | 229 | 20.7 (16.08-26.3) | 205 | 29.3 (23.5-35.8) |
| AHT management | 271 | 47.6 (41.5-53.7) | 306 | 53.3 (47.67-58.7) | 297 | 61.9 (56.3-67.3) |
| Dyslipidaemia and management | 240 | 65.8 (59.6-72) | 238 | 47.1 (40.81-53.4) | 296 | 67.9 (62.4-73) |
| Anticoagulation in patients with AF | 83 | 50.6 (39.2-62.0) | 95 | 51.6 (41.67-61.3) | 80 | 72.5 (61.9-81.1) |
| Antithrombotics at discharge | 283 | 95.1 (92.3-97.8) | 241 | 94.5 (90.99-96.8) | 258 | 98.1 (95.5-99.2) |
The most noteworthy actions among the process outcomes achieved in Aragon are:
- -
Comprehensive stroke management
- -
Creation of stroke units/areas
- -
Nurses trained to care for patients with stroke
- -
Implementation of intravenous fibrinolysis in all hospitals, with or without telestroke
- -
Development of neurosonology in all hospitals
- -
Coordination with primary care centres
- -
More efficient use of resources
- -
Coordination with rehabilitation centres
- -
District and whole-region care protocols based on medical evidence and clinical practice guidelines
- -
The ability to compare results and regularly and transparently share documentation and good practices (benchmarking)
- -
Consensus criteria for action and normalisation of interconsultation
- -
Networked organisation: telestroke, neurology and neurosurgery telephone consultations, standardised electronic clinical history, established referrals
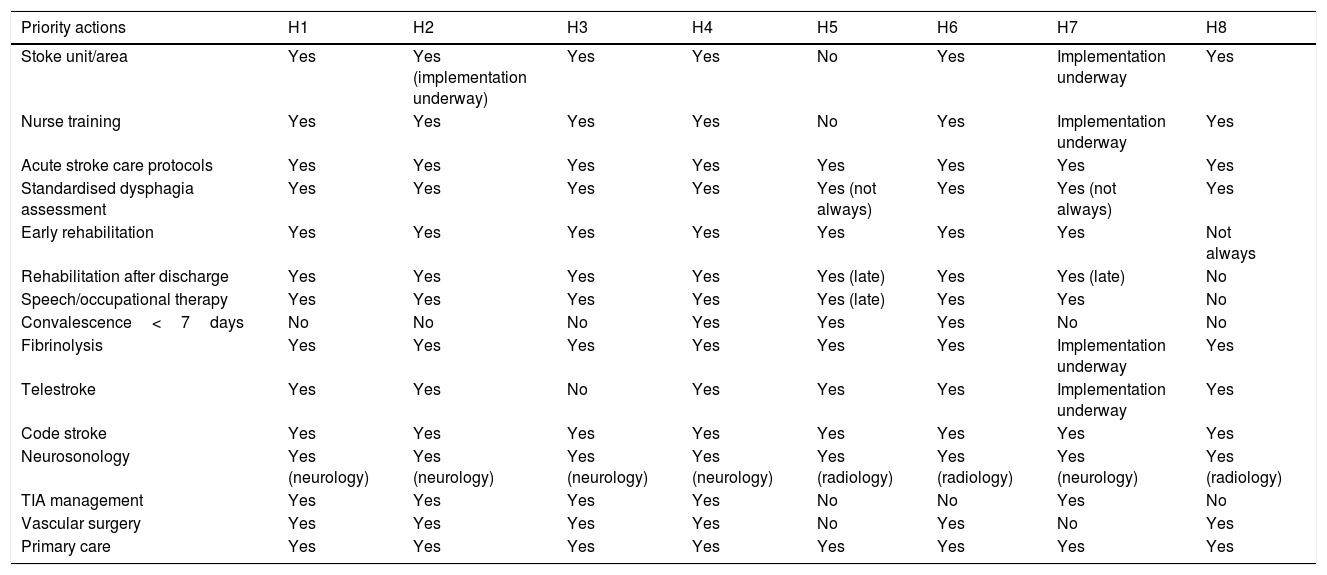
Table 2 shows the main results by health district.
Status of the main objectives in the different health districts at 31 December 2014.
| Priority actions | H1 | H2 | H3 | H4 | H5 | H6 | H7 | H8 |
|---|---|---|---|---|---|---|---|---|
| Stoke unit/area | Yes | Yes (implementation underway) | Yes | Yes | No | Yes | Implementation underway | Yes |
| Nurse training | Yes | Yes | Yes | Yes | No | Yes | Implementation underway | Yes |
| Acute stroke care protocols | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Standardised dysphagia assessment | Yes | Yes | Yes | Yes | Yes (not always) | Yes | Yes (not always) | Yes |
| Early rehabilitation | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Not always |
| Rehabilitation after discharge | Yes | Yes | Yes | Yes | Yes (late) | Yes | Yes (late) | No |
| Speech/occupational therapy | Yes | Yes | Yes | Yes | Yes (late) | Yes | Yes | No |
| Convalescence<7days | No | No | No | Yes | Yes | Yes | No | No |
| Fibrinolysis | Yes | Yes | Yes | Yes | Yes | Yes | Implementation underway | Yes |
| Telestroke | Yes | Yes | No | Yes | Yes | Yes | Implementation underway | Yes |
| Code stroke | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Neurosonology | Yes (neurology) | Yes (neurology) | Yes (neurology) | Yes (neurology) | Yes (radiology) | Yes (radiology) | Yes (neurology) | Yes (radiology) |
| TIA management | Yes | Yes | Yes | Yes | No | No | Yes | No |
| Vascular surgery | Yes | Yes | Yes | Yes | No | Yes | No | Yes |
| Primary care | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
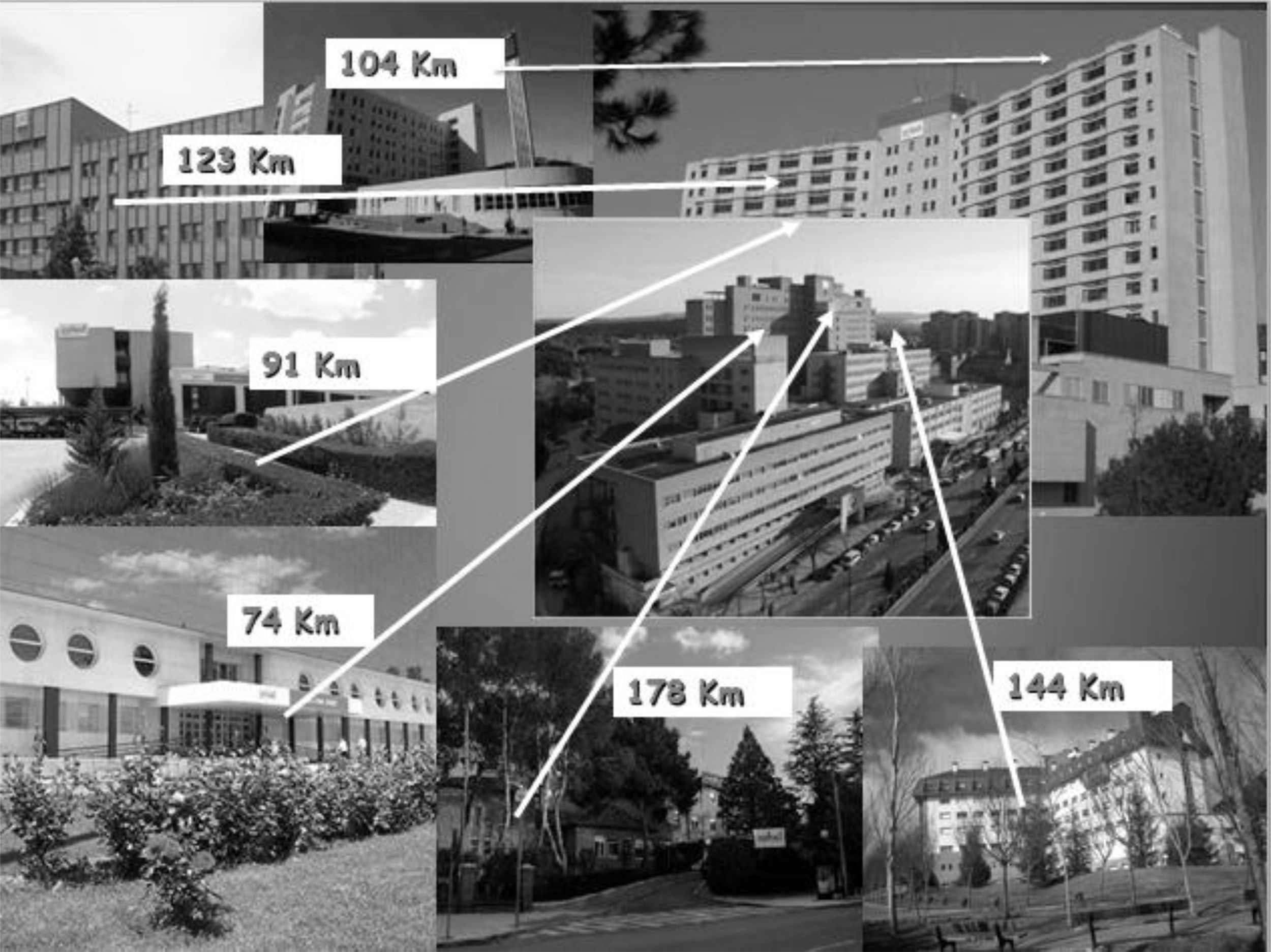
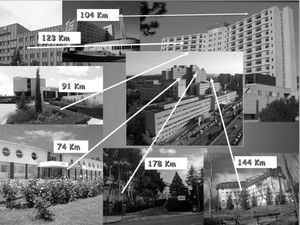
In early 2008, Aragon had a population of 1 326 918, of whom 66% lived in the municipality of Zaragoza, 146 324 in the province of Teruel, 225 271 in Huesca, and the rest of the population in the province of Zaragoza, with certain population groups located far from the city, in mountainous regions. Due to this population distribution, most resources are concentrated in the province of Zaragoza, meaning that there is almost no access to specialised care (such as stroke units and such specialised treatments as fibrinolysis) in the provinces of Huesca and Teruel (Fig. 2).
Given the importance of treating all patients with stroke in units with trained nurses, monitoring, and established care and assessment protocols, it was a priority to make this type of care available for all patients in all hospitals. Through the creation of stroke areas, defined as “specific inpatient areas with monitored beds, specific care protocols, and specially trained nurses,” PAIA resolves the problem of access to acute stroke care at primary- and secondary-level hospitals. While stroke units/areas were only available for 30% of the population in 2008, by 2014 they had expanded to cover 78% of the population. The creation of stroke areas has represented a substantial change in patient care, considerably reducing mortality in hospitals where they have been introduced. Hospitals that have stroke areas with specialised nurses had an in-hospital stroke mortality rate of 8%-11%, compared to 16%-18% in hospitals without these units/areas. This is reflected in the rate of in-hospital mortality due to CVD in the region; until 2010, it represented 18% of all in-hospital deaths, decreasing to 13.7% by 2014.16
In 2008, only the region's 2 tertiary-level hospitals offered fibrinolytic therapy. The introduction of telestroke was essential due to 2 issues which hindered universal access to fibrinolysis:
- -
Hospitals serving the population outside Zaragoza are small (<200 beds) or medium (<400) in size and lack on-call neurology services.
- -
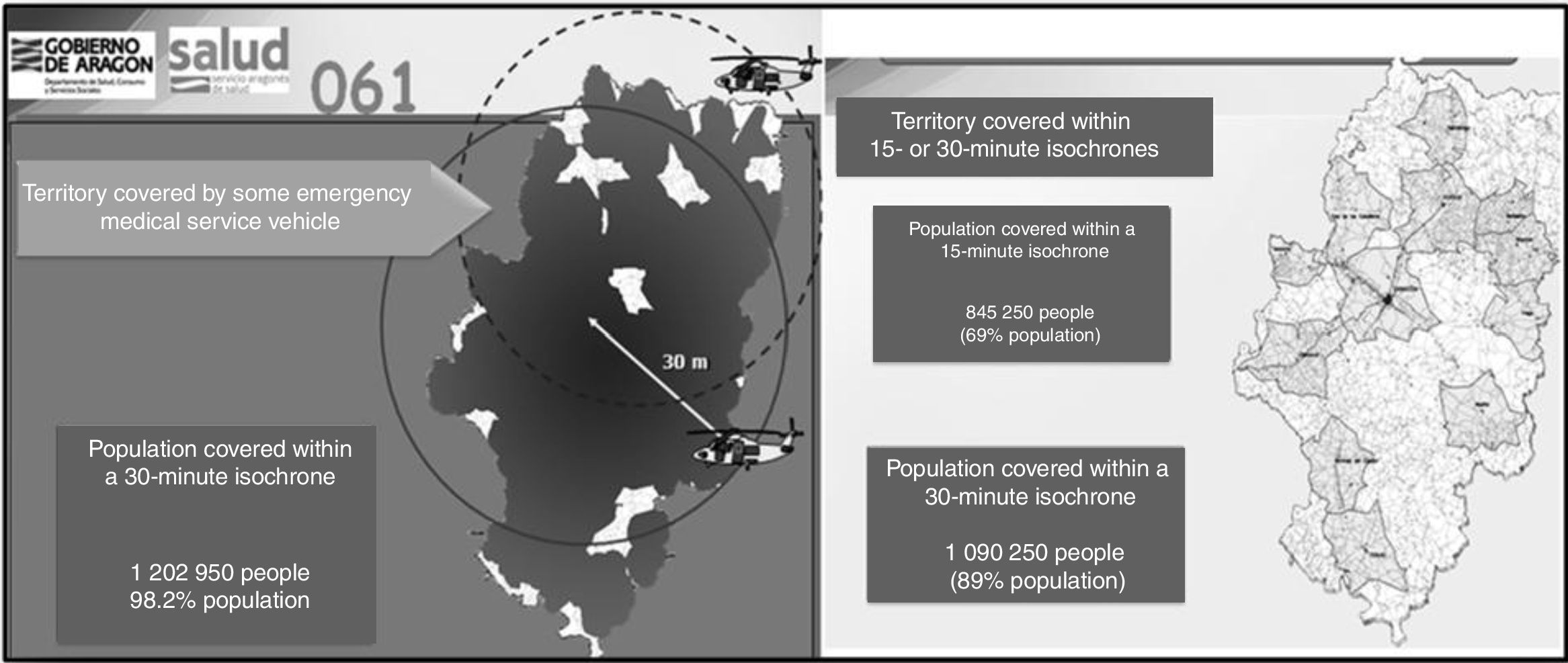
Aragon's size and rugged terrain result in long patient transfer times. Although ambulances from Aragon's emergency services achieve acceptable isochrones for transport to the first hospital (the <15minutes isochrone covers 69% of the population, <30minutes 89%, and the 2 helicopter ambulances cover 98.2% of the population), half of the population cannot be transported to a tertiary hospital in under 45minutes in real-life conditions. Furthermore, the air ambulances do not fly at night or in unfavourable weather conditions, which in mountainous areas makes it difficult to reach these patients, for whom time is a critical factor. Furthermore, both our experience and the literature show that 80% of patients transferred by helicopter following code stroke activation are ultimately not eligible for fibrinolytic therapy.17 Helicopters dispatched over 90minutes after onset of symptoms and having to cover an average distance of 95km are unable to arrive at hospital in time for treatment.
Introducing stroke telemedicine as a tool to sustainably establish equity was essential in achieving universal access to fibrinolytic therapy.
All hospitals in the Health Service of Aragon are connected by a specialised, high-availability health information network with sufficient bandwidth to meet the needs of the telestroke system (FO Gigabit, 2×100MBps). Since 2011, all hospital intranets have been interconnected, with each patient assigned a unique identity number. This enables clinical histories to be accessed between centres, as well as online interconsultations with records of the professionals issuing and responding to the request.
The Aragon telestroke service uses this interconsultation application and the ability to display DICOM-format medical images in real time to view computed tomography (CT) imagery. Combined with videoconference software (Spontania, by Dialcom Networks), the application enables multi-participant video calls to be made from any computer for examination of the patient and interaction with the emergency department at the peripheral hospital. These computers require very basic hardware (a webcam, a microphone, and speakers), with an approximate cost of €300. Since December 2013, the application has used a single-screen view incorporating neuroimaging, the videoconference, and a written report of the closure of the teleconsultation with an electronic signature.
The implementation of telestroke in 2011 made fibrinolysis available generally, with coverage increasing from 55% of the population in 2008 to 94% in 2014. In addition to the increased number of patients receiving fibrinolysis (details discussed later in the article), this has led to more efficient resource use, progressively decreasing the number of helicopter dispatches due to code stroke activation and unnecessary transfers of neurosurgery patients. In 2010 and 2011, helicopters were dispatched 20 and 21 times, respectively; this figure fell to 14 in 2012, 10 in 2013, and 4 in 2014 (including 2 in the Alcañiz area, the only district where telestroke is yet to be implemented).
Health outcomesThe changes observed in stroke care in our region over the past 4 years are reflected in the health outcomes. The most significant observations are the following:
Over the 2007-2012 period, the rate of hospitalisation due to stroke stayed between 2.46 and 2.32 per 1000 population, with little change. Beginning in 2013, a decrease was observed in the hospitalisation rate (2013: 2.07; 2014: 2.19).
Code stroke was introduced in the region's 125 basic health areas (100% of centres). A mean of 203 annual code stroke activations were registered by the emergency services telephone line (range, 159-226); 79% of these patients arrived at hospital within 3hours of symptom onset. Mean time between code stroke activation and arrival at hospital was 75.7minutes (range, 68.2-80.9).
The introduction of telestroke led to the expansion of fibrinolytic therapy into small- and medium-sized hospitals, leading to increased rates of patients receiving fibrinolysis. Therefore, while only 4.4% of stroke patients treated in Aragon received this treatment in 2010, this figure has risen as the technology has been introduced in other health districts, with 6.4% of patients receiving fibrinolysis in 2011, 6.6% in 2012, 8.09% in 2013, and 8.6% in 2014. In 2014, intravenous fibrinolysis was performed 125 times and 6 patients received neurointervention. Half of the fibrinolytic procedures (62) were performed at Hospital Universitario Miguel Servet (HUMS), 36 were performed at Hospital Clínico Universitario Lozano-Blesa, and 37 (29.6%) were performed at small- and medium-sized hospitals; 11 of these procedures were performed using telestroke.
Treatment took place within 3hours of symptom onset in 82% of cases, with a mean door-to-needle time of 77minutes (73minutes in the period 2008-2013). Around 4.1% of the patients receiving fibrinolysis died, and 5.5% displayed symptomatic haemorrhages within 36hours.
The percentage of patients receiving fibrinolysis outside the region's 2 tertiary hospitals increased from 12.5% in 2011 to nearly 30% in 2014. The telestroke service was used in 9% of all fibrinolytic procedures performed in this period.
Telestroke prevented 56% of non-indicated patient transfers, with fibrinolysis performed in 44% of cases, and led to a decrease in the number of helicopters dispatched due to code stroke activation, as described above.
Telestroke consultation was always with HUMS staff. These consultations occurred between 15:00 and 03:00 in 88% of cases, and on mornings of public holidays in 12% of cases.
Neurointervention was performed in only a small number of cases (2 in 2013 and 6 in 2014) at only one centre (HUMS), whose on-call neurointervention service is not available 24hours per day. An objective for 2015 is to consolidate the on-call service and to implement the necessary changes to increase the number of neurointervention procedures (primary, rescue, and unknown time). All centres were supplied with the equipment necessary to perform multimodal CT scans (CT-angiography and CT-perfusion).
All actions (Table 2) address one of the programme's main objectives: decreasing stroke mortality and morbidity.
The 2008 audit, conducted prior to the implementation of the strategy, observed an in-hospital mortality rate of 17%. This decreased to 14% in 2011, 12.5% in 2012, and 12.8% in 2013, rising to 13.7% in 2014 due to certain hospitals either not having introduced basic measures such as stroke areas, or experiencing staffing issues due to the economic situation in the last 2 years of the study period (Fig. 3).
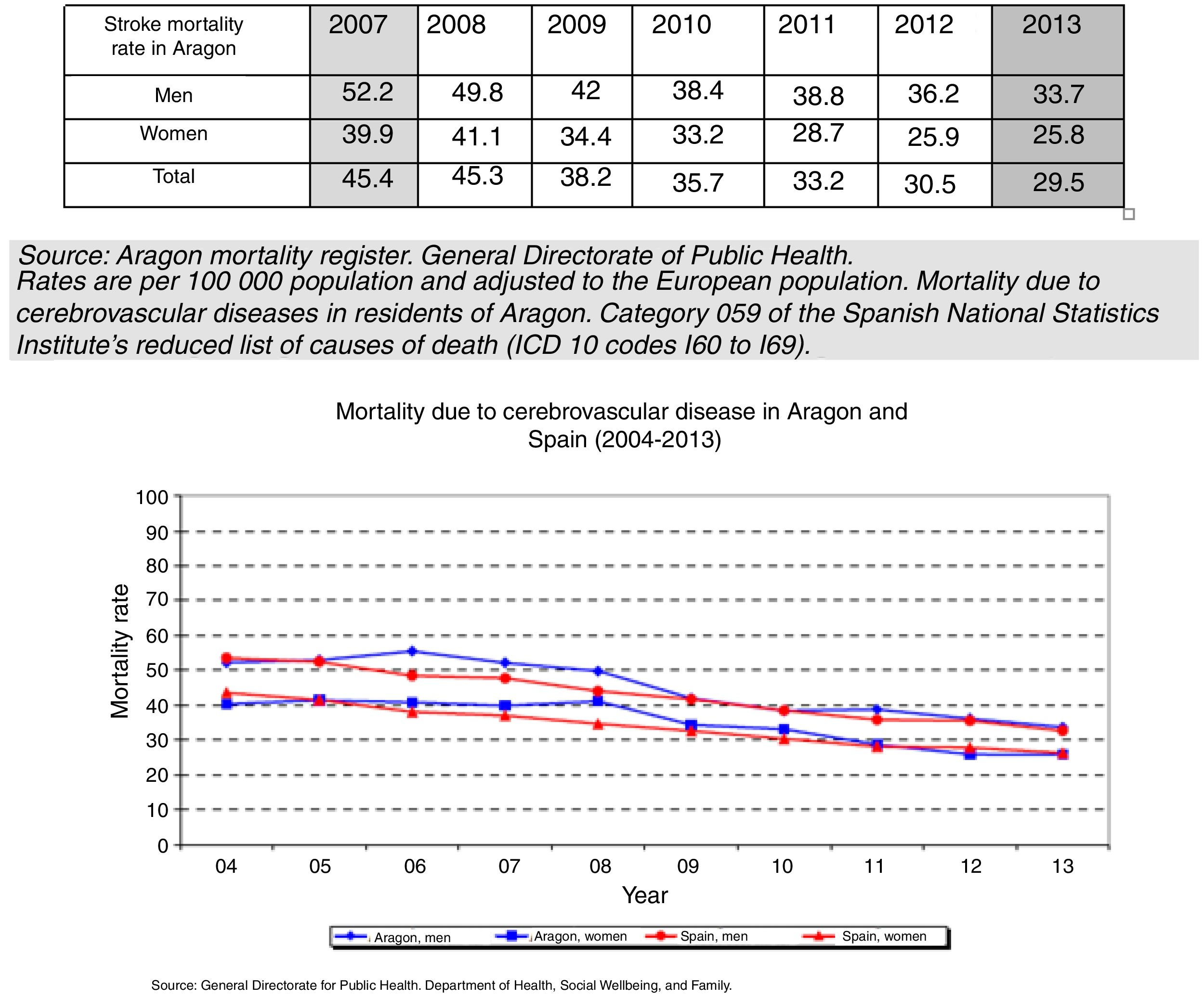
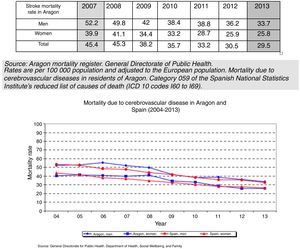
Although stroke continues to be the leading cause of death in women (9.1% of all deaths) and the second greatest in men in Aragon, CVD mortality has decreased by 36% in the last 10 years; this decrease has been much more rapid since the launch of PAIA (34.9% from 2008 to 2013), in both men and women (Fig. 4). The sex ratio in Aragon is 1.3 males per female. The mortality rates observed in our region are converging with national averages for both sexes; this represents an improvement in Aragon's relative position as a region (Fig. 4).
Life expectancy in Aragon was 83.2 years in 2013 (82.8 years in Spain as a whole). YPLL is an excellent indicator for identifying causes of premature mortality. The adjusted rate of YPLL due to CVD (the ninth greatest cause of YPLL in the region) in 2013 was 67.7 per 100000 population: 85.4 in men and 45.5 in women. This represents a significant decrease from the 2008 figures: 174 in men and 114 in women.18
DiscussionStroke care has improved significantly in the region thanks to the introduction of a treatment protocol and specific stroke areas (or units) for acute care, and the implementation of code stroke in all health areas. This has led to better health outcomes, with decreases in mortality and YPLL due to stroke.
The implementation of PAIA was fundamental to restructuring resources and developing and maintaining different lines of work through the Monitoring and Improvement Group, which includes neurologists representing each health district. The group establishes priorities and incorporates new scientific evidence, aiming to align itself with government independently of any political changes that may occur.
The inclusion of annual and biennial audits enabled us to analyse the programme's development, to identify critical and priority measures, and to identify issues in each district, in order to address these either locally or through the regional health service's planning department. The networked approach adopted also enabled care and referral protocols to be drafted for the region of Aragon as a whole, preventing differences between each health district's protocols and improving the uniformity of the care provided.
As shown in Table 2, the majority of priority programme actions have been developed and launched in each health district. Nonetheless, acute care implementation and nurse training continue to be a challenge in some districts. It is interesting to note that an absence of stroke areas with specialised nursing staff is associated with higher mortality rates than in districts that do have these resources in place. The majority of the issues hindering implementation are due to the economic situation, and particularly to a lack of leadership on the part of some hospital directors. In these cases, the PAIA Monitoring and Improvement Group is required to explain these issues and the lack of equity between health districts to government representatives.
Table 2 also shows some outstanding actions that do not require financial commitments and are easily implemented, such as the introduction of a clinical pathway for transient ischaemic attack. These actions have been set as outstanding objectives by the health districts that have yet to implement them.
Fibrinolysis has been one of the major achievements of PAIA, more in terms of the level of availability achieved than the number of procedures performed. The introduction of telemedicine has resulted not only in use of the technique, but also in a need for organisational and training efforts at all hospitals treating patients with stroke, the creation of stroke areas, and the organisation of interhospital patient transfers. These were the 4 key elements for success identified in the TEMPiS project, a programme implemented in the German region of Bavaria.19 The authors of that study note that improved understanding of stroke in local hospitals was associated with better overall care. In our experience, care quality improvements result from several actions (protocol reviews, training of nurses and emergency department staff, etc.), with telestroke interconsultation being a significant factor.
The record of teleconsultations shows that code stroke activation via the telestroke service mainly took place in non-working hours; code stroke activations occurring between 08:00 and 15:00 were managed by local neurologists. This led all health districts to reorganise care protocols in order to treat patients for whom code stroke was activated within working hours, avoiding unnecessary burdens on tertiary hospitals. Of all cases of fibrinolysis performed outside the 2 tertiary hospitals (30%), this treatment was performed via telestroke in 9% of cases and by local neurologists in 20%; this led to a twofold increase in the percentage of patients receiving fibrinolysis between 2010 and 2014 (4.4% and 8.6% of patients, respectively).
As the findings show, telestroke is a safe, efficient tool that reduces costs and improves the use of health resources.20 Furthermore, it prevented unnecessary transport of patients on 56% of occasions; this type of transport can disturb the patient and forces the family to travel long distances. Ribó and Álvarez-Sabín21 report that prior to telestroke implementation, 50% of patient transfers were unnecessary; after the service was implemented this figure fell to 20%.
The number of helicopters dispatched due to code stroke activation also fell by 80%. This not only represents a cost saving, but also allows the vehicles to be used for other emergencies, in a region equipped with only 2 air ambulances.
According to data from the Spanish Health Ministry's stroke strategy assessment, hospitalisation rates in Aragon are higher than the national average (mean hospitalisation rate of 1.86 in Spain vs 2.26 in Aragon in 2010), despite a decrease over the past 2 years.22 This is probably due to the higher average age of the Aragonese population compared to the Spanish population as a whole, and the resulting increased risk of CVD.
In-hospital mortality rates have significantly decreased (by around 25%) in recent years. The latest data (from 2014) reveal an in-hospital mortality rate of 13.7%. National mortality statistics from 2011 (Spanish National Statistics Institute, minimum basic dataset, ICD codes 430-438) show an in-hospital mortality rate of 12% (12.49% in 2009).23 Despite mortality being above the national average, there has been a marked downward trend in acute mortality in the region in recent years, particularly in health districts which have created stroke areas. This lends strength to our demand that regional government enable quality care to be provided in all health districts.
The decrease in acute mortality represents a significant decrease in overall mortality due to CVDs in the region (34.9% since the programme was implemented), as well as a decrease in premature mortality (measured in YPLL) of 50% in men and 68% in women.
Finally, neurointervention is unavailable in many hospitals in the region. Regional government has been reluctant to grant funding for this as the technique had not been clearly demonstrated to be efficacious prior to 2014. Since the publication in the last year of studies demonstrating the technique's efficacy, the technical group's most pressing objective, after the introduction of multimodal CT scanning in all hospitals, is the orderly, regulated introduction of neurointervention.
To conclude, despite the future challenges ahead, PAIA is a cost-efficient tool for improving stroke care. The positive health outcomes achieved in the population demonstrate the effectiveness of clinical practice based on clinical management, a networked approach, and continuous improvement.
Conflicts of interestThe authors have no conflicts of interest to declare.
PAIA coordinators:
Javier Marta Moreno, 2008-2012; María Bestué Cardiel, 2012-2015.
Neurologists (coordinators of their hospitals’ stroke care process teams):
Juan Ignacio López Gastón, Department of Neurology, Hospital Universitario Miguel Servet, Zaragoza.
Enrique Mostacero Miguel and Cristina Pérez Lázaro, Department of Neurology, Hospital Clínico Universitario Lozano-Blesa, Zaragoza.
Olalla Alberti González, Department of Neurology, Hospital San Jorge, Huesca.
Isabel Campello Morer and Álvaro Giménez, Department of Neurology, Hospital Royo Villanova, Zaragoza.
María José Borruel Aguilar, Emergency Department, Hospital General, Teruel.
José Antonio Oliván Usieto, Department of Neurology, Hospital de Alcañiz, Alcañiz.
José María Errea, Department of Neurology, Hospital de Barbastro, Barbastro.
Marta Samperiz Murillo, 061 Emergency Services director for the Aragon Stroke Programme.
María José García Gomara and Marta Palacín, Hospital de Calatayud, Calatayud.
Biennial audit coordinators: Álvaro Giménez and Marta Palacín.
Other group members (non-neurologists):
Javier Marzo (2008-2011) and Olga Martínez, Head of Programmes, General Directorate for Planning and Assurance, Department of Health, Regional Government of Aragon.
Julián Urralburu (2008-2010) and Adoración Felez, Health Service of Aragon.
Rafael Marrón, Information Systems representative of the Health Service of Aragon.
María Jesús Chopo Alcubilla, representative of nursing departments.
Belén Gros, representative of reference hospital emergency departments.
María José Borruel, representative of non-reference hospital emergency departments.
Marta Samperiz, representative of 061 Emergency Services. Non-hospital code stroke.
Pilar Reigada, representative of reference hospital rehabilitation and physical medicine departments.
Miguel Arranz, representative of non-reference hospital rehabilitation and physical medicine departments.
Ana Coarasa, representative of rehabilitation centres.
Inés Sauras, representative of primary care centres.
Group members are listed in Appendix 1.
Please cite this article as: Marta Moreno J, Bestué Cardiel M, Giménez Muñoz A, Palacín Larroy M, Grupo de Seguimiento y Mejora del Programa de Atención al Ictus en Aragón (PAIA). Programa de Atención al Ictus en Aragón (PAIA). Estrategia del cambio y resultados en el periodo 2009-2014. Neurología. 2018;33:301–312.
This study was presented in part as an oral communication at the 65th Annual Meeting of the Spanish Society of Neurology in 2013 and at the 12th Healthcare Costs Management and Evaluation Conference (SIGNO Foundation) in 2014.