Migraine is a common and prevalent disease that contributes to health expenditure and interferes with quality of life. Our goal was to analyse the level of stress at work in a sample of migraine and its possible association with the chronicity of the process.
Materials and methodsWe applied the Maslach Burnout Inventory (MBI), consisting of 22 items grouped into blocks that assess emotional exhaustion (EE), personal accomplishment (PA), depersonalisation at work (DP) and positive influence (PI), to 94 consecutive subjects recruited in the outpatient clinic. Differences were compared between clinical groups (chronic migraine [CM]: >15days/month with headache over a 3-month period vs episodic migraine [EM]: <15days/month with headache) using the general linear model adjusted for age and MIDAS score.
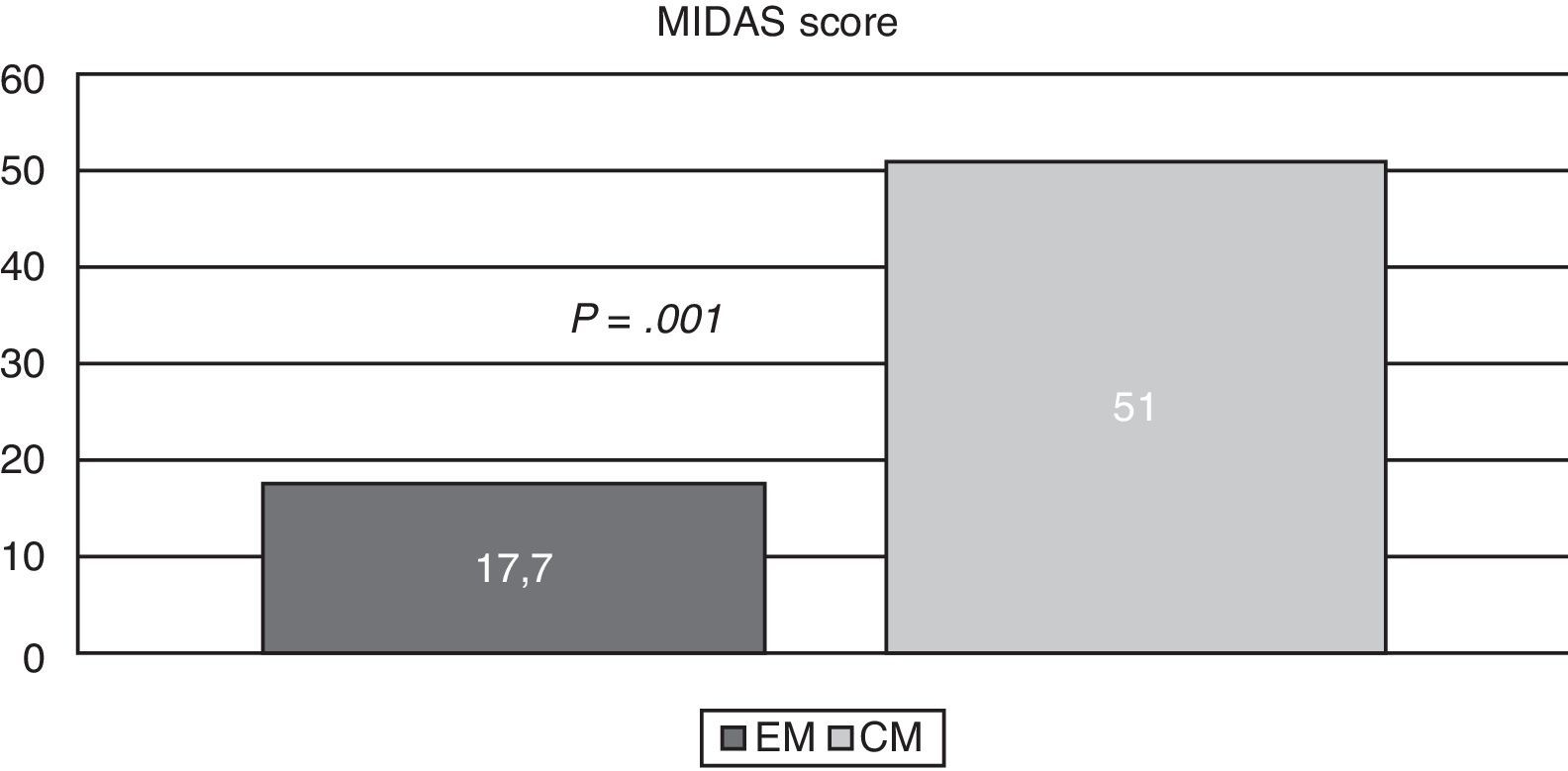
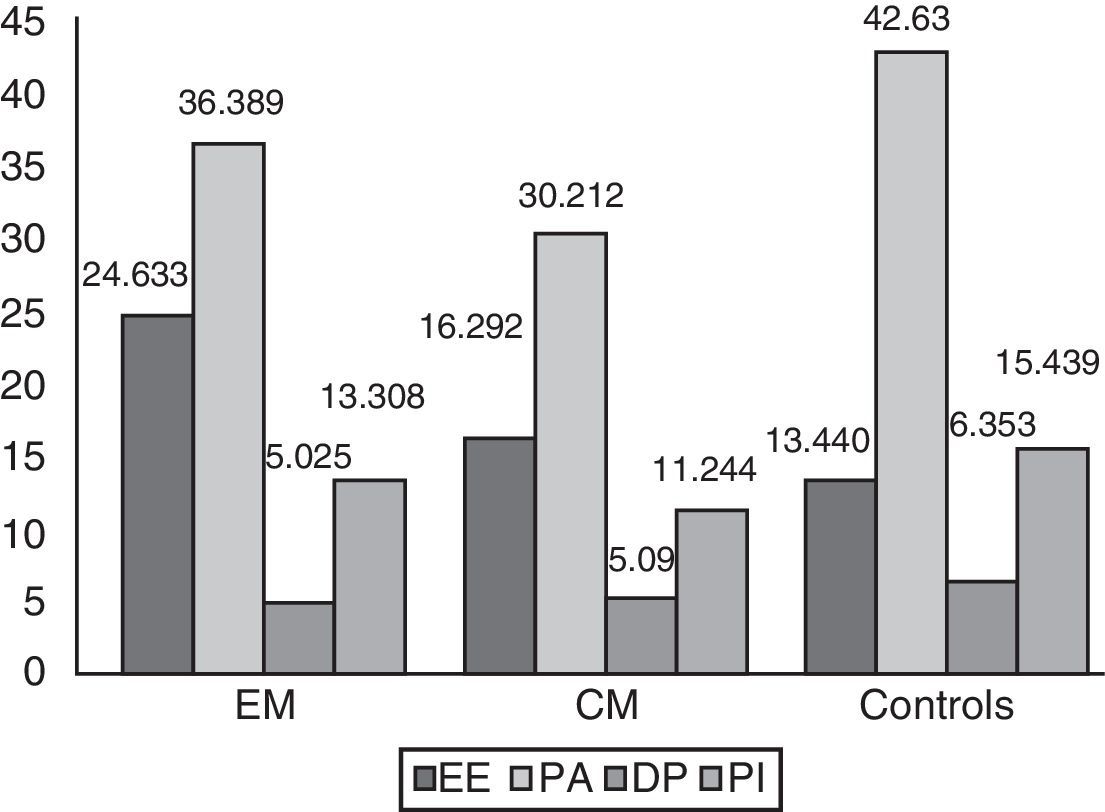
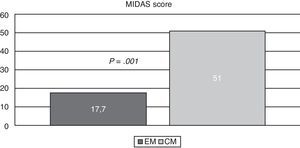
ResultsThe mean age was higher in the CM group. Mean MIDAS scores were 51±4.1 in CM, and 17.7±15 in EM (P=0.001). Adjusted means for EE were 24.6±2.6 in CM patients, 16.2±2.6 in EM patients, and 13.4±2.3 (P=0.03) in the healthy group. MIDAS scale scores were inversely correlated to PA (P<0.05).
DiscussionOur results suggest that the level of EE at work is higher in EM than in CM patients, while PA levels decrease as impact on the MIDAS scale increases. The Maslach scale is a potentially useful tool for studying migraine impact. Surprisingly, EE is higher in patients with fewer episodes; this tendency could be related to stress adaptation mechanisms present in patients with chronic illness.
La migraña es un trastorno común y prevalente que contribuye considerablemente al gasto sanitario e interfiere en la calidad de vida de los pacientes. Nuestro objetivo fue explorar el nivel de estrés en el trabajo en una muestra de migrañosos y su posible asociación con la cronicidad del proceso.
Material y métodosSe aplicó el test de Maslach («burnout inventory»: 22 ítems agrupados en bloques que valoran: agotamiento emocional [AE], realización personal [RP], despersonalización en el trabajo [DP]) e influencia positiva (IP) a 94 sujetos consecutivos reclutados en consultas. Las diferencias se compararon entre grupos clínicos (migraña crónica [MC] —más de 15 días/mes de cefalea/3 meses— vs. migraña episódica [ME] —< 15 días/mes—) mediante el modelo lineal general ajustado por edad y MIDAS.
ResultadosLa edad media fue superior en MC. Las puntuaciones medias en la escala MIDAS fueron 51±4,1 en MC y 17,7±15 en ME (p=0,001). La media ajustada de AE fue en ME 24,6±2,6, en MC 16,2±2,6 y en controles 13,4±2,3 (p=0,03). La escala MIDAS se correlacionó inversamente con RP (p<0,05).
DiscusiónNuestros resultados señalan que el nivel de AE es mayor en ME que en MC; mientras la RP es peor cuanto mayor impacto tiene la migraña según escala MIDAS. La escala Maslach es una herramienta potencialmente útil en el estudio de las repercusiones de la migraña. Sorprendentemente, el AE es mayor en pacientes con menos crisis, lo que podría relacionarse con mecanismos de adaptación al estrés presentes en el paciente crónico.
Migraine is a common and disabling disorder. It is one of the most frequent neurological diseases in Spain,1 where it has an estimated prevalence of 16.6% according to data from a self-administered questionnaire2 and of 11.02% according to data from the National Health Survey carried out in 2006.3 It also generates considerable expenditures for the health system; in addition to the direct costs of medication, there are the indirect costs of migraine which include missing days of work or decreased functional capacity. In light of the above, the World Health Organization recognises headache as a high-priority health problem and has ranked it 19th among causes of years of life lived with disability in both sexes and all ages, and 12th in women.4
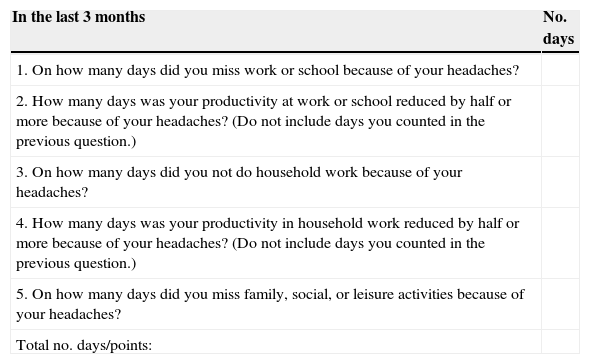
In addition to significantly contributing to healthcare expenditure, migraine interferes with quality of life. It is therefore important to be aware of its disability-creating factors that affect prognosis since this will facilitate disease management. The extent to which migraine affects daily living and the degree of disability it causes have been measured with different scales, which are becoming increasingly widespread since they are easy to use. They include the Migraine Disability Assessment Scale (MIDAS),5,6 displayed in Table 1, the Headache Impact Test (HIT),7–9 and the Beck Depression Inventory-II (BDI-II) and Beck Anxiety Inventory (BAI).10–12
MIDAS (Migraine Disability Assessment) questionnaire
| In the last 3 months | No. days |
|---|---|
| 1. On how many days did you miss work or school because of your headaches? | |
| 2. How many days was your productivity at work or school reduced by half or more because of your headaches? (Do not include days you counted in the previous question.) | |
| 3. On how many days did you not do household work because of your headaches? | |
| 4. How many days was your productivity in household work reduced by half or more because of your headaches? (Do not include days you counted in the previous question.) | |
| 5. On how many days did you miss family, social, or leisure activities because of your headaches? | |
| Total no. days/points: |
MIDAS questionnaire for assessing migraine-related disability. Scoring: 0-5: little or no disability; 6-10: mild disability; 11-20: moderate disability; >20: severe disability.
The high impact of migraine on working life cannot be measured merely in lost workdays or in healthcare costs. No studies have addressed the association between migraine and the level of stress at work. An increasingly relevant concept related to stress in the workplace is that of burnout syndrome. Burnout is a response to chronic stress at work (long-term and cumulative) which has a negative impact on both individuals and organisations. Its distinguishing features reflect specific areas of work (whether professional, voluntary, or household), especially when work involves contact with groups of users and consumers. Burnout is an indicator of emotional exhaustion (EE). Although there are multiple definitions for this syndrome, the most widely accepted one defines burnout as a response to chronic work-related stress derived from EE and negative attitudes and feelings about one's clients and work.13 Although the real incidence and prevalence of burnout are unknown, we do know that it includes 3 key traits: increased feeling of EE, negative attitude towards third parties, and a tendency to evaluate oneself negatively. As a result, burnout may cause absenteeism, low morale, and work-related problems.
The purpose of this study is to explore the influence of migraine and its severity on professional exhaustion in a sample of patients compared to a control group, in addition to studying its potential association with migraine chronicity.
Subjects, material, and methodsThis cross-sectional study recruited consecutive patients examined at the neurology outpatient clinic at Hospital Universitario Marqués de Valdecilla, in Santander, between 2010 and 2011. Participants were adults diagnosed with migraine at least 6 months prior to the study and who met the diagnostic criteria established by the International Classification of Headache Disorders, Second Edition (ICHD-2)14 and its revised 2006 version.15 Subjects were classified into 3 groups according to their clinical history and any necessary complementary tests. The first group included patients with chronic migraine (CM), defined as having headache more than 15 days per month during at least 3 months, including at least 8 migraine-like episodes not attributable to medication overuse or any other causes. Only patients with no history of medication overuse were selected. The second group consisted of patients with episodic migraine (EM), while the third group included controls, who were recruited from among patients’ companions. Inclusion criteria for controls were not having suffered headache episodes during the past year and never having experienced migraine, according to the ICDH-2 criteria. Patients in both the CM and the EM groups had been employed for at least 6 months during the year prior to the consultation.
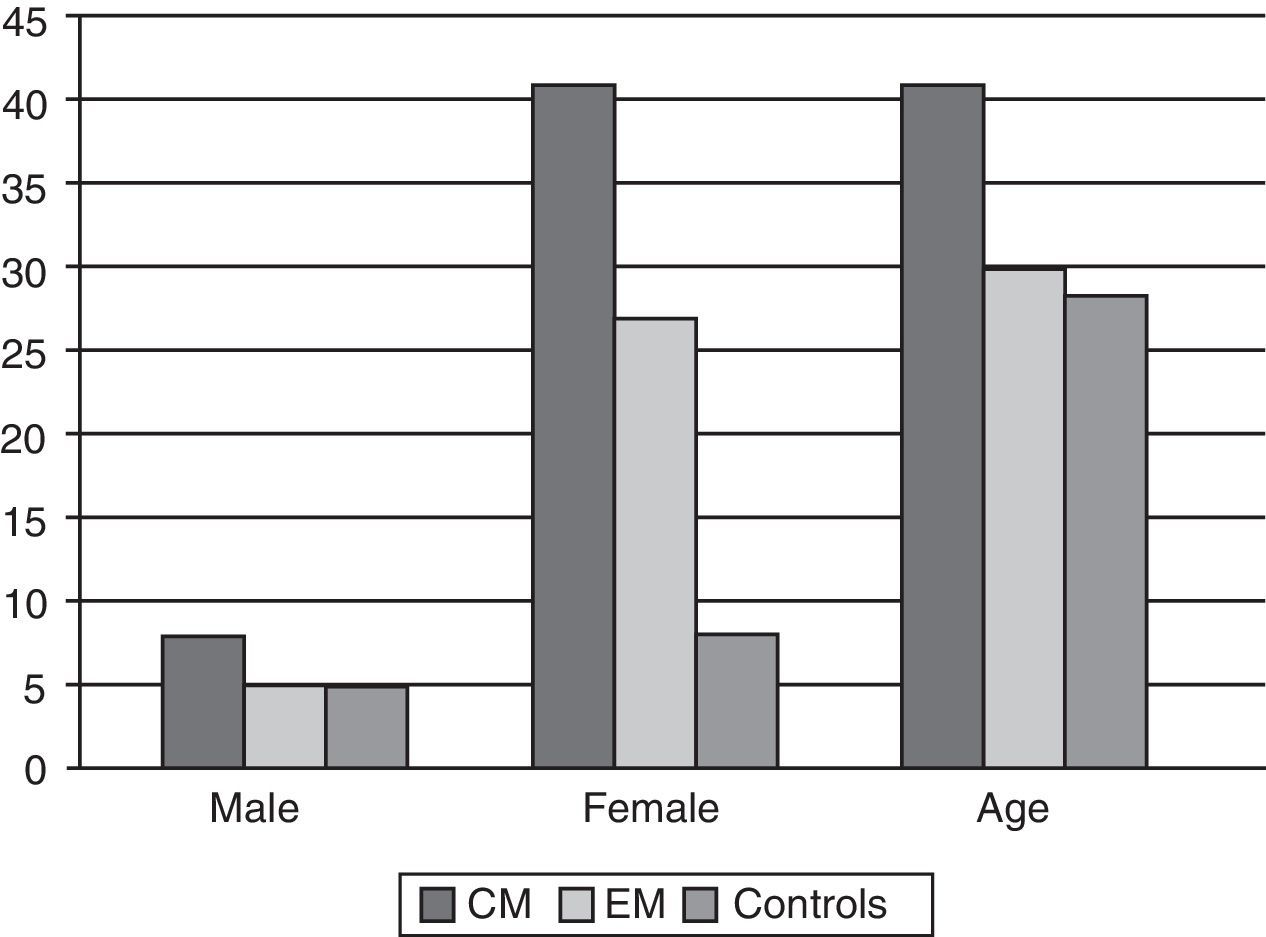
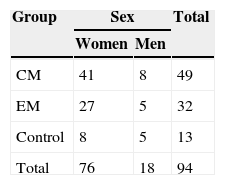
Our hypothesis was that the level of stress at work affects migraine chronicity. We included a total of 94 patients in our study: 49 of them (8 male) met inclusion criteria for CM group, 32 (5 male) had EM, and 13 patients were controls (Table 2). All participants were white. We collected demographical data, including age, sex, blood pressure, weight, height, and relevant medical history. Body mass index was calculated from the individual's weight and height using the formula designed by the World Health Organization. The differences in group size are due to difficulties with participant selection and the exploratory approach of the study.
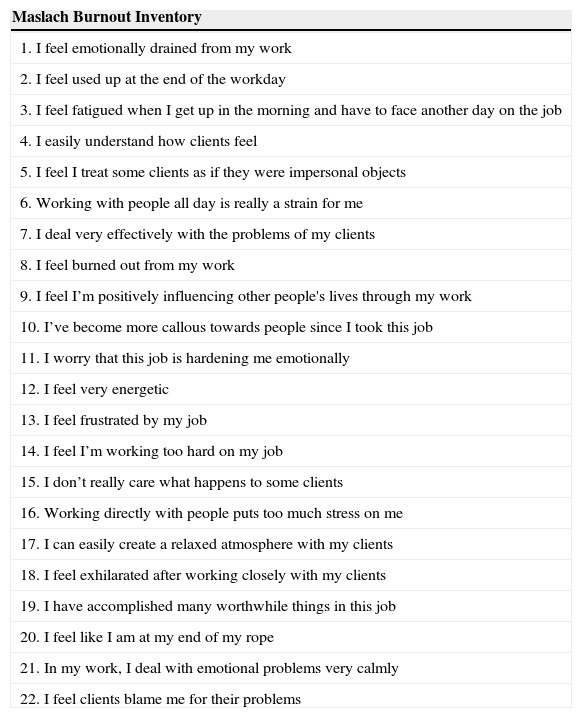
Professional exhaustion was measured using the Maslach Burnout Inventory (MBI),13,16 which is the most widely used and internationally accepted questionnaire for burnout assessment. The Spanish version of this questionnaire, adapted by Moreno et al. in 1991 and by Gil-Monte in 2002,13,17 includes 22 items that inquire about patients’ feelings and thoughts regarding several aspects of their normal job performance and interaction at work. Participants were asked to answer each item using a Likert-type scale with 6 possible response options, ranging from ‘never’ to ‘every day’ (Table 3). We used this version of the MBI questionnaire because it is the most widely used internationally, both as a tool for measuring burnout and as a model for validating other tools. This questionnaire presents the least intercultural variation, with validated results, an internal consistency coefficient of 0.80, and adequate convergent and discriminant validity. In addition to this, the last version (MBI-GS) is also applicable to non-healthcare occupations.18
Maslach scale
| Maslach Burnout Inventory |
|---|
| 1. I feel emotionally drained from my work |
| 2. I feel used up at the end of the workday |
| 3. I feel fatigued when I get up in the morning and have to face another day on the job |
| 4. I easily understand how clients feel |
| 5. I feel I treat some clients as if they were impersonal objects |
| 6. Working with people all day is really a strain for me |
| 7. I deal very effectively with the problems of my clients |
| 8. I feel burned out from my work |
| 9. I feel I’m positively influencing other people's lives through my work |
| 10. I’ve become more callous towards people since I took this job |
| 11. I worry that this job is hardening me emotionally |
| 12. I feel very energetic |
| 13. I feel frustrated by my job |
| 14. I feel I’m working too hard on my job |
| 15. I don’t really care what happens to some clients |
| 16. Working directly with people puts too much stress on me |
| 17. I can easily create a relaxed atmosphere with my clients |
| 18. I feel exhilarated after working closely with my clients |
| 19. I have accomplished many worthwhile things in this job |
| 20. I feel like I am at my end of my rope |
| 21. In my work, I deal with emotional problems very calmly |
| 22. I feel clients blame me for their problems |
Each item is scored using a Likert-type scale with 6 possible response options: never, a few times a year or less, once a month or less, once a week, a few times a week, and every day.
EE: 1+2+3+6+8+13+14+16+20; DP: 5+10+11+15+22; PI: 4+7+17+21; PA: 4+7+9+12+17+18+19+21.
The inventory is divided into 4 subscales, each of which assesses one of the 4 factors of burnout: emotional exhaustion (EE), personal accomplishment (PA), depersonalisation (DP), and positive involvement with others at work (PI). EE, assessed with 9 items, denotes fatigue or lack of energy and the feeling that one's emotional resources are depleted. PA is the feeling of lacking achievements at work including negative self-evaluation. This dimension includes 8 items. DP comprises 5 items and evaluates negative attitudes and insensitivity towards clients and colleagues, which leads to interpersonal conflicts and isolation. Positive involvement is assessed using 4 items. Scores from each one of these 4 subscales, considered continuous variables, can be low, medium, or high, measuring the degree of burnout.16,19
We stratified participants and measured the impact of headache using the HIT-6. We also determined the presence of depression and anxiety using BDI-II and BAI, and evaluated migraine patients using the MIDAS.
Statistical analysis was performed using SPSS software (version 15.0). The descriptive analysis included total percentage, mean, and standard deviation. We used the age-adjusted general linear model to compare the differences between clinical groups. Correlation coefficients between scores on BDI-II, BAI, MIDAS, and MBI subscales were obtained using the Pearson method. The Šidák correction for multiple comparisons was applied in all cases. We assumed a risk of 0.05 and calculated the sample size for a statistical power of 0.80, risk=0.05, and a difference between means of 25%. The necessary number of participants per group was 13. The sample size increased since multiple comparisons were made, especially in the patient groups.
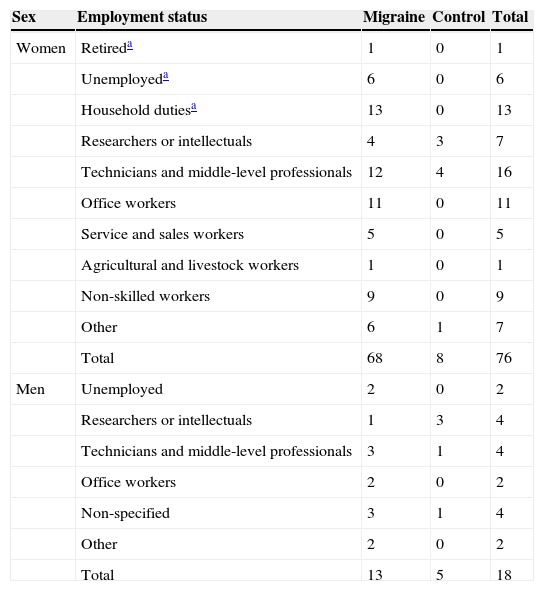
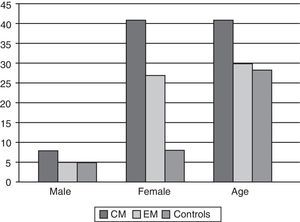
ResultsFrom the total of 94 patients, the CM group had a mean age [SD] of 41 [2.9] years, the EM group had a mean age of 29.8 [2.3] years, and the control group, 28.3 [7]. Patients in the EM group were therefore 11 years younger than those in the CM group, but no significant differences were found between the EM group and the control group (Fig. 1). The MIDAS test was administered to all patients with migraines. The mean scores (Fig. 2) were 51 [4.1] in the CM group and 17.7 [15] in the EM group (P=.001 for the difference between CM and EM). We also took into account the distribution of participants according to their level of education and job type, and we only included unemployed or retired patients with less than 6 months of inactivity to minimise bias. The breakdown of participants by job type is shown in Table 4.
Distribution of participants by job situation/type
| Sex | Employment status | Migraine | Control | Total |
|---|---|---|---|---|
| Women | Retireda | 1 | 0 | 1 |
| Unemployeda | 6 | 0 | 6 | |
| Household dutiesa | 13 | 0 | 13 | |
| Researchers or intellectuals | 4 | 3 | 7 | |
| Technicians and middle-level professionals | 12 | 4 | 16 | |
| Office workers | 11 | 0 | 11 | |
| Service and sales workers | 5 | 0 | 5 | |
| Agricultural and livestock workers | 1 | 0 | 1 | |
| Non-skilled workers | 9 | 0 | 9 | |
| Other | 6 | 1 | 7 | |
| Total | 68 | 8 | 76 | |
| Men | Unemployed | 2 | 0 | 2 |
| Researchers or intellectuals | 1 | 3 | 4 | |
| Technicians and middle-level professionals | 3 | 1 | 4 | |
| Office workers | 2 | 0 | 2 | |
| Non-specified | 3 | 1 | 4 | |
| Other | 2 | 0 | 2 | |
| Total | 13 | 5 | 18 |
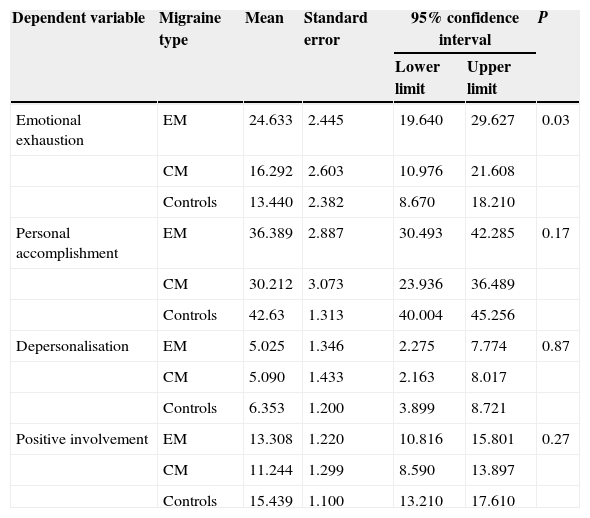
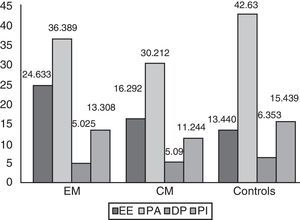
Using the model corrected for age, depression, anxiety, and MIDAS score, we compared the adjusted means for each MBI subscale. The adjusted mean of EE scores was 24.6 [2.6] in the EM group, vs 16.2 [2.6] in the CM group and 13.4 [2.3] in the control group (P=.03). The mean PA score in each of the groups was 36.3 [2.8], 30.2 [3.0], and 42.6 [1.3], respectively (P=.17). As for the third subscale in MBI, DP, the mean score was 5.0 [1.4] in the CM group, 5.0 [1.3] in the EM group, and 6.3 [1.2] in the control group (P=.87). Lastly, the mean score in PI was 11.2 [1.3] in CM patients, 13.3 [1.2] in EM patients, and 15.4 [1.1] in controls (P=.27) (Fig. 3). The most significant differences were observed between EE scores (P=.033) (Table 5). The total mean score on the combined EE and DP subscales was 29.662 in the CM group, 21.382 in the EM group, and 19.793 in the control group. High scores on these subscales indicate a strong feeling of burnout. The combined mean scores on the PA and PI subscales were 49.697 in the CM group, 41.456 in the EM group, and 58.069 in the control group. Low scores on these subscales reveal a strong feeling of burnout. These scores are considered continuous variables. Scores on each subscale were analysed separately and not combined to generate a single score since there is no evidence as to whether all subscales have an equal impact on the total score or to what extent they are more or less influential.
Mean scores on each of MBI subscales for each study group. Controls present lower levels of EE, stronger feelings of PA, and better interpersonal competence than migraine patients. EE: emotional exhaustion; DP: depersonalisation; CM: chronic migraine; EM: episodic migraine; PA: personal accomplishment, and PI: positive involvement.
Mean, standard error of the mean, and confidence interval for the 4 subscales in the Maslach Burnout Inventory
| Dependent variable | Migraine type | Mean | Standard error | 95% confidence interval | P | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Emotional exhaustion | EM | 24.633 | 2.445 | 19.640 | 29.627 | 0.03 |
| CM | 16.292 | 2.603 | 10.976 | 21.608 | ||
| Controls | 13.440 | 2.382 | 8.670 | 18.210 | ||
| Personal accomplishment | EM | 36.389 | 2.887 | 30.493 | 42.285 | 0.17 |
| CM | 30.212 | 3.073 | 23.936 | 36.489 | ||
| Controls | 42.63 | 1.313 | 40.004 | 45.256 | ||
| Depersonalisation | EM | 5.025 | 1.346 | 2.275 | 7.774 | 0.87 |
| CM | 5.090 | 1.433 | 2.163 | 8.017 | ||
| Controls | 6.353 | 1.200 | 3.899 | 8.721 | ||
| Positive involvement | EM | 13.308 | 1.220 | 10.816 | 15.801 | 0.27 |
| CM | 11.244 | 1.299 | 8.590 | 13.897 | ||
| Controls | 15.439 | 1.100 | 13.210 | 17.610 | ||
Comparison between clinical groups using the age-adjusted general linear model. We applied the Šidák correction for multiple comparisons and assumed a risk of 0.05.
CM: chronic migraine; EM: episodic migraine.
These results show that EM patients have a higher level of EE in the workplace than CM patients. Meanwhile, the PA is less favourable in patients with higher MIDAS scores. Conversely, higher levels of depression and anxiety were associated with decreased PA at work, regardless of the patient's clinical status (P=.001).
Additionally, we found a significant correlation between the level of depression (Pearson r=0.337; P=.003, regardless of clinical status) and anxiety (Pearson r=0.308; P=.023) for EE, as well as an inverse relation between level of depression and lower perceived PA (Pearson r=−0.440; P=.001). A higher education level was associated with higher PA at work (Pearson r=0.254; P=.040). Patients with more frequent CMs obtained higher scores on the BDI-II (P=.027). In any case, controls scored significantly lower on the BDI-II (7.080 points lower; P=.001 with Bonferroni correction). Regarding BAI, only patients with migraine with aura showed significantly higher scores than controls (12.7 points higher; P=.005 with Bonferroni correction). No significant differences were found between the 2 patient groups regarding the diagnostic categories of migraine with aura and migraine without aura. In addition, no significant differences were seen in BAI and BDI-II scores between the EM group and the CM group. However, both patient groups scored considerably higher than controls on the BDI-II (7.1 and 8.0, respectively; P=.006).
DiscussionThis study explored the potential applicability of the MBI on cohorts of patients with migraine not adjusted for job type. This tool is seeing increased use as a means of measuring burnout in different occupations, and its validity and reliability have been demonstrated in different contexts and professional groups. As a result, it can be administered easily to different types of neurological patients. Most studies have shown that MBI has an acceptable level of internal consistency.19,20 Our main findings underline its usefulness for headache research since it may help us understand the potential impact of disabling disorders such as migraine in the workplace.
As previous studies have shown, participants in both the CM and EM groups were predominantly female. The age difference between these 2 groups (EM patients were a mean of 11 years younger than CM patients) is consistent with published prevalence data: the highest prevalence rates of EM appear at ages of 30 to 40, whereas peak prevalence of CM is found approximately a decade later.21
With few exceptions, sex, body mass index, and blood pressure values were not indicative of significant variations in the interpretation of data from the CM and EM groups. The exception was age and the MIDAS scores, due to the differences previously mentioned.
An in-depth analysis of results on each of the MBI subscales shows differences in EE at work depending on migraine chronicity; EM patients are affected to a significantly greater extent. There are several possible explanations for this tendency. One plausible explanation would be the presence of an adaptation phenomenon. Adaptation, in patients with chronic headaches, would result in less EE in the workplace, accompanied by less pronounced fatigue. In contrast, these traits would be more marked in patients with a significantly lower headache frequency (the EM group). From a neuropsychological point of view, another plausible explanation would be the presence of a stress-induced adjustment disorder to migraine in EM patients: when an episode of migraine starts, patients show diminished coping skills and increased disability, which has a negative impact on professional life. Limited coping skills in EM patients, which is shown by their elevated EE scores, may be caused by different factors, the most interesting one being the sporadic nature of these episodes. However, and despite the level of anxiety these patients display, their scores do not show increased depressive tendencies: according to the other MBI scores, they display good personal and professional self-esteem, which underlines the temporary and sporadic nature of their episodes.
This curious adaptation phenomenon has never been described before, possibly due to the absence of studies aimed at determining the real impact of headache on the workplace and to the fact that most psychological tests administered to migraine patients have been used in EM patients exclusively, with only a few studies examining CM patients.22,23 The relevance of these findings also lies in the absence of other possible confounders, such as depression and anxiety, that may contribute to masking the results. Analysis of the rest of the MBI variables delivered a significant finding: migraine patients (both EM and CM) displayed lower levels of PA and PI towards their colleagues than did healthy controls. This finding evidences that migraine has a real and significant impact on patients’ professional performance that cannot be dismissed: it increases stress and makes completing daily tasks more difficult.
The possible association between migraine and the burnout syndrome must therefore be examined in depth. This close connection, represented by certain common and non-exclusive environmental factors, may point to the existence of a more profound causal relationship between both factors. However, further research is needed if we are to understand that connection.
Studies using the MIDAS questionnaire suggest that CM patients present a higher level of disability than those with EM. In these cases, productivity is more severely reduced. However, the mean number of lost working days and the mean MIDAS score vary greatly from one study to another. Differences between these studies may be due to the diversity of the study population or to retrospective data collection methods. In line with the published literature, this study shows that MIDAS scores are indirectly related to the degree of PA. Additionally, migraine chronicity was correlated with higher scores on the BDI-II and therefore with a perception of greater disability.24
Our study is the first to assess the connection between burnout syndrome and migraine types broken down by episode frequency. As a result, our findings, though significant, have some limitations. The age differences between the subgroups, while expected, may influence one or more of the study variables. The number of control patients was also limited due to the difficulty of finding patients without headache. Another limitation was the variety of job types, a consequence of recruiting consecutive patients seen in clinics. Future research must therefore consider patients’ job types in order to avoid biases that have not been contemplated by this study.
In conclusion, the level of burnout is higher in migraine patients than in healthy controls. We also emphasise that EM patients presented the highest levels of EE. The MBI is a useful tool for measuring the impact of migraines on patients in the workplace, and it shows that physical health and emotional problems may affect worker productivity. However, more detailed studies will have to show how these findings can be applied in daily practice in order to improve prognosis and facilitate comprehensive management for migraine patients that addresses social and work-related problems.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González-Quintanilla V, Toriello-Suárez M, Gutiérrez-González S, Rojo-López A, González-Suárez A, Viadero-Cervera R, et al. Estrés laboral en pacientes migrañosos: diferencias según la frecuencia de las crisis. Neurología. 2015;30:83–9.
Part of this work was presented at the Annual Meeting of Lasén 2011.